
Article
Work-related Capacity Impairments in Self- and Observerrating in Military Personnel with Mental Disorders
Clinical Psychological Intervention Division of Freie Universität Berlin¹ (Head of Division: Prof. C. Knaevelsrud) and the Bundeswehr Psychotrauma Centre² (Clinical Director: Dr P. Zimmermann) of the Bundeswehr Hospital Berlin (Hospital Commander: Commodore (MC) Dr K. Reuter)
Beate Muschalla¹’ ²’ *, Heinrich Rau²’ *, Annika Küster¹’ ², Gerd Dieter Willmund², Christine Knaevelsrud¹
* The two lead authors, Beate Muschalla and Heinrich Rau, have contributed in equal part to this study.
Summary
Background: About 14 to 23 percent of all military personnel throughout the world suffer from mental disorders. These lead to impairments to their day-to-day life and to the psychological capacities needed to do their job. In particular, physical and mental endurance, ability to adapt to rules and regulations as well as interactional competences and specifically group integration are important for military personnel.
Methods: In an interview, 71 service members (86% male, aged 19 to 59 and on average 31 years old, 26% junior enlisted personnel, 58% noncommissioned officers, 15% officers) with different mental disorders were examined with regard to their service-related capacity status. The interview was carried out by a psychotherapist trained in social medicine and the assessment was based on the internationally evaluated observer-rating Mini-ICF-APP. Subsequently, the patients completed an analogous self-rating questionnaire concerning their capacity profile.
Results: Among patients presently unable to work[1] there was a significantly higher incidence of severe impairment to mental endurance (52% of n = 25) compared with patients who were able to work (26% of n = 46). There were no significant differences in the twelve other capacity dimensions. The patients' self-rating and the interviewers' assessment of the capacity level corresponded in most of the capacity dimensions (r = .303 – .575) and only with regard to application of competence and knowledge was there no significant correlation.
Conclusions and Outlook: Military personnel suffering from mental disorders who are unable to work (on sick leave) deserve attention primarily with a view to strengthening their mental endurance. For a case-by-case assessment of service members suffering from mental disorders – concerning either their present fitness for service or their general employability – a differentiation between the different capacity dimensions can be useful in formulating a medical evaluation from a socio-medical perspective.
Keywords: mental disorders, capacity impairment, fitness for work, military personnel
Background
Mental Illnesses and Capacity Impairments in Military Personnel
International studies show that about 14 to 23 percent of all service members [36, 40] suffer from a mental disorder. This is less than in the general population, where approximately 27 to 38 percent are affected, depending on the examination system used [39]. As a rule, mental disorders are chronic and accompanied by impairments to everyday life [27]. This is particularly the case with regard to work [4, 14] as deviations from the norm are least possible in this context.
Bundeswehr military personnel are employed not only in various areas of activity, but must also comply with special military regulations in addition to the functional requirements of the respective assignment [5, 7], meet the requirements of psycho-physical fitness and possess the ability to integrate into a group [21].
The treatment of mental disorders comprises not only the reduction of symptoms, for example mitigation of the anxiety level, reduction of stimulus-triggered intrusions or improvement of general mood. It also consists to a significant degree of capability training, such as learning how to structure their days, practising interactional skills in order to improve private or work communication [30] and reassessing and keeping themselves emotionally detached from any moral violations [18] or injustices they have experienced. It is assumed that mental fitness can also be trained in a capability-oriented process in the field of mental disorder prevention. Military psychology was one of a number of fields that provided the first real stimulus for the scientific analysis of psychological abilities in humans. A prominent example is the assessment of mental ability [16], for example when selecting personnel. Differentiations have been established over time. Since the right combination of personal abilities and military functional requirements is needed, a wide range of requirements for military fields of activity have been described [11, 13, 29, 30, 37], ranging from global intelligence [31] to emotional competences [9].
If the German Medical Service today has to deal with medical assessments concerning the fitness for duty/employability of military personnel suffering from mental disorders, regulations apply as laid down in General Publication A1-831/0-4000 [17] "Wehrmedizinische Begutachtung" (Military Medical Assessment) and in Joint Service Regulation ZDv 46/1[1] [6]. Intelligence and psyche are discussed in one section of Joint Service Regulation ZDv 46/1. The central issue in this section is the assessment of "mental fitness and intellectual capabilities" ([6, p. 42]). This does not primarily concern the psychopathological "differentiation of neuroses or personality disorders", but as it is explicitly emphasised: "What is important is the functional assessment of fitness when it has to be determined if the person examined has a sufficient degree of adaptability, functional capacity, stress resistance, sociability and thus training capacity." [6, p. 43]
The determination of capacity impairments due to illness is of key importance for any medical decision taken during an assessment of fitness for service or ability to work. In the context of non-military socio-medical evaluations, examination by means of a differentiated capacity assessment has proven to be successful and is recommended in guidelines [10, 12, 33]. It is considered good practice to use the Mini-ICF-APP observer-rating to assess capacity and participation impairment in people with mental disorders (Mini-ICF-APP) [19] as an exploration aid and guideline. It is based on a holistic biopsychosocial understanding of health problems in accordance with the International Classification of Functioning, Disability and Health (ICF) [38][2] and describes thirteen psychological capacities which may be impaired in the case of mental disorders [19]. The Mini-ICF is a rating evaluated at international level and recommended in socio-medical guidelines [2, 3, 10, 12, 22, 33] (Table 1). In terms of their application in daily clinical practice, the capacity dimensions can be understood as a detailed capacity assessment (analogous to a psychopathological assessment for describing and assessing symptoms).
It has not yet been determined in which of these capacity dimensions Bundeswehr personnel with mental disorders exhibit relevant impairments and whether patients and examining individuals assess these impairments in a similar way. To shed light on this discussion, service members with mental disorders were examined with regard to their work requirements and capacity status. The aim was also to develop an improved inventory to assess fitness for duty/service of military personnel with mental disorders. Until now, no such tools have been available with which to identify and describe in a structured way mental capacities and illness-related capacity impairments apart from symptoms.
Methodology
Participants
Service members who were receiving treatment in the department of psychiatry and psychotherapy of the Bundeswehr Hospital Berlin were assessed by means of a structured diagnostic interview concerning illness-related work capacity impairment[3]. Participation in this survey was voluntary. A few days after being hospitalised, the patients were routinely contacted by the staff and invited to participate in the research interview.
The criterion for inclusion in the survey was the presence of a mental disorder. The criterion for exclusion from the survey was the presence of acute symptoms (depressive, manic or psychotic disorders or severe alcoholism), i.e. patients not able to participate in an interview. 80 percent (n = 103) of the invited patients took part in the interview and provided written consent. Following the interview, they were asked to complete a questionnaire. Interviews and self-evaluation report data of n = 71 patients are complete and have been included in the present analyses.
The majority of the interviewees were men (86.1%). 72.2% of all interviewees have completed a vocational training course or are holders of technical education qualifications, 12.5% have a university or technical college qualification, 15.3% have still to obtain a degree qualifying them for employment. 26.4% of them belonged to the career group of junior enlisted personnel, 58.3% of them were NCOs and 15.3% were officers. The persons interviewed were 19 to 59 years old, on average 31 years old (SD = 10.02) and at the time of the interview they had been unable to work for 4.1 weeks (SD = 8.99).
On average, the patients fulfilled the criteria of 2.2 (SD = 1.6) mental disorders in the diagnostic "Mini International Neuropsychiatric Interview" (MINI) [34]. They fulfilled the criteria for the following mental disorders:
- Depressive episode (50%);
- Panic disorder (14%);
- Agoraphobia (33.3%);
- Social phobia (18.1%);
- Generalised anxiety disorder (27.8%);
- Alcohol abuse or alcoholism (11.1%);
- Post-traumatic stress disorder (PTSD) (23.6%) and
- Adjustment disorder with embitterment (18.1%).
In the interview concerning their workplace-related anxiety [24] 19.4% of the interviewees satisfied the criteria of a specific workplace phobia.
In the department of psychiatry and psychotherapy at the Bundeswehr Hospital Berlin, event-related stress reactions (diagnoses according to ICD-10, Chapter V: F 43) are the most frequent reason for patients to be treated (50%), followed by alcohol-related disorders (F 10; 13%), medical examinations and observations (Z 04; 11%), mood disorders (F 25; F 31-33; 10%) as well as anxiety and somatic symptom disorders (5%) [8].
Tools
Mental disorders were explored in the internationally established MINI [34]. The MINI interview is based on the diagnostic criteria of the "Diagnostic and Statistical Manual of Mental Disorders" (DSM).
Capacity impairments were explored on the basis of the Mini-ICF-APP [19] by means of a guideline for interviews [25] adapted to suit the military sector. Whether and to what extent impairment may be confirmed also depends on the respective context requirements (requirements of the particular activity at the place of service). The examination involved asking the patient to describe the requirements of the present assignment in order to understand which capacities are relevant for the particular activity. The interviewer was free to pose further, more precise questions to obtain a comprehensive picture of the military functional requirements. Interviewers were to actively pose specific questions to receive more information on activities and requirements such as "During my routine duty, I have to line up at seven a.m. in the morning, then, in my office, I have to deal with applications and answer questions on the phone..." The interviewer must distinguish between requirements and affective experiences such as the complaint "my work is too boring / stressful" and the like. The requirements are relevant.
The interviews were conducted by a psychological psychotherapist trained in social medicine. An interview lasted about 60 to 90 minutes. The degrees of impairment were assessed in numerical terms and notes on the precise task-related problems were taken using the free-text field. In this survey, the exploration was based on the particular activity at the place of service in the home country, since not all of the participants had experienced requirements during operations abroad. Table 1 shows the definitions of the capacity dimensions and degrees of impairment. The interrater reliability of the Mini-ICF-APP is between r = .70 and r = .90 [19].
Table 1: Capacity dimensions according to the Mini-ICF-APP as well as definitions of the degrees of impairment (according to Linden et al., 2015)
| 1. Adaptation to rules and routines Ability to follow rules and meet deadlines, to integrate into organisational processes. This includes, for example, fulfilment of daily routine tasks, keeping appointments, punctuality. |
| 2. Planning and structuring of tasks Ability to plan and structure the day, pending tasks or, if required, projects, i.e. spend an appropriate amount of time sensibly structuring the order of working processes, conducting and finishing them as planned. |
| 3. Flexibility and adaptability Ability to adapt to changing situations in terms of acting, thinking and experiencing, i.e. to alter behaviour as required by the situation. This may include requirements at short notice, changes in work requirements, changes in (working) time, relocations, new social partners or assignment of new tasks. |
| 4. Application of specialised skills Ability to apply specialised skills, i.e. based on specific training or professional and life experience. Ability to apply specialised skills and life knowledge or competences in accordance with the situation-related expectations of one's role and to meet acceptable content and specialist requirements taking into account one's personal background. |
| 5. Ability to make decisions and exercise judgement Ability to make decisions or exercise judgement in a context-related and comprehensible way. Ability to understand facts/situations in a detailed and context-related way, to draw appropriate conclusions and consequences and translate them into necessary decisions. |
| 6. Endurance Ability to persevere with an activity within the normally expected period of time (at work or when performing other tasks) and to maintain a consistent level of performance. |
| 7. Assertiveness Ability to confidently assert oneself with regard to social contacts or conflict situations and to stand one's ground without breaching social standards. |
| 8. Contact with others Ability to establish direct, informal, social contact with other people such as appropriate interaction with (new) colleges including respect, appreciation of others or the ability to make small talk. |
| 9. Group skills Ability to integrate into groups, to understand the explicit or informal rules of the group and to adjust to them. The assessment is based on behaviour in group situations or (if required) the ability to address an audience including small groups, such as the staff team, club or large groups such as the company, a political group or the Church. |
| 10. Close dyadic relationships Ability to establish and maintain a close trusting relationship with another person. The purpose is to assess an individual's ability to give and/or receive emotional warmth and achieve satisfactory harmonisation with the other role expectations and the professional environment. |
| 11. Proactivity and spontaneous activity Ability of the interviewee to initiate spontaneous activities beyond professional or social obligations. The purpose is to assess activities where the interviewee himself/herself has to become active and take some initial steps and which are not imposed on him/her, for example, by his/her profession. These may include the procurement of goods and services for everyday use, food preparation, taking care of the household or office facility. They may also include creative or recreational activities such as hobbies, visiting cultural events, recreational activities, sports or artistic activities. |
| 12. Self-care and self-sufficiency Ability to take care of oneself, i.e. the ability to wash oneself, take care of one's skin, toenails, fingernails and hair and to brush one's teeth, to wear clean clothes according to the situation, occasion and season, to be sensitive to the needs of one's body and to respond accordingly. |
| 13. Mobility and driving ability Ability of the interviewee to go to different places, face different situations and use means of transport such as car, bus or aircraft. The purpose is to assess whether the interviewee is able to find familiar public places and use all standard means of transport without any problems. |
Degrees of impairment
|
In addition to the interviewer's assessment, the patients were asked to assess the impairment of the capacities they were currently experiencing with the aid of "self-assessment questionnaire" (Mini-ICF-APP-S) based on the Mini-ICF-APP [20]. In this self-rating questionnaire, they were asked to what extent they are able to use these capacities during their work and to assess this for each of the 13 capacities by means of a visual analogue scale (from "This is clearly one of my strengths" (0) to "I cannot do this at all" (7)).
In another part of the questionnaire, the patients were asked to analogously describe in a capacity-oriented way the requirements of their present duties in Germany from their own point of view (cf. Figure 1). The contents of the items correspond to the above-mentioned capacity dimensions and can be assigned to them [26]. The interviewees were also asked about their present workability status (able or unable to work) and, if appropriate, the duration of their incapacity for work.
Results
Reported Work-related Requirements
With regard to the requirements posed by their current duties at home, personnel of the career group of junior enlisted personnel, for example, reported above all the necessity of being flexible, while noncommissioned officers mainly stressed the experience of having to do a lot of planning and of acting flexibly (Figure 1). Officers are mainly confronted with the requirements of having to provide work results within a predetermined period of time and of having to advocate specified positions. The majority of all rank categories (> 60% of the interviewees in each category) have the impression that their duties require them to withstand extreme mental stress and that cooperation with their fellow service members is of great importance.
Type of Impairment Perceived
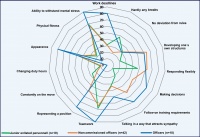 Figure 1: Requirements perceived by military personnel in their daily routine duty in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of service members who experience the respective requirements as high or very high (3 to 4 on a scale of between 0 and 4).
Figure 1: Requirements perceived by military personnel in their daily routine duty in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of service members who experience the respective requirements as high or very high (3 to 4 on a scale of between 0 and 4).
The strongest illness-related impairment of capacities referred to the fields of resilience and endurance (M=1.57, SD=1.4) and flexibility (M=1.43, SD=1.3), followed by assertiveness (M=1.07, SD=1.1) and planning and structuring capacity (M=1.00, SD=1.3). The smallest impairments referred to the fields of mobility (M=0.65, SD=0.9) and proactivity (M=0.7, SD=1.0). With regard to the levels of impairment in the individual capacity dimensions, there were no statistically significant differences between the rank categories.
Service Members Able and Unable to Work
Among patients who were unable to work immediately before their in-patient stay at the Bundeswehr Hospital, there was a significantly higher incidence of individuals frequently suffering strong impairment only with regard to their resilience and endurance (Figure 2). The interviewers' rating estimated that 52% of the patients currently unable to work cannot cope with normal everyday working life without support from others (i.e. they must be relieved by fellow service members, which corresponds at least to a capacity impairment level of 3 in accordance with the observer-ratings). Self-reports showed that service members, who were unable to work at the time in question, required support more frequently than the personnel able to work (Figure 3, self-rating level 6 to 7: "I need help from other people" or "I cannot do this at all", for example with respect to the application of knowledge and competence and regarding the making of decisions and judgements). Analogous to the observer-ratings, the self-reports also showed the most frequent significant impairments in the field of endurance: 50% of the service members currently unable to work felt that they needed support in order to endure a normal working day (Figure 3).
Patients' and Interviewers' Assessments of Capacity Impairments
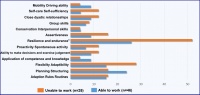 Figure 2: Capacity impairment in daily routine duty as indicated in the observer-ratings in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of military personnel who showed noticeable impairments, i.e. who needed the support of other people (rating 3 to 4 on the observer-rating scale of between 0 and 4).
Note: * p = .029 in the chi-squared test (statistically significant difference between the frequencies in the group comparison)
Figure 2: Capacity impairment in daily routine duty as indicated in the observer-ratings in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of military personnel who showed noticeable impairments, i.e. who needed the support of other people (rating 3 to 4 on the observer-rating scale of between 0 and 4).
Note: * p = .029 in the chi-squared test (statistically significant difference between the frequencies in the group comparison)
For almost all capacity dimensions (except for the application of competence and knowledge), patients' and interviewers' assessments show moderate interrelations (r = .303 – .575, Table 2).
Discussion
The various rank categories do not differ with regard to the extent of their psychological capacity impairments even though they describe different requirement profiles. In the case of personnel currently unable to work, impaired endurance seems to be most relevant, with service members attaching relevance to the ability to make decisions and exercise judgement and to the ability to apply specific technical skills.
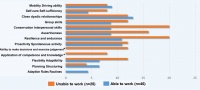 Figure 3: Capacity impairment in daily routine duty as indicated in the self-rating in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of military personnel who reported noticeable impairments, i.e. who needed the support of other people (rating 6 to 7 "I need help from other people" or "I cannot do this at all" on the scale of between 0 and 7).
Note: * p = .052 (application of competence and knowledge) *p = .018 (ability to make decisions and exercise judgement) in the chi-squared test (statistically significant difference between the frequencies in the group comparison)
Figure 3: Capacity impairment in daily routine duty as indicated in the self-rating in accordance with the Mini-ICF-APP capacity dimensions. The report refers to the percentage of military personnel who reported noticeable impairments, i.e. who needed the support of other people (rating 6 to 7 "I need help from other people" or "I cannot do this at all" on the scale of between 0 and 7).
Note: * p = .052 (application of competence and knowledge) *p = .018 (ability to make decisions and exercise judgement) in the chi-squared test (statistically significant difference between the frequencies in the group comparison)
Empirical findings from other international military contexts report a broad range of illness-related capacity and participation problems experienced on the respective post, as for example problems regarding the fulfilment of assigned tasks and duties, absences, errors, increased risk of accidents and interpersonal conflicts, sometimes even including early retirement. In this context, mental disorders are the most important reason for duty-related problems or even early retirement [15, 29, 31].
The fact that the significant problems discovered during this study refer mainly to endurance and less to adaptability or impairments regarding interaction in groups could suggest that the Bundeswehr, as a rule, is successful in matching capacities and requirement during personnel selection and task assignment. Thus, it may be possible that the capacity level – even in case of a (temporary) Axis I mental disorder[1] – remain compatible with the qualitative work requirements, while continuity and quantity of the work ability (endurance) will be reduced. This would be in line with the fact that the general fitness test already focuses on the significance of the central capacities, i.e. adaptability, performance capacity, resistance to stress and interactional capacities [6], which every service member must have in order to be able to work in the Bundeswehr.
In the Bundeswehr context, a deficiency in endurance (e.g. due to a lack of energy during a depressive episode) could most likely lead to significant impairments which require support, even if a person generally has sufficient endurance in a healthy condition (e.g. during a free interval of an affective disorder). On the other hand, a service member with an acute deficiency of endurance caused by a depression may be able to comply with rules, routines and regulations and may still have group skills, unless he/she is required to lead the group, which is reflected in less common impairments of these capacities.
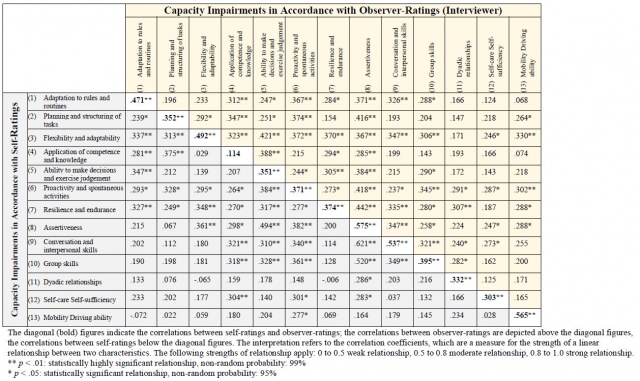
Interviewers and patients, independently of one other, made a similar assessment of the type and extent of the capacity impairments. This is in line with the empirical results of other comparisons between self-reports and observer-reports, e.g. in the fields of psychopathology and personality psychology [32, 35]. The relative conformity between the type and extent of the impairments, as reported in the self-ratings and observer-ratings based on the Mini-ICF dimensions, indicates that service members have a similar understanding of the capacity dimensions as the interviewers, who specify the impairments from the point of view of the observer-rating. Within the framework of the socio-medical performance evaluation, the self-rating questionnaire can provide additional information and possibly prepare the patient for the contents of the examination ("What can a person do (not do) because of his/her disorder?").
The capacity paradigm also offers possibilities to enter into a dialogue with patients who up to now have rejected a model of illness which includes a mental disorder. It provides an alternative for therapeutic dialogues and a way to lead the patient to the subject "behaviour and experiences" (= psyche). In some cases, the capacity paradigm may prevent the doctor-patient relationship from being burdened by conversations about "mental disorders" if the patient at first rejects the model of a mental disorder. For ambivalent patients, it is easier to accept a focus on capacities during the start of the examination – either in a diagnostic interview or a self-rating questionnaire issued in advance – than, for example, an examination with a purely clinical psychological orientation. If the dialogue starts with the question of what the patient can do at the present time and what causes problems, this may make it easier to embark on a comprehensive socio-medical psychological examination including a differential diagnosis. The focus on the requirements of duty, daily routine and the mastering of its challenges will bring the conversation round to what is for most service members the important question of how their career will continue and how they can return to duty as soon as possible. If these aspects are discussed with the individual, it is possible to involve him/her in setting the course, and the discussion about possible context-related therapy measures (step-by-step reintegration, reassignment, modification or adaptation of designated tasks instead of a complete release from service) will be possible at an early date. With regard to treatment and dismissal management, this may also be important in order to consider the career prospects at an early stage (at the time of hospitalisation).
Independent of the use of a capacity self-rating questionnaire, however, a careful clinical diagnosis and evaluation according to the medical specialist standard is indispensable for the socio-medical assessment of work ability and fitness for duty and must remain the gold standard [23]. As the assessments of patients and observers may differ in some cases and this study also shows that there is a relationship, but no complete concordance, between self-assessment and observer-assessment, it is helpful to specifically mark both perspectives in an expert opinion. This can be reported as follows: "The patient says [self-assessment of the patient]" and "We [expert, examiner, therapist] see… [observation-based diagnosis, description of behaviour]".
Limitation, Conclusions and Outlook
The concept of mental capacities, an analysis of the capacities and the graduated assessment of the support required for professional activities may be helpful for socio-medical questions, e.g. in order to decide whether a service member (temporarily) unable to work should be given a "sick leave" certificate or in order to prepare assessments in disability procedures.Due to the cross-sectional design of the study, a causal interpretation is not possible. The strength of the study lies in the fact that the interviews were conducted by a psychotherapist with expertise in social medicine.
For the purpose of treatment, the capacity concept may be useful for differentiating therapeutic objectives at capacity level (e.g. if a reduction of symptoms is not possible or not intended) [28]. In addition, it may also offer possibilities to enter into a dialogue with patients who are sceptical of mental disorder concepts. This is in line with the "mental fitness" model used for prevention purposes [1, 41].
Key Statements
- It is possible to describe qualitatively differentiated work-relevant capacity impairments in Bundeswehr military personnel of all rank categories who suffer from a mental disorder.
- The observer-ratings and self-ratings of the patients' capacity profiles are similar.
- Patients who were unable to work at the time of the study mainly suffered from a significant impairment of endurance. For these patients, treatment should focus on strengthening endurance in order to enable them to return to duty as soon as possible.
References
- Alliger-Horn C, Zimmermann P: Präventive und psychotherapeutische Praxis der Versorgung einsatzbedingter psychischer Erkrankungen im Rahmen der Bundeswehr. Verhaltenstherapie 2017; 27: 44-52.
- Balestrieri M, Isola M, Bonn R, et al.: Validation of an Italian version of the Mini-ICF-APP, a short instrument for rating activity and participation restrictions in psychiatric disorders. Epidemiology and Psychiatric Sciences 2013; 22: 81–91.
- Baron S, Linden M: Disorders of functions and disorders of capacity in relation to sick leave in mental disorders. International Journal of Social Psychiatry 2009; 55: 57–63.
- Bokma WA, Batelaan NM, van Balkom AJ, Penninx BW: Impact of Anxiety and/or Depressive Disorders and Chronic Somatic Diseases on disability and work impairment. Journal of Psychosomatic Research 2017; 94: 10-16.
- Bundesministerium der Justiz und für Verbraucherschutz (Federal Ministry of Justice and Consumer Protection): Gesetz über die Rechtsstellung der Soldaten (Soldatengesetz) (Legal Status of Military Personnel Act), in the version published 30 May 2005 (Federal Law Gazette (BGBl.) I, p. 1482), as last amended by Article 8 of the Act of 5 January 2017 (Federal Law Gazette (BGBl.) I p. 17). 2017.
- Bundesministerium der Verteidigung (Fü San I 2) (Federal Ministry of Defence – Medical Service Staff I 2): Joint Service Regulation ZDv 46/1: Allgemeine Durchführungsbestimmungen zu der ärztlichen Untersuchung bei Musterung und Dienstantritt von Wehrpflichtigen, Annahme und Einstellung von Bewerberinnen und Bewerbern für den freiwilligen Dienst in den Streitkräften sowie bei der Entlassung von Soldatinnen und Soldaten. Last amended: 27 July 2010
- Bundesministerium der Vertreidigung (FüSK III 3) (Federal Ministry of Defence – Directorate-General for Forces Policy, Branch III 3): Zentrale Dienstvorschrift A-2630/1 (Type A General Publication A-2630/1) "Das äußere Erscheinungsbild der Soldatinnen und Soldaten der Bundeswehr". Version 2 dated 21 December 2015.
- BwKrhs (Bundeswehr Hospital) Berlin: Weiße Liste (Whitelist). Zentrum für Psychiatrie und Psychotraumatologie – Psychotraumazentrum (Centre for Psychiatry and Psychotraumatology – Psychotrauma Centre). Die häufigsten Hauptbehandlungsanlässe. Bundeswehrkrankenhaus (Bundeswehr Hospital) Berlin. Downloaded 13 April 2017: https://www.weisse-liste.de/de/krankenhaus/krankenhaussuche/ergebnisliste/profil/?id=95401&searchHospital=Bundeswehrkrankenhaus+Berlin&searchType=HOSPITAL_NAME&type=hospitalUnitDetails&previousId=
- Daffey-Moor EK: Is emotional intelligence relevant to a fighting force? Journal of the Army Medical Corps 2015; 161: i14-i16.
- Deutsche Gesellschaft für Psychosomatische Medizin und Ärztliche Psychotherapie e.V. (DGPM) (German Association for Psychosomatic Medicine and Psychotherapy): Leitlinie zur Begutachtung psychischer und psychosomatischer Erkrankungen. Sk2-Leitlinie (Guideline), AWMF (Arbeitsgemeinschaft Medizinisch Wissenschaftlicher Fachgesellschaften – Working Committee of Medical-Scientific Societies) Guideline Register No. 051/029, last amended: 31 March 2012 (valid until: 31 March 2017). Deutsche Gesellschaft für Psychosomatische Medizin und Ärztliche Psychotherapie e.V. (DGPM) (German Association for Psychosomatic Medicine and Psychotherapy), Deutsches Kollegium für Psychosomatische Medizin (German College of Psychosomatic Medicine). Available online: www.awmf.org
- Doll RE, Gunderson EKE, Ryman DH: Relative Predictability of Occupational Groups and Performance Criteria in an Extreme Environment. Journal of Clinical Psychology 1969; 25: 399-402.
- Deutsche Rentenversicherung Bund (DRV) (German Federal Pension Insurance): Leitlinien für die sozialmedizinische Begutachtung. Sozialmedizinische Beurteilung bei psychischen und Verhaltensstörungen. Deutsche Rentenversicherung Bund (German Federal Pension Insurance), Berlin, 2012.
- Hambrick DZ, Rench TA, Poposki EM et al.: The Relationship between ASVAP and Multitasking in Navy Sailors: A Process-Specific Approach. Military Psychology 2011; 23: 365-380.
- Hendriks SM, Spijker J, Licht CM, et al.: Long-term work disability and absenteeism in anxiety and depressive disorders. Journal of Affective Disorders 2015; 178: 121-130.
- Hoge CW, Toboni HE, Messer SC, et al.: The Occupational Burden of Mental Disorders in the U.S. Military: Psychiatric Hospitalizations, Involuntary Separations, and Disability. American Journal of Psychiatry 2005; 162: 585-591.
- Hunt WA, Stevenson I: Psychological testing in military clinical psychology: intelligence testing. Psychological Review 1946; 53: 25-35.
- Kommando Sanitätsdienst der Bundeswehr (Bundeswehr Medical Service Headquarters) II: Type A1 General Publication A1-831/0-4000 "Wehrmedizinische Begutachtung". Version 1.2 dated 24 February 2017
- Kopacz MS, Connery AL, Bishop TM, et al.: Moral injury: A new challenge for complementary and alternative medicine. Complementary Therapy and Medicine 2016; 24: 29-33.
- Linden M, Baron S, Muschalla B: Mini-ICF-Rating für psychische Störungen (Mini-ICF-APP). Ein Kurzinstrument zur Beurteilung von Fähigkeits- bzw. Kapazitätsstörungen bei psychischen Störungen. Göttingen: Hans Huber, 2009.
- Linden M, Muschalla B, Baron S, Ostholt-Costen M: Mini-ICF-APP-S. Ein Selbstbeurteilungsfragebogen zu Fähigkeiten und Aktivitäten im Alltag und im Beruf. Berlin: Forschungsgruppe Psychosomatische Rehabilitation (Research Group Psychosomatic Rehabilitation), Charité Universitätsmedizin, 2017.
- Martins LC, Lopes CS: Rank, job stress, psychological distress and physical activity among military personnel. BMC Public Health 2013; 13: 716.
- Molodynski A, Linden M, Juckel G, et al.: The reliability, validity, and applicability of an English language version of the Mini-ICF-APP. Social Psychiatry and Psychiatric Epidemiology 2013; 48: 1347–1354.
- Muschalla B, Linden M: Sozialmedizinische Aspekte bei psychischen Erkrankungen. Teil 1: Definition, Epidemiologie, Kontextbedingungen und Leistungsbeurteilung. Der Nervenarzt 2011; 82: 917–931.
- Muschalla B, Linden M: Workplace Phobia. A first explorative study on its relation to established anxiety disorders, sick leave, and work-directed treatment. Psychology, Health & Medicine 2009; 14: 591–605.
- Muschalla B: Mini-ICF-APP Interviewer Ratingbogen. Aktivitäts- und Fähigkeitsbeeinträchtigungen bei psychischen Erkrankungen bei Bundeswehrsoldaten. Freie Universität Berlin and Bundeswehr Hospital Berlin, 2016.
- Muschalla B: Assessing objective psychological work demands by means of self-rating – Is this possible? Forwarded to the Journal "Gruppe Interaktion Organisation".
- Muschalla B, Vilain M, Lawall C, Lewerenz M, Linden M: Participation restrictions at work indicate participation restrictions in other domains of life. Psychology, Health & Medicine 2012; 17: 95-104.
- Muschalla B: Fähigkeitsorientierte Verhaltenstherapie bei psychischen Erkrankungen. Verhaltenstherapie 2014; 24: 48–55.
- Pflanz SE, Ogle AD: Job Stress, Depression, Work Performance, and perceptions of Supervisors in Military Personnel. Military Medicine 2006; 171: 861-865.
- Redmond SA, Wilcox SL, Campbell S, et al.: A brief introduction to the military workplace culture. Work 2015; 50: 9-12.
- Ree MJ, Earles JA, Teachout MS: Predicting Job Performance: Not Much More Than g. Journal of Applied Psychology 1994; 79: 518-524.
- Schotte CKW, de Doncker DAM, Dmitruk D, et al: The ADP-IV Questionnaire: Differential Validity and Concordance with the Semi-Structured Interview. Journal of Personality Disorders 2004; 18: 405-419.
- Schweizer Gesellschaft für Versicherungspsychiatrie (SGVP): Qualitätsleitlinien für psychiatrische Gutachten in der Eidgenössischen Invalidenversicherung. Schweizer Gesellschaft für Versicherungspsychiatrie und Schweizerische Gesellschaft für Psychiatrie und Psychotherapie SGPP, Bern, 2012.
- Sheehan D, Janavs J, Baker R, et al.: MINI. Mini International Neuropsychiatric Interview. Tampa: University of South Florida, 1994.
- Steketee G, Frost R, Bogart K: The Yale-Brown Obsessive Compulsive Scale: Interview versus Self-Report. Behaviour Research and Therapy 1996; 34: 675-684.
- Trautmann S, Goodwin L, Höfler M, et al.: Prevalence and severity of mental disorders in military personnel: a standardised comparison with civilians. Epidemiology and Psychiatric Sciences 2016; 18, ahead of print.
- Tziner A, Meir EI: Occupational Congruence and Personal Task-Related Attributes: How Do They Relate To Work-Performance? Journal of Career Assessment 2002; 10: 401-412.
- WHO: International Classification of Functioning, Disability and Health. World Health Organisation: Geneva, 2001.
- Wittchen HU, Jacobi F, Rehm J, et al: The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology 2011; 21: 655–679.
- Zamorski MA, Bennett RE, Rusu C, et al.: Prevalence of Past-Year Mental Disorders in the Canadian Armed Forces, 2002-2013. Canadian Journal of Psychiatry 2016; 61: 26S-35S.
- Zimmermann P, Kowalski J, Niggemeier-Groben A, et al.: Evaluation of an inpatient preventive treatment program for soldiers returning from deployment. Work 2015; 50: 103-110.
Conflicts of interest / positions:
Heinrich Rau and Gerd Dieter Willmund are active German Medical Service officers. Beate Muschalla and Annika Küster are clinical psychological scientists working at the Bundeswehr Hospital Berlin within the framework of the project. Christine Knaevelsrud is initiator and head of the overall project.
Citation format
German:
Muschalla B, Rau H, Küster A, Willmund GD, Knaevelsrud C: Dienstbezogene Fähigkeitsbeeinträchtigungen in der Selbst- und Fremdeinschätzung bei Soldaten mit psychischen Erkrankungen. Wehrmedizinische Monatsschrift 2017; 61(11)): 260 - 268.
Citation format
English:
Muschalla B, Rau H, Küster A, Willmund GD, Knaevelsrud C: Work-related capacity disorders in self- and observer-rating in military personnel with mental disorders. Wehrmedizinische Monatsschrift 2017; 61(11)): 260 - 268.
Corresponding author:
Dr Beate Muschalla
Psychologie, Freie Universität Berlin,
Habelschwerdter Allee 45, 14195 Berlin, Germany
E-Mail: [email protected]
This article is also available in German.
[1] Axis I mental disorders are defined as acute mental disorders which are manifested by symptoms (anxiety, depression, substance addiction) and significantly impair the lives of the patients. Axis II mental disorders are classified as personality disorders. These describe permanent inflexible experience and behaviour patterns (e.g. obsessive-compulsive, insecure, aggressive, dramatic, erratic, anti-social) and may, like Axis I mental disorders, lead to considerable problems with regard to the ability to cope with everyday life and to participate in social interactions.
[1] General Publication A1-831/0-4000 [17] "Wehrmedizinische Begutachtung" (Military Medical Assessment) states that, until a revised version is issued, the preceding document, Joint Service Regulation ZDv 46/1 [6], remains valid concerning the assessment of fitness for military service in case of health problems.
[2] The International Classification of Functioning, Disability and Health (ICF) was published by the World Health Organisation as a new classification system in 2001. The holistic biopsychosocial health model of the ICF makes it possible – beyond the level of symptoms – to take into account environmental factors and activities when describing health problems. As the ICF containing almost 1500 individual items cannot be applied in practice, specific tools must be used for its application.
[3] This is part of a larger project approved by the Bundeswehr (U 2.1 d E/U2AD/FD002/FF550). The ethics commission of Freie Universität Berlin has given its consent to the research project. The present survey was carried out as part of a pilot study.
[1] The term "unable to work" from social medicine, which is also used in this paper for the sake of simplicity, when used in the military field refers to the fact that the service member concerned is principally fit for service but temporarily unable to perform their duties for health reasons.
"Unfit for service", however, implies a status which permanently prevents the service member from performing military service for reasons of health.
Date: 11/02/2017
Source: Wehrmedizinische Monatszeitschrift 11/2017











