Article: A. Franke and E. Kollig
Recommendations for the treatment of severe burn injuries in the field
Owing to the increasing incidence of severe burn injuries caused by enemy action in current operations of the German Armed Forces (Bundeswehr), a recommendation on how to manage in an operational environment has been prepared for the Bundeswehr Advisory Group of Surgical Consultants. In this article, the most important treatment parameters are highlighted with particular emphasis on potential pitfalls.
Owing to the increasing incidence of severe burn injuries caused by enemy action in current operations of the German Armed Forces (Bundeswehr), a recommendation on how to manage in an operational environment has been prepared for the Bundeswehr Advisory Group of Surgical Consultants. In this article, the most important treatment parameters are highlighted with particular emphasis on potential pitfalls. Our findings reflect the experience that we have gained in the burn intensive care unit of the Central Military Hospital of the Bundeswehr in Koblenz and the specific injury patterns that we have seen in the past. The complex field of burn medicine, however, has made it necessary for us to divide this subject into two separate parts. The first part is presented here and focuses on initial care and stabilisation. The second part will follow and will address the transportation as well as the further surgical and intensive medical care of burn patients. In our opinion, the current reality of Bundeswehr operations and the particular challenges of treating severe burn injuries make it absolutely essential that the management of severely burned patients remain one of the prominent services provided by the Bundeswehr Medical Service. Whenever possible, treatment of severely burned soldiers should be performed in one of our military hospitals not only in order to use the existing expertise but also to maintain this expert capability, or in comparable civil burn units.
Introduction
In view of the menacing diversity of forms of assault used in asymmetric warfare and the growth in terror attacks, a resilient and realistic concept for the initial treatment and stabilisation of casualties with combined thermodynamic injuries needs to be developed as the basis for medical support in the field provided as part of the military rescue chain. The type of injuries more commonly associated with mechanised warfare are becoming less frequent while blast injuries resulting, for example, from exposure to IEDs and suicide bombers are now predominant.
A component of all combined thermodynamic injuries (CTIs) is a burn injury to soft tissue, mainly involving the integumentary system and the lungs. The subsequent course will be determined primarily by the extent and depth of this damage. If the explosive device was supplemented with combustive agents, it is likely that the victims will suffer extensive burns.
Because of the other injuries caused by explosives (inhalation burns, pulmonary blast injuries, contusions to larger areas of soft tissue), the status of burns victims in the field rapidly becomes critical or even acutely life-threatening. Our experience to date shows that the specific requirements for the treatment of burns casualties while on deployment abroad and the resulting consequences for the primary treatment and stabilisation (to repatriation) of victims with thermomechnical wounds are not taken adequately into account in the training provided while insufficient expertise is provided on the ground – the “be prepared” mentality seems to be lacking.
We have written this article on behalf of the Bundeswehr Surgery Consultancy Group with the aim of providing basic advice for the treatment of service personnel with burns injuries in the field. The article highlights the main treatment parameters and draws particular attention to potential pitfalls. We have also included information drawn from our own experience to date of dealing with the characteristic trauma profiles that can be expected.
As this is necessarily a complex subject, this article will appear in two parts. In this first part, we will be looking at the pathophysiological aspects and the forms that initial care should take. The second part will follow and will address the subsequent course of burns injuries, transport, further surgical treatment and the associated intensive care requirements.
We hope that our observations here will provide all those working in related medical disciplines with a useful guideline for the provision of interdisciplinary treatment in the field, with the proviso that our article is not intended to represent an exhaustive review of the subject.
Part 1: Initial care and stabilisation
The severity and prognosis of injuries
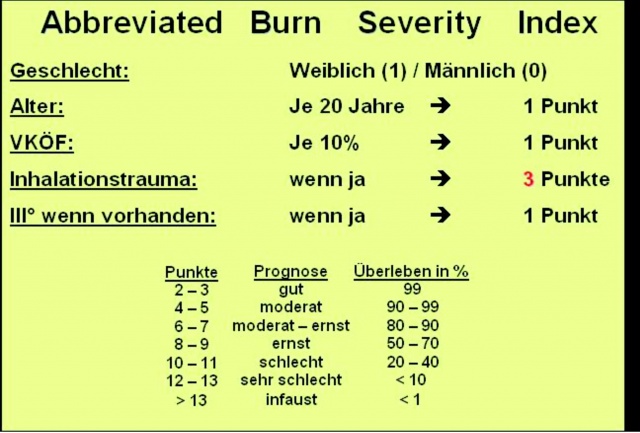
The prognosis and threat to the life of a casualty on admission will be determined by the presence of the trauma triad of death (hypothermia, acidosis and hypoxaemia) and the severity of any burn injury. When assessing the burned body surface area (BBSA), it is advisable to include all areas of at least second-degree burns (II a). The modified version of Tobiasen’s abbreviated burn severity index provides an indication of the risk of mortality of the patient, taking into account factors such as the additional presence of inhalation trauma (IHT), age and gender of the casualty.
With its total area of some 1.8 m2, the skin is the largest human organ. It consists of three main layers that are made up of different kinds of cells and have differing functions. Keratinocytes constitute by far the largest component of the epidermis (97%), and provide protection against mechanical stresses and infection. There are very few pathogens that are capable of penetrating across the intact epidermis.
Thanks to the proliferation of the basal keratinocytes, the epidermis is constantly renewed. This means that there are no negative consequences if the basal cells remain unharmed following an injury to the epidermis. The fibroblasts of the dermis enhance the protective mechanisms of the skin and make it elastic. Collagen and flexible fibres form the framework of its extracellular matrix.
The dermis contains a wealth of blood vessels and nerve endings that supply the epidermis and provide for the skin’s sensitivity. Hair follicles and the sweat and sebaceous glands are located in the lower dermis. This is important, as only these cells have the ability to proliferate and rebuild the epidermis. The other elements in the dermis are not capable of regeneration. When these are damaged, a scar remains, and the size of any such scar will be determined by the extent and depth of the original lesion. The subcutis contains adipocytes and connective tissue, and allows the skin to glide and flex. The blood vessels and nerves pass through this layer. The subcutis also protects the tissues immediately below it.
Any severe damage to the skin will result in, among other things, the loss of the immune barrier and the disruption of homoeostasis in the affected area. This will be accompanied by the continuous, systemic release of mediators that is characteristic of the clinical picture in burn victims.
With these factors in mind, calculation of the ABSI score (see appendix) for a 40-year old soldier (2 points) with second- to third-degrees burns (1 point) affecting 40% of BSA (both legs, 4 points) and pulmonary blast or inhalation trauma (1 – 3 points) show that he would have an approximately 50% chance of survival – but only if effective first response treatment is provided and definitive treatment is rapidly made available in a burns centre.
Depth of burns
The depth of a burn will be determined by the temperature causing the injury and the duration of exposure. It has been demonstrated that cell damage can result, with release of oxygen radicals, even after exposure to a temperature of 45°C for more than 1 hour. Very serious damage to tissue can occur in a fraction of a second when there is exposure to the combustion gases created during an explosion, which can reach temperatures of up to 2000°C.
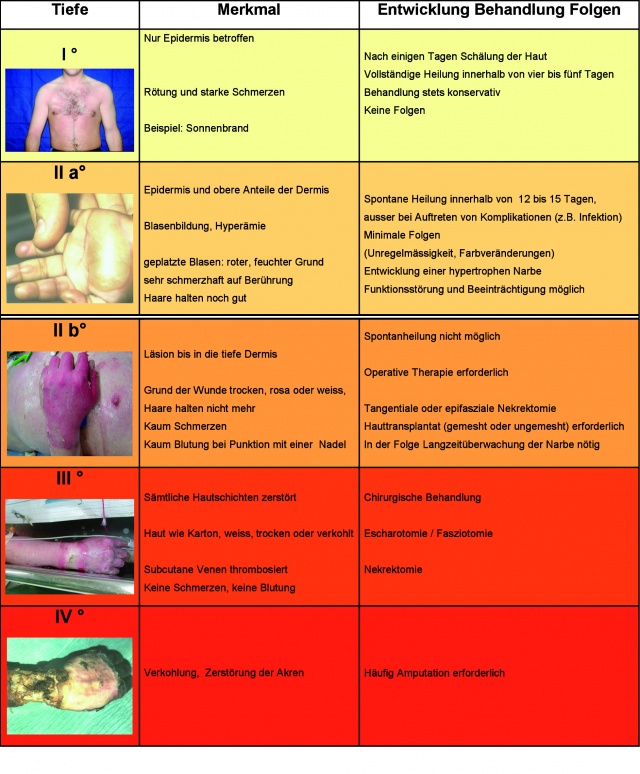
In the system we use, we classify the depth of a burn injury using four categories. While the regeneration capacity of the skin is retained in burns that are no severer that superficial, second-degree burns (II a) and any injury will spontaneously heal if conservative treatment is provided, there will be limited or no healing of burns that are more severe (II b) and extensive scarring will result if there is no surgical intervention. This is the case when there is damage to the lower layers of the dermis. The cells of the skin appendages of ectodermal origin are then dysfunctional and unable to rebuild the epidermis due to their deficient proliferation capacity.
The clinical effects of a deep, second-degree burn (II b) involve the loss of hair in the affected skin regions, which is generally accompanied by hypaesthesia or even total analgesia here, and there will be no bleeding when the relevant skin is punctured with a fine cannula. An overview of our burns classification system is provided in Fig. 2.
Percentage of burned body surface area (BBSA)
It is generally advisable to take into account areas of second- and third-degree burns only when assessing the extent of burn injuries. Wallace’s “Rule of Nines” is a useful aid for obtaining a quick, relatively accurate estimate of BBSA in adults. A more precise method is the “Rule of the Palm”: the palmar surface area of a patient is equivalent to 1% of that person’s total body surface area (Fig. 3).
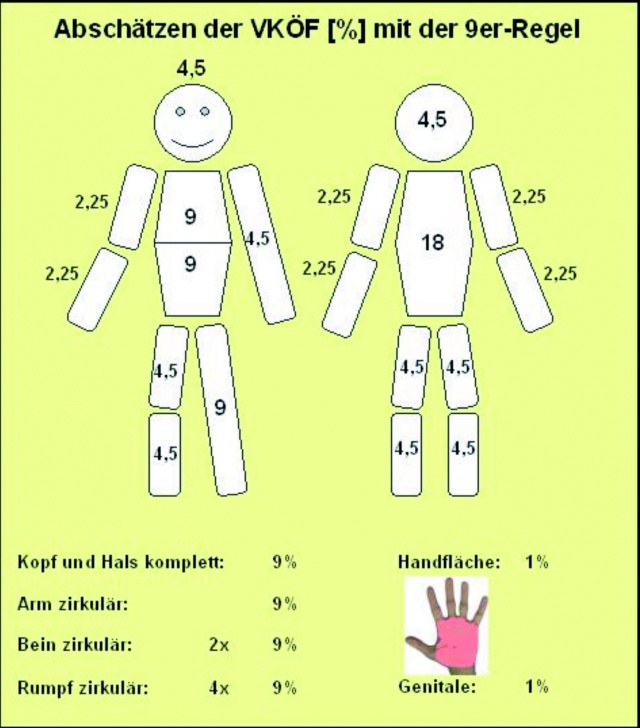
The Rule of Nines cannot be used in the case of children because of the different body proportions.
Experience shows that the surface extent of a burn injury is frequently overestimated, while the depth of such an injury is often underestimated. This means that it is essential to accurately and reliably document initial status and to regularly evaluate status when renewing dressings. The use of catecholamines (epinephrine and norepinephrine) to treat burn shock and/or excessively restrictive fluid replacement therapy in the first 24 hours following initial injury can mean that a burn that has been assessed as being of a lower degree can be exacerbated. This potential complication must be taken into account when the therapeutic goals and priorities are set at the commencement of treatment.
Inhalation injuries
During the preliminary assessment of severe burn cases, the aspect of inhalation trauma (IHT) is often not accorded the importance it deserves. IHT is the main cause of mortality in 80% of the cases that succumb at the site where the injury was incurred and is diagnosed in 25% of severe burn patients surviving at the time of delivery to a trauma unit. Its influence on prognosis is both beyond dispute and fundamental. In the field, IHT can double the mortality rate of casualties with burns. It is necessary to distinguish between thermal and toxic inhalation trauma, and both can occur in combination.
The inhalation of hot gases results in thermal and chemical damage to the epithelium of the airway passages and to carbon monoxide (CO) and, less commonly, cyanide compound intoxication. When a patient is conscious, reflex closure of the glottis will normally prevent hot gases and combustion residues passing into the lungs. However, inhalation of hot particles (aerosols, dust etc.) is quite possible in the context of explosion injuries.
There are many types of combustion gases that can damage the mucous tissues of explosion or burn victims. The result will be the development of local oedema in the airways, bronchospasm, loss of the protective surfactant film, atelectasis and toxic pulmonary oedema. The effects of lipophilic substances (such as phosgene) are predominantly observed in the lower airways, while hydrophilic substances (such as NH3) generally cause laryngopharyngeal symptoms.
Toxic compounds are formed during conflagrations in confined spaces and in burning vehicles. If these are inhaled, they can lead to medium to long term pulmonary damage. The risk of mortality or permanent injury is high, similar to the risk that unprotected soldiers faced when faced by gas attack in the First World War, when phosgene was used.
As a result of the fact that the mucous membranes exhibit a relatively higher thermotolerance than other tissues, direct heat-related damage is usually confined to the supraglottal region. Peri- and intraoral burn injuries rapidly result in oedematous transpositioning of the airways, particularly if volume replacement therapy has been provided, often making orotracheal intubation difficult if not impossible.
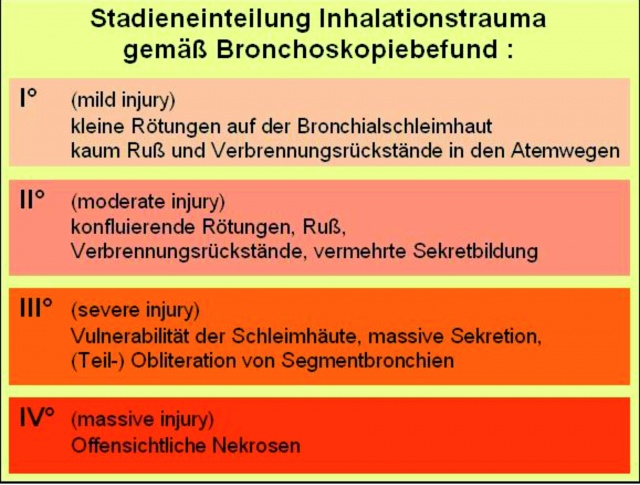
Clinical signs indicative of an inhalation trauma are fuliginous sputum, burned eyelashes and nasal hair, facial burns, chemosis, enoral combustion residues, coughing, hoarseness, dyspnoea, inspiratory stridor and bronchospasm (Fig. 4).
Where there is clinical evidence of the presence of IHT, the indication for intubation needs to be liberally interpreted (“in dubio pro tubo”); in extreme cases, a surgical access may need to be created (cricothyrotomy or tracheotomy, e.g. using the Quicktrach kit).
Bronchoscopy should be performed at the earliest possible time point at the first facility equipped for this and the results should be documented. In addition to its diagnostic purposes, it can also be used to rapidly remove any accessible combustion residues by means of bronchoalveolar lavage (BAL). The degree of any inhalation trauma is classified in accordance with the results of bronchoscopy (see Fig. 5 for an overview).
Once the presence of IHT has been confirmed, it should be borne in mind that there is the risk of development of toxic pulmonary oedema (in the form of acute lung injury, ALI) within the initial 72 hours following injury, and of protracted acute respiratory distress syndrome (ARDS) during the subsequent course (in weeks 1 – 4). Priority should be given to the provision of pulmonary protection and oxygenation/decarboxylation when planning the therapeutic regimen.

Combined thermodynamic injuries
Because explosion injuries (primary to quaternary injuries) are caused by a range of mechanisms, there are not just the skin burns resulting from exposure to high temperatures to be taken into account - these are also accompanied by the effects of the direct and indirect kinetic energy released by the blast. These direct and indirect forces generally cause contusions over the whole body of differing depth and extent and can result in bone fractures. In cases of combined thermodynamic injuries, superficial injuries may appear slight but, at the same time, all internal body compartments will have suffered extensive trauma due to the sudden transitions in internal or external pressure and the direct and indirect effects of other forces. The perfusion of these injured deep muscle and tissue regions results in local and systemic immune reactions that potentiate the symptoms associated with burns. Patients also develop capillary leak syndrome, which can predispose them to compartment syndrome in the extremities.
The above indicates how important it is both to sufficiently stabilise any fracture as soon as possible by means of external fixture in burns regions (even if only crudely and without excessive concern for anatomical alignment), and to liberally interpret the indication for fasciotomy in order to preserve extremities and their functions.
Burns and their consequences
Burn shock, which occurs in the initial 12 hours, is essentially volume-deficiency shock. It is characterised by local impairment of capillary permeability in the affected areas and local release of mediators, such as cytokines, leukotrienes, histamine, oxygen radicals and prostaglandins. When they occur systemically, these messenger substances are indicative of the presence of systemic inflammatory response syndrome (SIRS). In patients with burns to more than 20% of their BSA, the associated capillary leakage also occurs in body regions that have not been burned. The result is the escape of proteins with a molecular weight (MW) of up to approximately 350,000 into the extravasal space. As there is a simultaneous loss of water due to the osmotic effect, there is transfer of isotonic plasma into the tissues. At the same time, there is elevation of extravascular osmotic pressure as small molecular weight substances are released from damaged tissue and sodium combines with damaged collagen. The upshot of this is the extensive formation of interstitial oedema.
There is pathological adhesion of leukocytes and erythrocytes to each other and to vascular walls, further impairing the microcirculation. Reduction of cell membrane potential in burned and non-burned tissues leads to the accumulation of intracellular sodium and thus to cellular oedema, and the associated massive cytolysis can cause severe hyperkalaemia. Generalised oedema becomes clinically apparent within 2 – 3 hours of the trauma event and peaks after 12 – 24 hours. Reabsorption occurs as the result of enhanced lymph outflow and the reestablishment of the physiological capillary barrier, a process that commences some 24 hours after the trauma event and which promotes the restoration of physiological colloid osmotic pressure.
Hence, all that is required in this context in the first 24 hours after the trauma event is adequate replacement therapy using crystalloid infusion solutions to offset losses. As capillary leakage can also occur in the lungs in patients with extensive burns, pulmonary protection and maintenance of positive end-expiratory pressure (“Keep the PEEP”) are relatively significant in patients receiving controlled ventilation. It is necessary to maintain a high PEEP in patients with CTI because of the systemic effects on haemodynamics.
Triage of burns victims in mass casualty situations
On the German side, we have to date experienced one situation involving mass casualties in the field (MASCAL) with combined thermomechanical injuries. This fortunately occurred against a background of a relatively favourable constellation with regard to transfer options and transport distances (attack on a bus taking personnel to the airport for a flight home in Kabul in 2003).
Following 2003, there have been occasions in which only one or two cases of severely wounded German ISAF personnel with combined thermomechanical injuries have arrived for treatment, so that our medical rescue centres were able to provide optimal individualised care to these in the relatively short periods until they could be repatriated (within a maximum of 48 hours).
The care of patients with severe burns represents a major challenge for the first links in the rescue chain. Available resources are rapidly expended during their treatment - initially infusion solutions, centrally acting analgesics and dressings. Personnel and equipment soon also need to be dedicated specifically to the treatment of patients, who are often already in need of intensive care on arrival. In a MASCAL situation involving a larger number of severely wounded personnel with burns or combined thermomechanical injuries, a rescue centre will be stretched to full capacity with the arrival of the second patient within the first 24 hours.
This means that if a situation arises in practice in which more than two patients requiring intensive care are delivered to the same rescue centre and immediate air transport to a less heavily engaged medical facility in the country of deployment is not available, early and systematic triage becomes essential.
In MASCAL situations, lower priority should be afforded to cases with more than 40% BBSA or more than 20% BBSA with accompanying inhalation trauma. Even in circumstances in which optimal provision of individual and intensive care is possible, statistics show that survival can only be achieved in 50% of such cases.
At the rescue centre, the subsequent strategy to be adopted will be determined by the number of casualties and the severity of their injuries, the presence of other casualties, and the availability of personnel and of the means and options for transfer and repatriation.
Phases of treatment of a burns patient
There are generally different phases of treatment of a burns patient. As a chronological guideline, these can be associated with the various treatment days. The primary phase commences with the water day. These first 24 hours are used for adequate volume replacement therapy in order to stabilise the patient and preserve their organ functions. The second day (24 – 48 hours following the trauma event) is the protein day, during which balance and oncotic pressure are re-established. From day three (surgery day), surgical intervention is possible, assuming that general status allows this and homeostasis has sufficiently normalised. Day four (> 72 hours) is nutrition day. The appropriate supply of calories can now commence following the remission of any perioperative stress reaction.
In our experience, the individual care of a severely burned casualty in the field is subject to a number of limiting factors. The spectrum of what is possible in this context stretches from initial life-saving and extremity preserving measures followed by immediate transfer to another medical unit through to longer admission of the patient, involving stabilisation and treatment over the initial 72 hours, and then subsequent transfer or repatriation.
The following recommended treatment schedule is appropriate to the more extensive requirements for the care of one to two patients with CTIs and in cases in which transfer to another facility is delayed.
It is not possible to provide detailed advice for the procedure in MASCAL situations. The imponderables of these special circumstances are so multifaceted that the decision can only be made on an ad hoc basis with reference to the actual state of affairs. This applies in particular to the requirement for early triage and its consequences.
Deviations from and modifications to these guidelines may become necessary depending on what options and resources are available; the art of improvisation in the field is a capability that is as valuable as it is vital.
Initial treatment by the mobile field physician
The mobile medical team should not forget to ensure its own safety is assured before going in and during treatment of a burns victim – only a secure and uninjured team can provide the best level of treatment. For treating a patient with extensive burns, it is generally possible to adopt the procedures of, for example, the Pre-hospital Trauma Life Support (PHTLS) and Advanced Trauma Life Support (ATLS) concepts. Where there are combined thermomechanical injuries, the ABCD protocol for field medicine should be modified to a C-ABCD approach (“stop the bleeding”) in order to prevent any life-threatening loss of blood (“treat first what kills first”).
There are both advantages and disadvantages to cooling the burned skin regions. There is no doubt that cooling alleviates pain. However, it is only possible to avoid “afterburn” if cooling can be applied immediately after the injury. If 15 – 20 minutes have already elapsed, cooling has no benefit. There is also the risk that excessive cooling of larger areas (20% BSA or more) for longer periods could result in iatrogenic hypothermia with all its pathological consequences (“Cool the wound but warm the patient”). The best cooling agent has proved to be clean water. It is neither appropriate nor advantageous to waste sterile infusion solutions for this purpose. The use of special topical agents, such as tea tree oil, during first response can also not be recommended; results of their use to date are negative. The cooling procedure should on no account be allowed to delay recovery and transport of the patient; cooling can be provided en passant.
Systemic capillary leakage means that the fluid requirement of such patients is considerably greater than that in “normal” polytrauma cases. Patients with burns also become more rapidly hypothermic, which places their core temperature at risk. The longer times required for primary transport in the field in comparison with civilian scenarios also need to be borne in mind and appropriate measures taken.
It is advisable to use Ringer’s solution or a balanced electrolyte solution for infusion. As in the case of polytraumatised patients, the risk of inducing iatrotrogenic lactate overload also needs to be avoided. In view of the permeability of the endothelium in capillary leak syndrome and eventual reabsorption, the use of colloid volume replacement solutions is not recommended.
At least two large calibre accesses should be created during first response treatment. Areas on limbs with second-degree (II a) burns can be used for this purpose. Any accesses created on the hand surface, which will generally be moist, need to be appropriately secured, using sutures if necessary. Where it is difficult or impossible to create a peripheral access, intraosseous infusion is a viable alternative. Analgesia needs to be provided at an early stage following the standard guidelines for emergency treatment. Opioid monoanalgesia has proved to be effective, as has the combination of an opioid with titrated ketamine/midazolam. Following the physical examination and initial procedures, the casualty should be protected to prevent the development of hypothermia. Complex dressings are not necessary; wounds can be effectively covered using a large dressings pack, and these will be held in place when the patient is wrapped in a rescue blanket. If a patient with a combined thermomechanical injury (CTI) also has injuries to extremities, these should also be immobilised using splints or other measures in a neutral position. Conventional dressings can be applied to mechanically generated wounds. Depending on the ambient temperature and the exposure level (wind chill), additional insulation layers may be needed (wool blanket, poncho, sleeping bag).
A summary of recommendations for primary treatment by the first responding field physician is provided in Fig. 6.
Casualty admission – shock room management
In situations in which is it possible to send advance notification of the arrival of a burns patient, specific preparations can be made for the reception of the casualty. As casualty transport generally takes longer in the field than in the homeland, there is an increased risk that patients can develop hypothermia.
Room temperature in treatment rooms should be increased by adjusting the air conditioning system or any heating system and crystalloid infusion solutions should be pre-warmed in sufficient volume. If there is adequate time, the proposed treatment approach can be reassessed within the team. It is advisable to ensure that everything will be documented beforehand using a checklist (Fig. 7).
Following admission of the casualty to the shock room and referral of the case by the mobile field physician, vital parameters should be evaluated. ATLS parameters should also be reviewed and an abdominal ultrasound scan performed if the patient has a CTI. The wound coverings should be removed from burns for this purpose, leaving any dressings on open wounds in place. If patient respiration is insufficient, intubation should be performed at this point at the latest (“in dubio pro tubo”).
If the intravenous accesses created during first response are insufficient or appear inadequate, a central venous access sheath can be inserted and an arterial access created. Assuming there is no burned tissue in the inguinal region, it is advisable to create these accesses here.
Urinary bladder catheterisation (“everyman’s Swan-Ganz catheter”) is essential so that diuresis can be monitored. Volume therapy should be continued using Ringer’s solution in accordance with calculated volume requirement. In casualties with CTIs and extensive soft tissue contusions, continuous infusion of a sodium bicarbonate solution should be considered for the purposes of prophylaxis of renal crush syndrome (see below: Aims of intensive care).
If the patient is stable, further diagnostic procedures can now be performed; in a rescue centre this will take the form of conventional radiology. If a CT apparatus is available, a spiral scan can be performed to evaluate trauma. If the patient is not stable, a quick check in the form of x-ray of the thorax and lateral x-ray of the cervical spine is advisable. If this is appropriate in view of the nature and severity of any accompanying injuries, the casualty can now be transferred for damage control surgery to the theatre or intensive care unit.
A summary of the recommendations for shock room management procedures is provided in Fig. 8.
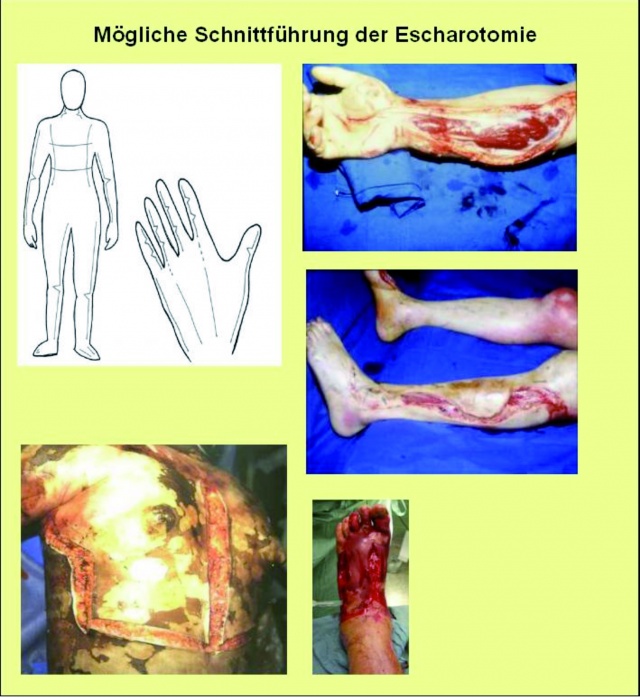
Surgical management of casualties with burns
If there is nothing more than a thermal lesion to the integument, the burned tissues can be removed by lavage with an antiseptic solution. Detached skin and any larger blisters should be removed by means of debridement. Where burns are causing constriction, escharotomy needs to be performed to ensure that blood circulation is maintained or restored. This may also be necessary on the thorax and abdomen for the purpose of respiratory excursion and on the neck to prevent congestion. The recommended techniques are shown in Fig. 9.
The new dressings on the burned areas should be applied in combination with an antiseptic; we have found PVP-iodine and silver sulphadiazine-moistened dressings to be effective. Alternatively, dressings can be steeped in an aqueous antiseptic preparation, such as octenidine HCl.
Early necrotomy of extensive burned tissues with use of temporary synthografts or autologous skin grafts is of little value in the field. The potential advantages of the avoidance of this procedure outweigh possible risks, while this also means that limited resources are spared.
In the presence of CTIs, surgery needs to be prioritised according to the severity of each trauma and its associated threat to the patient (“Treat first what kills first”).
In patients with life-threatening injuries to their thorax or abdomen following blunt or penetrating trauma, DCS must be given absolute priority. When surgical incisions need to be made, no consideration should be given to avoiding burned areas.
External fixation of unstable fractures to the extremities has proved to be the most effective strategy. Restoration of anatomical alignment is not required; all that is necessary at this stage is rapid and rudimentary fixation to provide adequate stabilisation. Shortening can even be of advantage in the case of shaft fractures where the soft tissue situation is compromised. A splint should be positioned with a view to subsequent permanent fixation. Splints should be mounted across fractures in the region of joints or that involve joints to hold the limb in a functional position. In every case of wounds to the extremities, the presence of compartment syndrome needs to be excluded as a matter of urgency. If the presence of compartment syndrome is confirmed, dermatofasciotomy must be used for the decompression of all compartments of the limb segment irrespective of the extent or severity of burns in the affected region. Dermatotraction can also be used for closure of burned skin edges without applying undue stress. Higher grade soft tissue injuries should be treated systematically, but without ultraradical debridement. Where there is vascular damage, the procedure needs to be adapted to the local and systemic status of the casualty and the actual situation (MASCAL). If there is absolute ischaemia of a terminal vessel, an ad hoc decision needs to be made on whether revascularisation is indicated or possible (even a drainage tube can serve as a rudimentary form of vascular bridge) – in any case of doubt, however, always follow the precept “life before limb!” The relevant evaluation scores used to determine whether a limb can be preserved or not have proved to be of limited value in battle and field medicine; the decision should be made in context and on an individual basis.
The management of defects remaining after debridement has been markedly facilitated in recent years thanks to the introduction of the technique of vacuum-assisted closure using wound sponges. Alternatively, dressings soaked in aqueous antiseptic preparations or synthografts can be used. The technique of primary closure of penetrating (explosion/shotgun/splinter/shrapnel) wounds suffered in the field has become obsolete. The risk of contamination is diametrically opposed to this, particularly in view of the possibility of infection with anaerobic pathogens and the multi-resistant bacteria that are often encountered in the field. We have found silicon drainage tubes, such as the Easyflow, to be of particular benefit in treating shrapnel, shotgun and penetrating injuries.
The risk of exacerbating hypothermia in the patient must be borne in mind in connection with all surgical procedures.
Burns dressings should be replaced after 24 hours; unless there is a reaction to a secondary compartment syndrome, there should be no further surgical intervention. A second look at other injury entities is only necessary if genuinely indicated, ideally this should be left until the patient has been repatriated to the intended hospital.
Our recommendations for surgical management of burns and CTIs in the field are summarised in Fig. 10.
Aims of intensive care
In cases where BBSA is 20% or greater, generalised oedema can be expected to develop even if the patient is young and was healthy prior to receiving the injury. The capillary leak syndrome associated with burn shock results in excessive loss of protein-rich fluids to the interstitial space and from burn wounds. To date, it has not proved possible to directly influence capillary leakage. Leakage will persist for the first 24 hours, and oedema will develop, the extent of which will also be dependent on the replacement therapy provided. It is necessary to ensure that this fluid is subsequently mobilised and reabsorbed. For this reason, it is advisable to refrain from the administration of any colloid volume replacement solutions during this initial 24 hour period as it is postulated that slowly metabolised molecules (gelatin, hydroxylethyl starch, albumin) have an oncotic effect in the interstitium, preventing or at least prolonging the reabsorption of water.
Among all the various concepts and formulae that there are for volume replacement therapy, we would recommend use of the Parkland-Baxter formula which is also routinely employed at many burns centres in Germany:
4 ml (6 – 9 ml) x kg bodyweight x % BBSA
of which 50% to be administered in the initial 8 hours
Only BSA with severer second-degree burns (> II a) should be used for calculation. The target for volume replacement therapy is spontaneous diuresis of 0.5 – 1 ml/kg bw/hour. If target diuresis is not achieved using the calculated infusion volume, it should be correspondingly increased (500 – 1000 ml Ringer’s as bolus). If an inhalation trauma has already been diagnosed, the volume infused should be carefully adjusted with a view to pulmonary function (catecholamines? – see above). In cases of combined thermomechanical injuries resulting in extensive destruction of muscle tissue, volume replacement therapy should be supplemented by early and mild alkalinisation of urine by means of continuous drip infusion of an 8.4% sodium bicarbonate solution (10 mval/hour). The additional CO2 load can be offset by means of the provision of adequate ventilation. Mild alkalinisation of the urine promotes the elimination of protein fragments and metabolites from the damaged tissue and prevents accumulation of these proteins in the renal glomeruli and tubuli. This is particularly advisable if there is a risk of myoglobin accumulation, which can result in renal failure as a consequence of tubular necrosis.
We consider it doubtful that use of catecholamines during these first 24 hours to increase peripheral resistance is of benefit. Although it is possible to reduce volume requirement by means of continuous infusion of norepinephrine, this results in reduced perfusion of damaged tissue regions and can result in exacerbation of burns injuries.
As fine titration of catecholamine therapy by means of monitoring with a PiCCO device or Swan-Ganz catheter is not practicable in the field, diuresis is the only relevant parameter that can be used to assess perfusion. Administration of catecholamines is advisable if the major proportion of burns is more severe than second-degree (> II b) and there is accompanying inhalation trauma. In this context, it is easier to maintain pulmonary function in the presence of a restrictive fluid regimen using controlled administration of catecholamines (see also Fig. 11).
Prophylactic use of antibiotics to prevent burn wound infection is not indicated. No special steps need to be taken to prevent bacterial contamination of burned areas; any infection will prove problematic for the patient only after 3 – 5 days. Non-targeted use of antibiotics in situations in which the potential infecting agents are unidentified is both counterproductive and unnecessary. The therapeutic indication is quite different if the patient has penetrating injuries: here the use of a second generation cephalosporin in combination with a anti-anaerobic agent (such as metronidazole) can be recommended.
If the patient is likely to require ventilation support for a longer period after repatriation because of trauma load, the creation of a tracheostoma should be considered prior to transfer (e.g. during surgical procedures). However, avoid this in the presence of fractures of the cervical spine so that the subsequent surgical treatment of these is not complicated.
If repatriation is possible within 24 – 36 hours of initial treatment, there is no need to consider the requirement for initiating artificial nutrition in the field situation. If this time window is likely to be postponed for 48 – 72 hours, hypocaloric parenteral nutrition may need to be commenced. It is also advisable to initiate enteral nutrition at a rate of 10 ml/hour via a nasogastric/duodenal tube in order to protect enterocytes.
All diagnoses and treatments provided must be documented in detail so that the subsequent treating physician(s) have all necessary information. If rapid contact is made with the homeland by means of telephone or telemedicine facilities, bidirectional information exchange is possible and additional expert help can be obtained.
Dept XIV Orthopaedic and Accident Surgery
[Medical Director: Major Priv. Doz. Dr. E Kollig] of Koblenz Bundeswehr Central Hospital
[Senior Consultant: Brigadier General Priv. Doz. Dr. G. Mager]
By A. Franke and E. Kollig
Contact author for list of references.
Contact details of author: Dr. Axel Franke, Major, Bundeswehr Central Hospital Koblenz, Dept. XIV Orthopaedic and Accident Surgery, Rübenacher Str. 170, 56072 KOBLENZ
Email: dr. axel.franke@t-online.de
Date: 11/01/2011
Source: MCIF 4/´11