Article: W.C. DORLAC, J.M. BISHOP, G.R. DORLAC (USA)
Use of Simulation and Military Medical Training: 2014
Use of simulation of all types is playing an ever-increasing role in medical education at all levels of civilian and military medical training. Increasingly, uses of simulation are expanding to additional applications such as skills assessment, credentialing, quality improvement and research. Simulation now augments nearly every clinical and operational training program.
Introduction
Over the past two decades, simulation has played an increasing role in both civilian and military medicine, now fulfilling a wide variety of objectives beyond the initial role of education. It has been incorporated into training programs at all levels and across most disciplines. Multidisciplinary simulation training has been evolving to enhance interdisciplinary collaboration, communication, resource management and transitions of care.
The military has embraced simulation with even more vigor than most civilian training programs, resulting in a wealth of experience and success. These initiatives have been driven by a number of factors to include the lack of “live” patients, the need to train large numbers of personnel, the need for sustainment of operational-specific skills, and the need for standardization of situational exposure and training. Additionally, simulation provides an opportunity to perform extremely high risk medical tasks in a no-risk training environment.
This increased reliance on simulation has driven educators in the search for ways to best use simulation and to validate its benefits. The purpose of this review is to summarize some of the key issues in using simulation for military training.
Objectives of Simulation
Simulation was initially introduced as an educational tool, and that is the context in which medical providers are still most frequently exposed to simulation. Simulation can be used to teach anatomy, physical exam skills, procedures (from basic to complex), clinical skills, disease recognition, medical team training and equipment proficiency. More advanced skills that can be honed using simulation include team leader training, critical thinking, situational awareness, crew resource management and interpersonal communication skills training. In addition to its role in individual and team education, simulation is being used in research and quality improvement programs, as well as in high-stakes testing to evaluate clinical competency.
Pros and Cons of Simulation
Adult learners have long been identified as benefiting from hands on experience. In the words of Confucius, “I see and I forget, I hear and I remember, I do and I understand.” Edgar Dale first described the cone of learning in 1946, proclaiming that after two weeks we tend to remember 10 % of what we read, 20 % of what we hear, 30 % of what we see, 50 % of what we see and hear, 70 % of what we say, but 90 % of what we say and do.1
Experiential learning has a long standing history in medical education. A common example of this is apparent in a common saying heard throughout academic medical centers is, “See one, do one, teach one”, with emphasis being placed on the “do”. With limitations on duty hours and an ever increasing volume of information to absorb, there is a greater need to obtain and retain a vast amount of knowledge in a limited time frame. Educational designs must be tailored to meet these demands, and simulation provides an ideal approach. Simulation scenarios can be designed to assure that key clinical elements are taught, reinforced and better retained. In terms of availability and portability, manikins as a training model are readily available and easier to transport than animals, cadavers or actors. High-fidelity full human simulators can help to compensate for limited clinical exposure by giving ready access to a variety of standardized clinical scenarios, many of which may be infrequently encountered when overall patient exposure is limited. Simulators are ideal in the military medical setting to maximize exposure and realistic response to medical decision making while minimizing time away from primary operational duties. Students are able to perform a clinical scenario over and over again and this repetition has been shown to improve learning. Simulation provides a controlled scenario and environment that can be replicated from group to group and be fully customized to meet the needs of a trainee. It also allows for targeted and immediate feedback with an unsurpassed freedom to learn from mistakes.
Despite many advantages, there are also challenges to simulation use. In comparison to traditional lecture-based education, simulation training is expensive and labor intensive. Significant resources must be invested to develop simulation training programs. Physical resources in the form of proprietary medical simulators, live animal tissue models, cadavers, disposable materials, physical space, and medical equipment must be obtained and dedicated for the sole purpose of training. High-fidelity full human simulation manikins require dedicated personnel, equipment and space to utilize them properly. For many programs, they are prohibitively expensive. A model designed for anesthesia education may cost as much as US $ 250,000. Simulation training is also time intensive, requiring dedicated time to develop, enact, evaluate and debrief each simulation experience to maximize the benefit to the trainee. Experts with both clinical expertise and experience in the use of simulation are essential to optimize training. Furthermore, some educators question how simulator experience translates to a “real patient”. Although rapidly improving, the manikins are still artificial in appearance and feel, which can limit the trainee’s ability to suspend disbelief and fully immerse in the scenario. Finally, and perhaps most importantly, many of the current simulators are not validated, and their real benefit in terms of outcomes is often unknown. Because there are limited data available to clearly quantify the value of this type of education, the aforementioned resources and the associated costs may be difficult to justify.
Levels of Simulation in Training
A recent paper from the United Kingdom organized training simulation into three categories, as determined by the training focus, skills and format. These three groups were termed microsimulation, mesosimulation, and macrosimulation.2 Microsimulation is that which focuses on training the individual, emphasizing basic motor and cognitive skills and occurring in a basic skills laboratory. Mesosimulation focuses on training clinical teams, emphasizing higher cognitive and behavioral skills and occurring in a simulated specific environment. Finally, macrosimulation focuses on training organizations or institutions, emphasizing organizational fitness for purpose and occurring in a hospital/system.
Examples of these different types of simulation training can be found throughout the military:
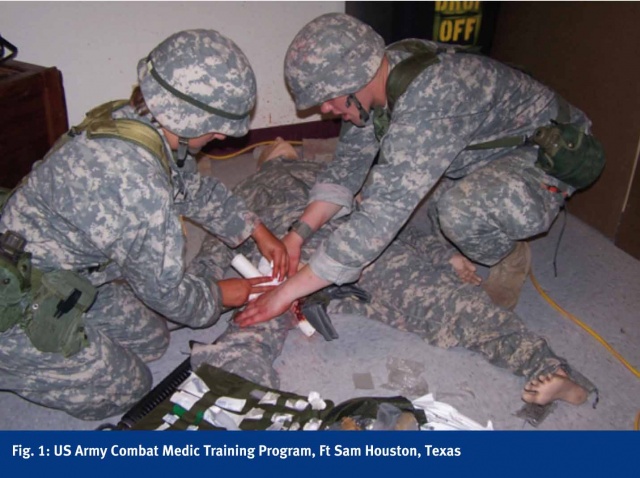
Microsimulation is used at the US Army 68W Combat Medic training program in San Antonio, Texas-the training facility for entry level Army combat medics. A large number of medics are trained (7500 annually) in a
16-week training course emphasizing the following: Emergency Medicine Technician Basic (EMT-B), limited primary care, tactical medicine (Tactical Combat Casualty Care), situational training exercises and a final field training exercise. Simulation is used extensively and is critical for the certification process in both cardiopulmonary resuscitation (CPR) and EMT-B. Skills taught and reinforced through simulation include combat casualty assessment, tourniquet use, utilization of hemostatic agents, needle chest decompression, surgical airway, laryngeal airway, intravenous and interosseous catheter placement. In addition to training and reinforcement, simulation is also used for skills assessment and validation. Currently, about 60 to 70 percent of students will deploy and utilize the knowledge and skills obtained during this training for real casualty care within six months of graduation from their advanced individual training. (Fig. 1)
Mesosimulation is used at the Army Trauma Training Center in Miami, Florida. This center offers a team based training course where more advanced procedures and higher cognitive functions are taught along with inter-professional team training, emphasizing communication, mitigation of task saturation and crew resource management. In addition to high-fidelity full human simulators, live tissue labs are utilized. An exercise takes place where clinical scenarios are presented and managed by the trainees while immersed in a simulated combat environment compounded by resource limitations, security breaches, power outages and other stressors. The simulated exercise allows the team to practice their combat trauma skills in addition to teamwork, organization, resource allocation, communication, treatment and overall performance. Team leaders obtain a realistic, working knowledge of their team’s capabilities, limitations, weaknesses and strengths. (Figs. 2, 3)

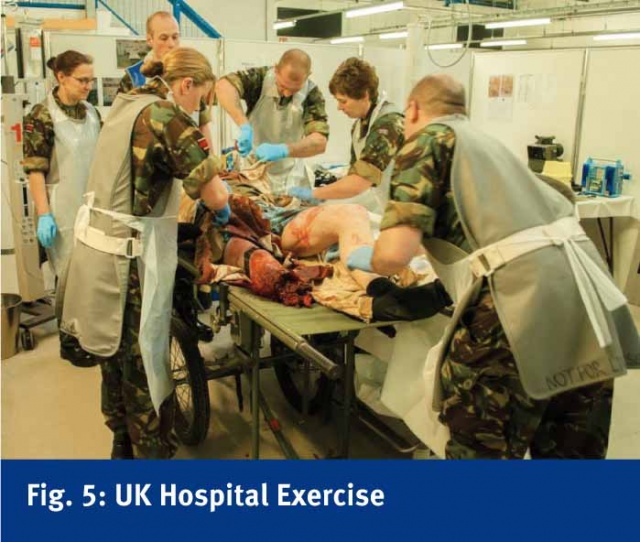
Macrosimulation training is employed at the Army Medical Services Training Centre at Strensall, York, a pre-deployment training platform for an entire deployable hospital. Multinational training is regularly carried out at this simulation center, which is a mirror image of the UK field hospital in Camp Bastion, Afghanistan. Using a developed process known as the Imperial Personnel Assessment Tool, they have been able to evaluate crisis management, trauma care, hospital environment, operational readiness and procedural skills. Simulation occurs at all levels and for the entire hospital personnel and their specialties. They incorporate a number of simulation tools to include high-fidelity full human simulators and moulaged ex-combat patients with amputations. (Figs. 4, 5)

These are individual examples of the different categories of simulation currently in use for military medical training. Many more are in practice, with others constantly being developed and evolving to meet the rapidly changing needs of the operational units that military medics support. Each individual training platform has the opportunity to alter and modify scenarios and incorporate new technologies for the purpose of assuring maximum preparedness of the deploying military medical personnel. Oftentimes, individual training platforms combine efforts or exercises to go from micro- to meso- and on through macro-level simulation, further enhancing the value and realism.
Simulation Tools
A variety of patient simulation tools exist and their use must be optimized in the context of a given curriculum. Simulation cannot replace all other education material; it must be used as an adjunct to enhance the education and retention of a given topic. A comprehensive curriculum design should consist of didactic instruction, detailed description and demonstration of the procedure to be trained with explanation of complications and pitfalls followed by simulator-based instruction. Pre-scenario simulator instruction must include familiarization with the model and identification of how the model differs from reality. As in many of the training types previously discussed, a complex scenario may involve multiple simulation tools. To optimize the effectiveness of simulation, there is a need for “suspension of disbelief”. When this occurs, the participant feels as though the simulated patient is a real casualty in a real clinical scenario. This is best obtained when the simulation tool is carefully matched to meet the clinical objectives of the scenario by providing an appropriate level of realism, while minimizing distractions of the simulation tools themselves.
Simulation tools include the following:
Live animals have the advantages of living tissue, allowing for actual bleeding, a life and death situation and standardized injuries. However, there are a number of disadvantages as well, including dissimilar anatomy, governance laws, veterinary support and the potential for disease transmission. An example of their use in training would be the American College of Surgeons Advanced Trauma Operative Management (ATOM) Course which is designed to teach advanced trauma skills to junior surgical residents.
Human Cadavers (fresh or preserved) have the advantages of exact anatomy and real tissue handling. Advanced techniques with cadaver models can include perfusion with a pump and artificial blood to allow for simulated bleeding. This realistic visual and tactile interface enhances the suspension of disbelief. However, there are a number of disadvantages as well, to include limited cadaver availability, potential disease transmission and lack of relevant bleeding unless a perfused model was used. Additionally, this resource has limited opportunity for multiple use trainings, especially when utilized for procedural training. An example of current use in training would be the American College of Surgeons Advanced Surgical Skills for Exposure in Trauma (ASSET) Course which is designed to teach surgical exposure for trauma to senior surgical residents and refresher training for surgeons out of training.3,4
High-fidelity task trainers are used to focus on a single procedure or set of procedures and offer similar anatomy, are re-usable, easily transported and may give immediate feedback (such as bleeding). However, there are a number of disadvantages as well, to include a potential need for reprocessing, which can be costly, and less than optimal tissue handling. An example of their use in training would be a craniectomy model designed to teach junior neurosurgery residents or trauma surgeons.5
Low-fidelity manikins have the advantages of being more durable, easily transportable, relatively inexpensive and can be moulaged to meet a specific patient appearance. Disadvantages include non-realistic tissue appearance or feel, need to simulate even the most basic procedures, and lack of realistic immediate feedback. These forms of low tech manikins are used to teach very basic medical skills, but their utility can be limited by the trainee’s inability to suspend disbelief.
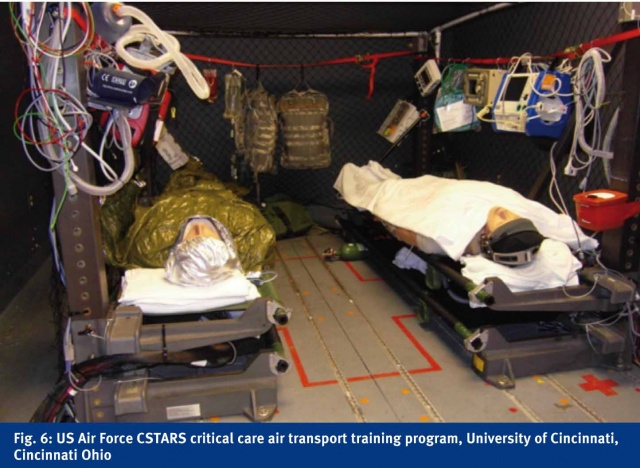
High-fidelity full human manikins (which widely vary from very realistic tissues to simulated human physiology) have the advantage of being able to demonstrate complex physiology, a more realistic interaction to the trainee, may be “vascularized” and be capable of immediate feedback. Disadvantages include cost, requirement for ongoing maintenance, and lack of portability and durability. Although they try to simulate the human body, they are not perfect. Lungs for an example do not respond to manual ventilation in the way a human lung would. An example of their use in training would be the use of METI HPS simulators at the USAF advanced Critical Care Air Transport Team (CCATT) training program which are designed to teach physiology, anatomy, task saturation, equipment interactions, ICU management and anesthesia.
Moulaged actors for human injury models have a number of advantages, to include lower cost, enhanced realism, immediate verbal and movement feedback and portability. Some programs use actors who may have real amputations, simulated wounds, or strap on prosthetic body parts upon which procedures can be performed. However, disadvantages still exist, to include need for manpower and actors who may require specific training for each event. An example of training using moulaged live human models would be the realistic training that occurs by the Norwegian special operations units and the UK HOSPEX which incorporate amputees into scenarios (Amputees in Action Ltd). These can be used to teach triage, mass casualty events, patient movement, and significantly help with the “suspension of disbelief”.
Simulation of the environment (to include location, temperature, noise, light, vibration, lethality) is an adjunct to all forms of simulation in an effort to make the scenario more realistic and akin to the environment where the medical care will be provided.
Best Practice use of Simulation in Education
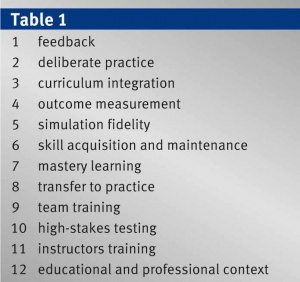
In a critical review of the literature on simulation-based medical education research, McGaghie identified twelve concepts and components of the best practice of simulation based medical education. This paper serves as an excellent framework for the development or the refinement of any simulation based training program.6 (TABLE 1)
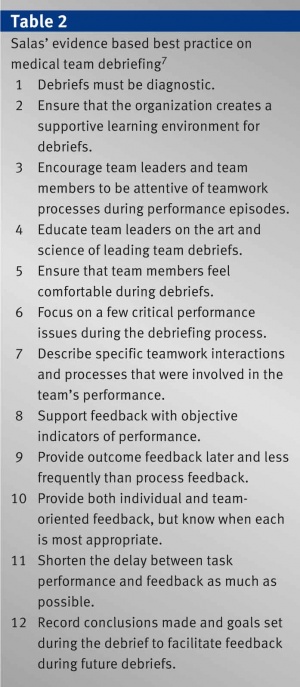
Feedback is a critical component of effective simulation. Post-scenario debriefings that review critical errors and strengths are described as formative feedback. This type of feedback is designed to emphasize educational goals and improve trainee performance. Feedback may also be summative, merely for the purpose of “pass or fail”, and has less of an educational purpose.7 (TABLE 2)
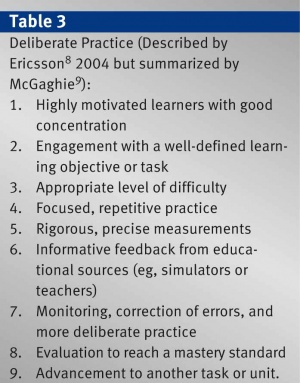
Deliberate practice refers to the process of learning that is accomplished after initial rote learning. It addresses the behaviors and skills of learning and the “how we learn”, to include motivation, individualized training, manner of feedback and need for repetition. It is this targeted, intentional repetition that truly solidifies the trainee’s learning. Simulation in its best form provides ample opportunity for deliberate practice of the material being taught. There are 9 features of deliberate practice originally described by Ericsson in 2004 but summarized by McGaghie.8,9 (TABLE 3)
Curriculum integration must occur for simulation to be used optimally and fully. Simulation training and maintenance should be fully integrated within the trainee’s educational process and focused on specific educa-
tional objectives. This requires planning, scheduling, dedicated time and ideally dedicated instructors, as does any other fully integrated clinical component of a trainee’s education.
Outcome measurement that yields reliable data will assist in feedback, assessments and validation. Outcomes are most commonly based on observer ratings or trainee responses. Haptic sensor measurements and the use of simulator physiology are more advanced techniques which may be used.
Simulation fidelity should meet the training objectives or educational goals. A task trainer may be sufficient to teach a given skill, whereas a high-fidelity full human physiologic manikin may be required to instruct more complex concepts or procedures.
Skill acquisition and maintenance of clinical and procedural skills are common uses of simulation. The idea of how often one must train to prevent skill decay is currently being explored but appears to depend on the level of training of a trainee, the complexity of the skill being performed and the time between training and follow-up measurements.
Mastery learning is a term which describes education which has a goal of complete mastery of a given concept or procedure. Programs seeking mastery ensure that all trainees fully meet all of the educational goals with minimal variation during outcomes measurement. Such programs require clearly defined objectives, standards and measurement tools. The amount of time spent training or the number of repetitions needed to reach mastery will vary among trainees.
Transfer to practice addresses the “why”. Although simulation may be fun to play with, it must directly translate to improved clinical outcomes or skills in dealing with actual patients or situations. Fewer complications, improved disease recognition, and better team dynamics during resuscitation would all be examples that would ideally result from the use of simulation.
Team training is a component of nearly every advanced scenario because medical care tends to be carried out by a team of providers rather than a single individual. Simulation can be used to train and assess a variety of key components of team dynamics, to include leadership, situational awareness, task saturation and communication.
High-stakes testing refers to the increasing use of the results of simulation testing as a component of certification or licensure. In order to be valid and accepted, the simulation data generated and used for such determinations must be highly reliable and reproducible.
Instructor training is an area often overlooked or misunderstood but is essential for any type of effective learning program. A million dollar simulation center will be essentially worthless without educators who know how to optimize training using these models. Instructors do not need to be from the same field of study but must be motivated and specifically trained for the role. Clinical expertise alone does not translate to effective simulator instruction.
The educational and professional context in which simulation is used is critical in the design and utility of a program. For example, programs involving high-stakes testing require authenticity and a realistic scenario that directly applies to the clinical process being evaluated. The impact, credibility, and benefit of simulation based medical education will be greatly influenced by how it is integrated into a training program.
Areas Using Simulation Medical Education
Every medic, nurse and physician training program in the United States currently uses some form of simulation as part of the formal education process. Accreditation Council for Graduate Medical Education (ACGME) has attempted to redefine experiential education to move away from the traditional “see one, do one, teach one” model that has long been central to medical education. Simulation based education provides an opportunity to practice skills repeatedly in a risk-free environment in order to achieve proficiency. ACGME has recognized that simulation can successfully be utilized in the education of medical residents in each of 6 core competencies: Patient Care, Medical Knowledge, Practice-based Learning, Interpersonal and Communication Skills, Professionalism, and Systems-based Practice. Therefore, it has now mandated that each individual training program has a simulation requirement for accreditation. Simulation is currently a component of every US medical and surgical residency program.
In addition to the direct effect on a trainee’s procedural skill, programs using simulation have demonstrated collateral benefits. In one study, internal medicine residents trained in central venous catheter insertion using simulation showed improved proficiency in the procedure. Moreover, in subsequent years new residents were more proficient prior to their own initial simulation training due to better bedside teaching from their senior, simulation-trained residents.10
Assessment and Evaluation
Teaching hospitals have traditionally led the field in the use of simulation. Simulation use remains most prevalent in education, but is also beginning to be used in medical provider assessment, quality improvement programs and research.11
Examples of simulation’s role in assessment and evaluation of skills and knowledge within the United States include the USMLE Step 3 Computer-Based Case Simulations, Advanced Cardiac Life Support and Advanced Trauma Life Support, Maintenance of Certification for many specialties, the American Board of Internal Medicine (i.e, Interventional Cardiology) and Anesthesia.
Credentialing
Credentialing for procedures now occurs in part by the American Board of Surgery with a requirement in Fundamentals of Laparoscopic Surgery and Fundamentals of Endoscopic Surgery which utilize simulation as a key element to the assessment of applicants. The American Board of Internal Medicine has instituted a simulation program for maintenance of certification in the field of interventional cardiology, by which high-fidelity full human simulators are utilized to assess procedural skills. In 2008, the expert panel on credentialing for the Commonwealth of Massachusetts Board of Registration in Medicine formally recognized high-fidelity simulation as an acceptable method to assess clinical competencies for the purpose of medical staff credentialing. Many hospital systems have, in turn, incorporated high-fidelity simulation assessments as part of the privileged provider credentialing process.
Many facilities are developing programs to incorporate medical simulation as an integral part of provider assessment and evaluation. These high-stakes testing procedures and evaluations are likely to become commonplace in the medical field and will be included in the assessment of providers ranging from nurses, physicians, advanced practice providers, dentists, physical therapists, to respiratory therapists.
Validation
Within the military, validation of clinical and operational competencies before deployment to an active combat zone occurs in a few select programs. These include the US Special Operations Command medic training, the United Kingdom Ministry of Defense training with HOSPEX, a hospital based simulation, and the US Air Force Critical Care Air Transport Team (CCATT) program. As a part of CCATT maintenance of training, simulation is used to assess every facet of medical management and operational readiness. This includes equipment proficiency testing using standardized equipment, such as intracranial pressure monitoring, defibrillators, infusion pumps, and transport ventilators. Environmental immersion patient care scenarios are utilized in live flight exercises aboard C-130 aircraft with low fidelity manikins to assess team communication, resource management, and situational awareness in a realistic environment. Finally, a series of high-fidelity simulations with significant environmental manipulation involving two complex resuscitations occurring simultaneously are administered for assessment, evaluation and directed feedback for a standard treating three member team. The compilation of clinical and operational competencies assessed provides adequate data to determine capability to effectively provide patient care in the deployed setting. Common to all three programs is the ability to deny deployment to individuals who fail to validate during simulation training. (Fig. 5)
Research
Simulation has been used as a way to standardize clinical experience and performance. In a study performed at the Oxford Orthopedic Simulation and Education Centre at the University of Oxford, orthopedic surgery residents already competent in diagnostic knee arthroscopy but without prior meniscus repair experience were trained with an arthroscopic meniscus repair simulator. Their learning curve was found to be variable, with some reaching a plateau in performance after twelve procedures while others required as many as 21 training episodes before reaching a plateau.12 This important study highlights the need for individualized training and education. Learners given a specific task will progress at a variable pace, and that rate is difficult to predict. Mastery varies depending on the procedure or task to learn and ndividual aptitude. This important concept has been utilized in many areas of medical education to redefine the amount of training required to progress and complete a training exercise. By identifying core competencies and assessing individual skill sets, programs can define progression and completion based on achievement, as opposed to arbitrary time tables.
Simulation training is an optimal education modality as it allows for immediate feedback, identification of strengths and weaknesses, and development of individualized training given the performance on an individual task or scenario.
Maintenance of procedural skills has also been assessed with simulation. Significant simulation-trained psychomotor skills deterioration was noted when studied in first year surgical residents using virtual simulation in a controlled setting that measured both cognitive and psychomotor skills.13 Laparoscopic proficiency was measured by assessing the smoothness of hand and instrument movements. Trainees were trained to proficiency, tested and then retested monthly for six months to assess deterioration of skills. Following the study, they were then retrained to their original proficiency and the number of iterations was assessed. In this study a significant deterioration in acquired skills was noted at 4 months. The number of iterations required in retraining was significantly fewer than the iterations required for initial training.
One of the most difficult things to assess is the benefit of any educational tool on clinical outcomes. Simulation has traditionally measured “benefit” by instructor observation (pass/fail), trainee responses (did you learn anything?), or the time required to complete a given tasks. More advanced assessments of outcome include haptic data (where motion and efficiency are evaluated) and task saturation by participants.14
Future of Simulation
Simulation based medical education is constantly evolving to meet the demands of expanding medical knowledge, limited time and exposure to trainees, and limited financial resources. This is true in both civilian and military medical education. Research efforts must be focused to optimize the utilization of current simulation practices and to advance simulation with new technologies and experiences. Still in their relative infancy are the roles of virtual reality and defining the role of simulation in the maintenance of skills, specifically the timing and the degree of follow-up training. In addition there is a continuing need for better tools to mimic reality, respond realistically in real time to the trainee, and facilitate training on multiple skills rather than a single task. Educators and trainees demand increasingly lifelike and realistic manikins. At present the DoD is investing millions to improve simulation and to demonstrate the relative merits of different simulation tools currently available (i.e. grants to the University of Missouri and the University of Minnesota).
Any piece of equipment is only as good as the educator using it. The importance of developing formal curriculum to ‘teach the teacher’ on the optimal practices for manipulating the simulation, interpreting the interactions of the trainees, and providing assessment and feedback cannot be understated. The rate of advancement of these practices are dependent upon the dedication of the educators to answer these important questions, advance research and technology development and to teach future generations of educators.
As high-stakes testing becomes more prevalent, it will be vital to develop formalized and objective measurements of performance and outcomes. When used simply as an educational tool, feedback is provided in a formative fashion, based on subjective opinion of the observing clinical expert. This often meets the educational needs of the trainee, but can be extremely difficult to standardize when summative feedback is required, as is the case in credentialing evaluations, validation platforms, and certification examinations. Objective measures of communication efficacy, teamwork, collaboration, resource management, and situational awareness must be developed to secure simulations role in formal assessment of these medical skills.
Summary
Simulation can encompass anything from the simplest task trainer to a multiple patient hospital scenario. Use of simulation of all types is playing an ever-increasing role in medical education at all levels of civilian and military medical training. Increasingly, uses of simulation are expanding to additional applications such as skills assessment, credentialing, quality improvement and research. The DoD is making unparalleled contributions to these efforts through substantial investments in resources and research, which is helping to drive many of these developments. Simulation now augments nearly every clinical and operational training program. Simulation has been demonstrated to teach a wide variety of skills and procedures and likely promotes patient safety. n
References: ref@mci-forum.com
Authors
Warren
C Dorlac, MD
Col. (Ret) Warren C. Dorlac, MD, FACS is Medical Director of the Acute Care Surgery Service and Associate Professor of Surgery at the University of Cincinnati. He is an active member of the Division of Trauma and Surgical Critical Care with an interest in aeromedical transport and trauma care research. Col. Dorlac served on active duty with the USAF for 26 years, retiring in Oct 2011, and is credited with many trauma system advancements. His last military assignment was as Director of the advanced Critical Care Air Transport course, 2007 to 2011. In addition, he served as the Trauma Consultant to the USAF Surgeon General from 2008 through 2011. In 2009, he deployed as the Central Command (CENTCOM) Joint Theater Trauma System Director where he oversaw trauma care in Iraq and Afghanistan. In his prior assignment, he was the Trauma Medical Director at the Landstuhl Regional Medical Center in Germany.
Col (Ret), USAF, MC, FS
Associate Professor of Surgery
Division of Trauma and Critical Care
University of Cincinnati and
Uniformed Services University
Cincinnati, OH 45267
E-mail: Warren.Dorlac@uc.edu
Fax 513-558-3136
Office 513-558-5661
First and corresponding author
CO-AUTHORS
Jonathan M Bishop, MD
Assistant Professor of Medicine
Section on Pulmonary, Critical Care,
Allergy & Immunologic Diseases
Wake Forest Baptist Medical Center
Winston Salem, NC 27157
jmbishop@wakehealth.edu
Phone 336-716-1210
Gina R Dorlac, MD
Col (Ret), USAF, MC, FS
Associate Professor of Surgery
Division of Trauma and Critical Care
University of Cincinnati
Cincinnati, OH 45267
Gina.Dorlac@uc.edu
Fax 513-558-3136
Office 513-558-5661
Date: 09/30/2014
Source: MCIF 3-14