
Article: M.C.M. Bricknell, A.G. Johnson (UK)
Forward Medical Evacuation
This paper discusses the principles of medical evacuation planning and execution with specific consideration of the command and control arrangements for Forward medical evacuation. The current operational context has focused efforts on helicopter medical evacuation as the main evacuation element of the pre-hospital military medical care system rather than the ground ambulance. This paper complements the significant number of papers recently published by RAMC clinical staff on pre-hospital care.
‘right patient, right platform, right escort, right time, right destination’
Introduction
Medical Evacuation is absolutely central to any military medical support system. This paper discusses the principles of medical evacuation planning and execution with specific consideration of the command and control arrangements for forward medical evacuation. The current operational context has focussed efforts on helicopter evacuation as the main element of the pre-hospital military medical care system rather than ground ambulance [1]. There are occasions when the tactical situation prevents helicopters reaching the casualty and thus the casualty will have to be moved by ground ambulance to a safe location for a helicopter landing site. Furthermore, ground medical evacuation is essential for moving significant numbers of casualties in a large-scale warfighting scenario. However this paper will not consider ground medical evacuation nor Tactical Aeromedical Evacuation, the movement of patients between medical facilities within a theatre of operations.
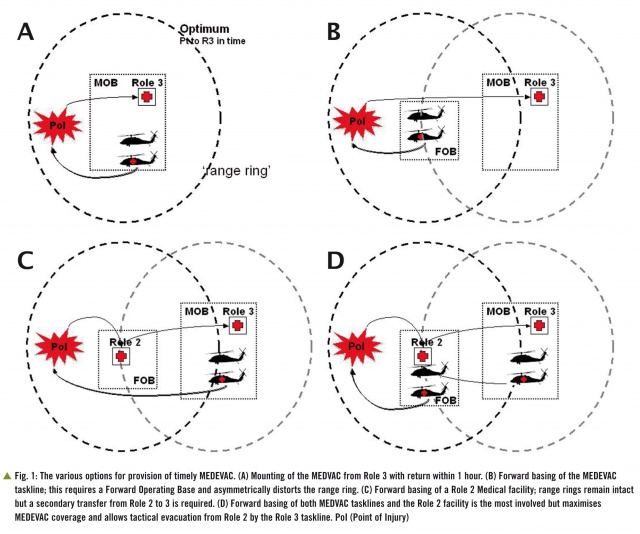 Fig. 1 shows the range of options for laying out medical facilities and MEDEVAC tasklines. Two aircraft are shown for the MEDEVAC taskline, the MEDEVAC aircraft and the accompanying chase aircraft that provides intimate force protection, particularly during the hazardous recovery of the casualty from the Point of Injury (PoI).
Historical Perspective
Fig. 1 shows the range of options for laying out medical facilities and MEDEVAC tasklines. Two aircraft are shown for the MEDEVAC taskline, the MEDEVAC aircraft and the accompanying chase aircraft that provides intimate force protection, particularly during the hazardous recovery of the casualty from the Point of Injury (PoI).
Historical Perspective
A review of casualty evacuation in the British Army described the emergence of helicopters as a platform for medical evacuation during the Korean War [2]. Whilst helicopters were frequently used for medical evacuation in subsequent counter-insurgency operations such as Malaya, Borneo and Oman [3], it was assumed that the majority of casualties in conventional warfighting operations would be moved by ground ambulance and helicopters would not be dedicated for medical evacuation. Helicopters were designated for the medical evacuation task from Role 1 to Role 2 facilities during the military operations in the Falkland Islands, the First Gulf War and the former Republic of Yugoslavia. The Balkans experience led to the creation of the helicopter-borne Incident Response Team (IRT) which was formed from medical, Defence Fire Service and military protection personnel [1]. The IRT was designed as a package that could be rapidly deployed to an incident in a designated helicopter to transfer a casualty from point of wounding directly to a hospital. This concept was continued during Op TELIC and introduced into Afghanistan when the UK deployed to Helmand Province in 2006 [5]. The deployment to Afghanistan has introduced a new term, Medical Emergency Response team (MERT), as the collective noun for the medical personnel aboard a helicopter carrying an IRT. The use of dedicated or designated helicopters for medical evacuation from as close to point of wounding as possible to the first receiving hospital has become the international standard [6]. Ground ambulances have only been used to move casualties from point of wounding to a helicopter landing site if the local security situation or ground has prevented collection directly from the site. There is international variation in the size and type of helicopters assigned to the medical evacuation mission, the number and competencies of personnel assigned as medical escorts and the mechanisms for command and control of medical evacuation helicopters.
Medical Evacuation
Definitions and Resources
NATO medical doctrine defines a number of medical evacuation terms [7]. Medical evacuation is the movement of patients under medical supervision. The term CASEVAC has been used to describe casualty evacuation in a non-assigned vehicle/aircraft and may not include in-transit care; this term is best avoided to prevent misunderstanding. Forward Aeromedical Evacuation (FAME or more commonly MEDEVAC) provides for transfer from the point of wounding to the initial medical treatment facility. Tactical Aeromedical Evacuation (TACEVAC) is the evacuation of casualties between medical facilities within the theatre of operations.
In current operations MEDEVAC is almost invariably undertaken by helicopters. The assignment of aircraft to the aeromedical mission may be ‘dedicated’ in which the particular airframe is role specific and cannot be used for other general tasks. This might include the display of the Red Cross, modifications to take stretchers and medical equipment and fitting of specific capabilities such as a winch. This is likely to result in an aircraft most suitable for the medical mission but with a risk of non-availability. An alternative is to have designated aircraft in which a general support aircraft is assigned to the task but may be re-assigned to other tasks. This gives more flexibility as the capability can be transferred to another aircraft if the designated aircraft becomes unavailable. The difference between ‘dedicated’ and ‘designated’ has been a contentious issue in the UK but needsto be considered in the context of managing aircraft fleets rather than single aircraft capabilities [8,9].
The exact type of aircraft for rotary wing (RW) aeromedical evacuation varies by nation according to the performance, volume and protection requirements. As an example the UK has used the Puma and Sea King helicopter for this role in the Balkans, the Merlin helicopter in Iraq and the Chinook in Afghanistan. The US Army invariably uses the UH-60A which is marked with the Red Cross but has limited protective firepower. The US Air Force has a specialist aircraft the HH-60 which has a substantial night operations and protective firepower capability but does not display the Red Cross. This capability has a priority task for ‘personnel recovery’ but is primarily employed within Afghanistan to support MEDEVAC. There is also significant variation in the number and training of the medical escorts between these capabilities. The UK standard is now the Medical Emergency Response Team comprising a paramedic and a flight nurse or the enhanced MERT [MERT-E) when a doctor trained in pre-hospital care is added to the team [10]. Recent experience of opposition anti-helicopter tactics in Afghanistan has led to the requirement for a ‘gun-ship’ escort for MEDEVAC aircraft [6]. Thus the MEDEVAC mission should be considered as aviation ‘task line’ of a minimum of two aircraft rather than just the aircraft assigned to the MEDEVAC function.
Planning Medical Evacuation
The goal of ‘right patient, right platform, right escort, right time, right place’ requires a detailed understanding of the inter-relationship between MEDEVAC, TACEVAC and deployed hospital capability and capacity. Time is the fundamental factor in patient survival. The term ‘clinical timelines’ is used to describe the target times for each element of the casualty evacuation chain from point of wounding to primary surgery. Although there is dispute about the appropriate target for an acceptable time from wounding to initial resuscitation for medical planning purposes [8,9], there is widespread agreement that this should be as short as possible. There are four key timelines described in NATO policy and doctrine (Box 1)[7, 11].
The planning for the location of MEDEVAC helicopters is based upon the cumulative time between initiation of the request for evacuation – the ‘9 liner’ and the ‘wheels down’ of the MEDEVAC helicopter at the receiving hospital. This includes the time taken for the ‘9 liner’ to be initiated and passed through the communications system to the controlling headquarters, the time required to process the information and issue the launch authority, and the ‘notice to move’ time for the helicopter and crew. Thus the actual total flight time is likely to be much less than the cumulative two hours to surgery and therefore the maximum range of the MEDEVAC mission loop is not usually more than 40-60 nautical miles.
The tactical geometry for the current operating environment is based upon security forces holding areas of ground and securing this space from opposition activity. This converts the battlefield from the conventional force-on-force linear geometry with an identifiable confrontation line to an area battlefield with multiple nodes of contested space. Thus the MEDEVAC mission is converted from a linear flow to area support, hence MEDEVAC planning is based upon a ‘range ring’ coverage with a radius of 40–60 nautical miles.
Option A shows the optimum MEDEVAC solution which is the collection and return of the casualty from PoI to a Role 3 medical unit within one hour.
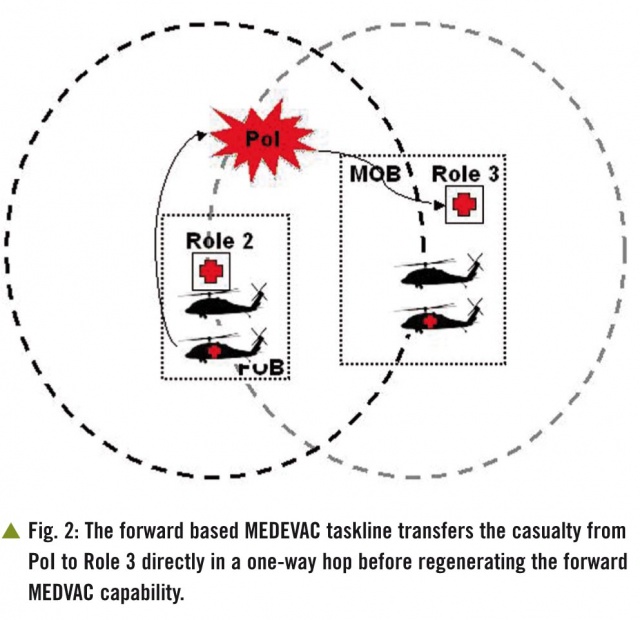
If the distance from PoI to the Role 3 exceeds 40–60 nautical miles there are three MEDEVAC planning options. As the best solution for a casualty is a single transfer to Role 3 [9], Option B is to forward base a MEDEVAC task line to extend the range ring to enable the patient to reach Role 3 but this requires a Forward Operating Base (FOB) for aviation and distorts the range ring in a single direction.Option C is to forward base damage control surgery with a Role 2 medical unit. This is less satisfactory for the patient as it is almost inevitable that the patient will require a subsequent TACEVAC move from Role 2 to Role 3.This creates an additional demand on the aviation MEDEVAC task line but does ‘protect’ the Role 3 MEDEVAC range ring as the MEDEVAC task line aircraft do not move.The final option, D, in this sequence of logic is to forward base both Role 2 and MEDEVAC.This clearly requires the most resources but is also the planning solution that covers the greatest area as the MEDEVAC taskline from the FOB now has the full ‘range ring’.It also allows the taskline from the Role 3 to support a patient retrieval TACEVAC mission.The final subtlety is the use of the ‘Role 2’ MEDEVAC taskline to move a casualty from a PoI between the Role 2 and Role 3 facility direct to the Role 3 facility thus making the flight a ‘one way’ trip rather than a collection loop. The main risk with this solution is the ‘breaking’ of the MEDEVAC ‘range ring’ supporting the Role 2 facility.It is possible to mitigate this by moving the Role 3 MEDEVAC task line forward as a replacement (Fig. 2).
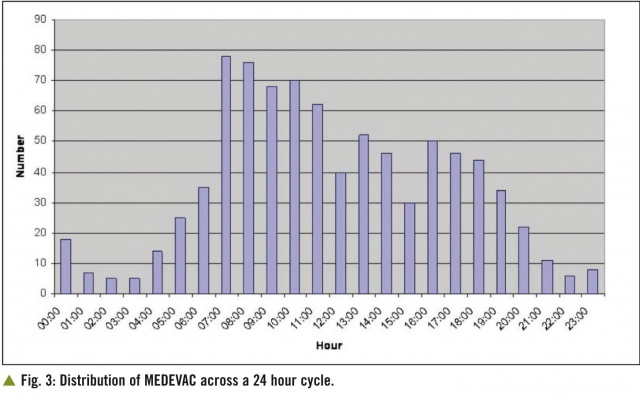
This discussion on MEDEVAC planning is based upon moving casualties from a single PoI. The next aspect of planning is to consider the capacity of the MEDEVAC system based upon the number of casualties per incident and thus the evacuation capacity of a single MEDEVAC task line, the likelihood of more than one MEDEVAC request within the timeline of a single mission and the requirement for TACEVAC using RW assets. This analysis should be based on historical evidence of the number of MEDEVAC missions requested in the 24 hour cycle (Fig. 3),
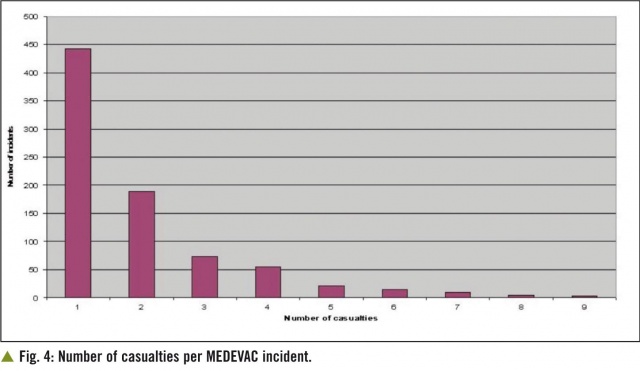
the distribution of casualties per incident (Fig. 4) and the distribution of numbers of MEDEVAC missions per day over the previous representative time period such as three months.
This historical assessment should be supported with a review of the future tactical plan to ensure that MEDEVAC laydown matches future location and distribution of the Population at Risk.This element of the planning process is clearly informed by the casualty estimate.
The final product of the MEDEVAC planning analysis is usually a ‘range ring’ laydown shown in two dimensions on the map with the numbers of MEDEVAC task lines at each location.It may also be useful to list the MEDEVAC and TACEVAC tasklines in a table so that the assignment of these to individual missions can be tracked. The aviation staff should also track airframe assignment to aeromedical evacuation tasklines and should report aircraft availability on a regular basis.It may also be necessary to track clinical escort teams in a similar manner [6].
Control and Co-ordination
Control and co-ordination (Cc) is differentiated from command and control (C2) to emphasise the fact that helicopters are commanded by aviation not medical commanders. The medical services are customers on behalf of the casualties and determine the aeromedical evacuation requirement by capability, capacity and destination. The final assignment and management of aircraft to meet this requirement is very rarely a medical function. The Cc function should be delivered from within the headquarters most suited to integrate the battlespace picture with the requests for MEDEVAC, the allocation of missions to tasklines and the selection of destination medical facility. The selection of the most suitable headquarters is complex when the MEDEVAC range rings cover ground controlled by more than one battlespace owner and may require the application of the ‘artillery principle’ of command at the highest level and control at the lowest level.
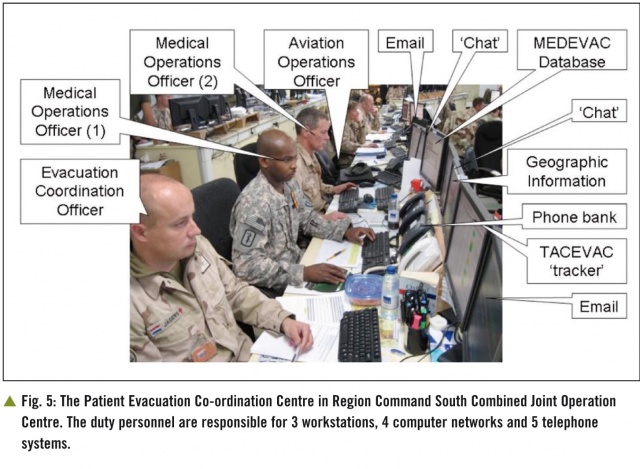
NATO doctrine (AJP 4.10A) directs that medical evacuation is controlled by a Patient Evacuation Co-ordination Centre (PECC).Operational experience has demonstrated that this must be located in the headquarters command post or Combined Joint Operations Centre (CJOC) able to both read and respond to the battle [12]. The PECC should be very closely sited to the Aviation and Air staff cells and be readily accessible to the CJOC duty officer [13]. This is the justification for separating out the PECC function from the Medical Plans function that may sit in the Medical Director’s main office. The PECC may need to be separated into the Medical Operations cell (Med Ops) providing Cc to MEDEVAC and the Evacuation Co-ordination Cell, managed by the Evacuation Co-ordination Officer (ECO) providing Cc to TACEVAC.
The Cc of MEDEVAC previously summarised [1] was an over simplification of the process. Medical evacuation is requested by the ‘9 liner’ submitted over the combat/tactical radio net to a sub-unit command post from where it is passed by the unit command net to the CJOC, either by radio or more commonly over a digital ‘chat’ system. This is highlighted by the duty watchkeeper and passed to Med Ops and the Aviation desk; both desks check the grid for the pick-up location. The Med Ops desk confirms the priority for evacuation, recommends the assignment of aircraft and medical escorts, and the destination medical facility. The aviation desk confirms the availability and suitability of the aircraft. The duty officer authorises the mission. The aviation desk then assigns the mission to the aviation commander. The aviation commander has the final launch authority for the aircraft. During the MEDEVAC mission the Med Ops desk tracks key information used for monitoring performance.
The MEDEVAC Cc process should enable the MEDEVAC task ‘right patient, right platform, right escort, right time, right destination’ to be achieved by matching the resources described to the clinical needs of the patient and the tactical environment – so called ‘intelligent tasking’. The patient’s clinical needs are described by the urgency category for delivery to a hospital facility: A – within 90 minutes; B – within 4 hours and C – within 24 hours and clarified by the MIST (Mechanism of injury, Injury, Symptoms and signs and Treatment given) report. This information enables the clinical escort to be matched to the patients’ requirements. Overall, the competencies required of the Med Ops watchkeepers depends on the range of decision options available. It is simple if there is only one aircraft type and medical escort available to deliver casualties to a single facility. More complex options require people in the decision-making process who can assess both the operational and clinical situation before making the MEDEVAC decisions.
The function of the PECC can be a challenging and complex activity, especially in multi-national operations where there may be considerable variety in the resources available, the destination medical facility, capabilities of aircraft and critically the range of communication systems (Fig. 5).
Monitoring Performance
The final element of the MEDEVAC system is the monitoring of performance as described by both Hodgetts and Cordell [1, 12] which can be divided into clinical audit, incident reporting and trend analysis. This is an integral element of Healthcare Governance on military operations.
Summary
This paper has reviewed the arrangements for the control and co-ordination of medical evacuation focussing on aeromedical evacuation, particularly MEDEVAC.It describes the range of options in the planning of medical evacuation including type of aircraft, type of medical escort and destination for a particular casualty. The purpose of the whole process is to ensure ‘right patient, right platform, right escort, right time, right place’. n
References: ref@mci-forum.com
Notice: This article was first published in the Journal of the Royal Army medical Corps. Reprint with kind permission of the Editor JRAMC.
Date: 07/04/2013
Source: MCIF 1/13









