
Article: Heidi Danker-Hopfe, Cornelia Sauter, Jens T. Kowalski (a), Stefan Kropp (b,c), Andreas Ströhle (d), Ulrich Wesemann, Peter L. Zimmermann
Impact of deployment in Afghanistan on sleep quality and daytime sleepiness in German soldiers
From Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Competence Center Sleep Medicine1(Head: Prof. Dr. Heidi Danker-Hopfe), an the Bundeswehr Psychotrauma Center (Head: Colonel (MC) Assoc. Prof. P. Zimmermann) at the Bundeswehr Hospital Berlin (Commander and Medical Director: Admiral (MC) Dr. K. Reuter)
SUMMARY
In this prospective study subjective sleep quality and excessive daytime sleepiness prior, during and after deployment of German soldiers in Afghanistan were examined. Sleep quality (Pittsburgh Sleep Quality Index; PSQI) and daytime sleepiness (Epworth Sleepiness Scale; ESS) were assessed prior to deployment in 118 soldiers of the German army, who were deployed in Afghanistan for six months (deployment group: DG), and in parallel in 146 soldiers of a non-deployed control group (CG). Follow-up data are only available for subsamples (43.2% to 67.8% of the baseline sample). In the cross-sectional analysis, the DG showed higher prevalences of impaired sleep quality and increased daytime sleepiness than the CG.
Differences between the groups were significant during deployment with regard to the PSQI (36.8% vs. 24.5%), and before deployment in the ESS (25.7% vs.10.5%). The present results clearly indicate the need for more attention on the high prevalence of disturbed sleep and excessive daytime sleepiness in young soldiers, not only during and after deployment, but already during the pre-deployment training phase. Programs to teach techniques to improve sleep and reduce stress should be implemented prior to deployment to reduce sleep difficulties and excessive daytime sleepiness and subsequent mental disorders.
Keywords: Subjective sleep quality, PSQI, ESS, excessive daytime sleepiness, military deployment, prospective study
INTRODUCTION
Epidemiological studies show, that sleep disorders are very common in the general population. A study on health in German adults (DEGS1), which was conducted by the Robert-Koch-Institute on 8.152 adults in the age range from 18-79 years, revealed that approximately one third of the participants reported to have had potentially clinically relevant difficulties to fall asleep and to maintain sleep during the past for weeks [25]. Twenty percent of the study participants reported a bad sleep quality [25]. A study on sleep problems 12 months after return from deployment in soldiers of the German armed forces (n=1478) in comparison to non-deployed soldiers (n=880) indicated that 41% of the deployed population suffered from sleep disorders, and 38% of the control group HEINRICH et al. [12]. Therefore, sleep problems in German soldiers are independent from deployment and have a higher prevalence than in the general population.
Despite of a psychological preparation, deployment may lead to an increase in mental disorders [16]. Furthermore, traumatic events, which may occur during deployment, may lead to an increased risk of developing a Posttraumatic Stress Disorder [PTSD; 31]. A study of MCLAY et al. [18] it has been shown that insomnia symptoms, which were already present in soldiers prior to deployment, increased the score of PTSD severity significantly at follow-up assessment compared to soldiers, who did not initially report insomnia symptoms. That impaired sleep quality prior to deployment is a highly relevant predictor for developing psychiatric disorders, was also shown in the so-called Millennium Cohort study [7]. In that study, analysis of the data from 15.204 soldiers revealed that sleep-duration and insomnia symptoms prior to deployment were risk factors for the development of new-onset mental disorders after return.
In epidemiological studies, data on sleep is often gathered with non-standardized methods, e.g., single questions on sleep from non-specific questionnaires are used. The present study differs from previous studies on sleep in deployed soldiers as follows: 1) sleep quality and excessive daytime sleepiness were assessed by validated sleep questionnaires, 2) data was gathered not only prior and post deployment, but also during deployment, and 3) a comparison with a non-deployed control group of soldiers, who were studied in parallel at the same times of measurement, was made.
MATERIAL AND METHODS
Sample
The study sample consisted of two cohorts:
1.) 118 male soldiers of an infantry battalion, who were deployed to Afghanistan from July 2012 to January 2013 for an International Security Assistance Force (ISAF) operation (deployment group, DG),
2.) 146 at that time non-deployed male soldiers from another infantry battalion (control group, CG), who were studied according to the same time schedule.
Study design
The collection of data took place in both groups in parallel at three points in time: approximately six weeks prior to deployment (T0), during the deployment phase, at approximately three months after the beginning of deployment (T1), and directly after the end of the deployment (T2, approx. seven months after T0).
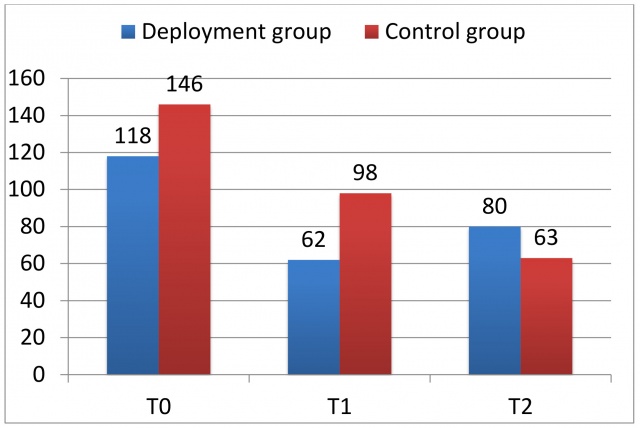 Samples for groups and different times of measurement (T0: prior to deployment; T1: during deployment; T2: after deployment)
Samples for groups and different times of measurement (T0: prior to deployment; T1: during deployment; T2: after deployment)
The sample sizes at different times of measurement for both groups are displayed in Figure 1. The figure shows that at the point of time T1 only 53% of the deployment group and 67% of the control group participated in the follow-up assessment. At T2 the corresponding numbers were 68% (DG) and 43% (CG) of the initial sample, respectively.
Measures
Depressive symptoms were assessed by the Patient Health Questionnaire-9 (PHQ-9), which is a self-rating questionnaire. The PHQ-9 is part of the Patient Health Questionnaire [PHQ-D, deutsche Version, 10], which belongs to the Primary Care Evaluation of Mental Disorders [PRIME-MD; 29]. The PHQ-9 covers the nine diagnostic criteria of depression of the Diagnostic and Statistical Manual of Mental Disorders [DSM-IV, 1] concerning the past two weeks. For further analysis data was dichotomised by two severity classes: < 5 (minimal) vs. ≥ 5 (mild to severe).
Somatic symptoms were evaluated by the module PHQ-15, which asks for 15 different somatic symptoms. The total score varies between 0 and 30. For the present data analysis, the severity of somatic symptoms was dichotomised by a total score of 5: < 5 (minimal) vs ≥ 5 (mild to severe).
Stress was measured by the corresponding ten items of the stress module of the Patient Health Questionnaire. For the present analysis total scores were categorised into two different severity classes:< 5 (minimal) vs ≥ 5 (mild to severe).
Daytime sleepiness was evaluated by the Epworth Sleepiness Scale [14], a validated instrument in sleep medicine to measure self-rated tendency of falling asleep (not only feeling tired) in eight everyday situations. The total score ranges between 0 and 24. A total score > 10 is considered to reflect an increased daytime sleepiness in the context of sleep medicine.
Sleep quality was measured with the Pittsburgh Sleep Quality Index [PSQI; 3], a self-rating questionnaire, which is comprised of 19 items. The global PSQI-score ranges from 0 to 21. A global score > 5 is indicative of a „poor“ sleep quality.
Statistics
In the statistical analyses the total scores of the questionnaires (ESS and PSQI) as well as ordinally scaled and dichotomized variables (ESS: ≤ 10, >10; PSQI: ≤ 5, > 5) were considered. Data analysis included 1.) differences in sleep variables between the deployment and the control group for all three times of measurement, and 2.) variations within groups, based on the cross-sectional data at the three times of measurement. c2-tests were applied to the dichotomized variables within as well as between groups. For the ordinally scaled data, differences in distribution between groups and within groups were analysed by Wilcoxon-2-sample tests and Wilcoxon’s k-sample tests, respectively. Cramers V was calculated to quantify the effect of dichotomous variables, whereas Cohen´s d was applied (for comparisons of two groups), and η2 (for more than two groups), respectively. Interpretation of effect sizes was made according to Cohen [5]. All tests were performed with a two-sided significance level of p < 0.05.Statistical analysis was performed SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
The characteristics of both samples are shown in Table 1 and 2. The deployment group and the control group differed significantly with regard to age, height and weight, but not BMI. Soldiers of the deployment group were older, taller, and had a greater weight (Table 1). Effect sizes are small (≥ 0.20 and < 0.50) for weight and age, and medium (≥ 0.50 and < 0.80) for height. Spearman rank correlations showed that with one exception sleepiness and sleep quality were not meaningfully correlated with these factors. All correlation coefficients ranged between -0.10 and +0.11 and were non-significant. An exception was that sleep quality worsened slightly but significantly with increasing age (r = 0.1361, p = 0.0318).
The distributions of rank, status, duration of the commitment period, graduation and living with a partner also differed significantly between the deployment and the control group (Table 2). The corresponding effect sizes were weak to moderate (Cramers’ V: ≥ 0.10 and < 0.40). In the deployment group the soldiers tended to have higher ranks, overall higher graduations, and more professional soldiers and less frequently volunteers. More subjects in the deployment group lived with partners and had a longer commitment period. The marital status was not different between groups (Table 2). The number of soldiers who had been deployed before was larger in the deployment group than in the control group (45.8 vs. 34.2%). The difference, however, was not statistically significant and showed a small effect size (Table 2). Further information on the number and duration of prior deployments was not collected.
The number of subjects with a bad sleep quality (PSQI-score > 5) as well as with excessive daytime sleepiness (ESS-score > 10) did not vary significantly with regard to rank, commitment period, graduation and living with a partner, and to whether the soldiers had been deployed before.
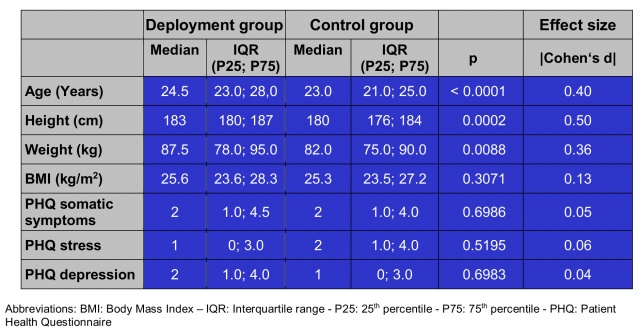 Basic sample characteristics for variables assessed at an ordinal scale. Comparisons between groups (deployment groups vs. control group).
Basic sample characteristics for variables assessed at an ordinal scale. Comparisons between groups (deployment groups vs. control group).
The only statistical difference was observed for status: Out of the professional soldiers 1 out of 3 showed an impaired sleep quality, in the group of regular soldiers the percentage was 25%, while in volunteers it was less than 5%. These differences were statistically significant (p = 0.0276). Effect sizes were weak for the association of sleep quality with rank, (Cramers V: 0.18), status and graduation (Cramers V: 0.15). For daytime sleepiness effect sizes were also weak for the associations with rank (Cramers V: 0.16) and with marital status (Cramers V: 0.15).
The samples were not different with regard to the Patient Health Questionnaire scores for somatic complaints, stress and depression at the baseline assessment T0 .
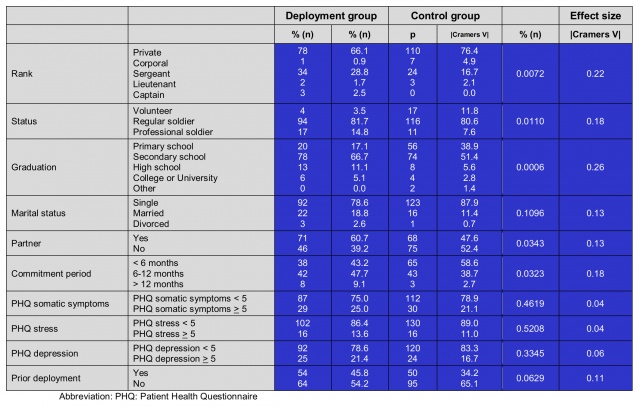 Basic sample characteristics for variables assessed at a categorial scale: Results of chi-square tests for comparisons of deployment group and control group.
Basic sample characteristics for variables assessed at a categorial scale: Results of chi-square tests for comparisons of deployment group and control group.
Epworth Sleepiness Scale
Boxplots of the distribution of the ESS-score by group and time of measurement are displayed in Figure 2. It shows that daytime sleepiness is higher at all times of measurement in the deployment group as compared to the control group. However, the difference reaches statistical significance only at baseline (T0: p = 0.0118) with a small effect size (d = 0.34). At the times of measurement T1 and T2 the effect was larger (T1: d = 0.42; T2: d = 0.40), but did not reach statistical significance due to the smaller sample size compared to T0 (T1: p = 0.0523; T2: p = 0.0526). The same tendency was seen with regard to the dichotomised parameter daytime sleepiness. The percentage of soldiers with a suspicious ESS-score (> 10) is higher in the deployment compared to the control group (see Figure 2). The increased percentage of daytime sleepiness is again statistically significant only at T0 (25.7% vs. 10.5%, p = 0.0014; Cramers V: 0.20).
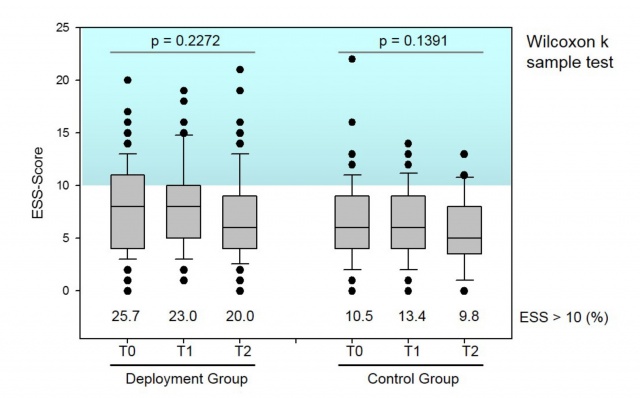 Boxplots of the distribution of Epworth Sleepiness (ESS) scores by group and time of measurement (T).
Boxplots of the distribution of Epworth Sleepiness (ESS) scores by group and time of measurement (T).
A within-group comparison of ESS-scores reveals that neither for the deployment group (p = 0.2272) nor for the control group (p = 0.1391) the degree of sleepiness varies significantly between the three times of measurements (Figure 2). The corresponding effect sizes indicate negligible associations (DG: η2 < 0.01, CG: η2 = 0.01). In the deployment group the percentage of subjects with increased daytime sleepiness varies between 20.0% (T2) over 23.0% (T1) to 25.7% (T0) (p = 0.6627). Therefore, during the preparation phase, daytime sleepiness is highest, and after the deployment it is lowest, but still far above the highest observed percentage in the control group (T1: 13.4%). In the control group, daytime sleepiness varies not significantly from 9.8% at T2 over 10.5% at T0 and 13.4% at T1 (p = 0.7267).
Pittsburgh Sleep Quality Index
The boxplots of the distribution of the PSQI-scores by group and time of measurement are depicted in Figure 3. It indicates that sleep quality is worse in the deployment group as compared to the control group at all times of measurement. However, differences in the distribution are only significant at T1 (T0: p = 0.0659, T1: p = 0.0281 and T2: p = 0.1795). Effect sizes are small at all time points (T0: d = 0.32; T1: d = 0.42; T2: d = 0.32). That sleep quality is worse in the deployment group is also reflected in a higher percentage of bad sleepers (PSQI-Score > 5; Figure 3).However, although the prevalences are markedly different, none of the differences is statistically significant at any time point (T0: p = 0.2587, T1: p = 0.1051 und T2: p = 0.2358). Effect sizes (Cramers V) varied between 0.07 (T0) over 0.10 (T2) to 0.13 (T1) and are therefore negligible or weak.
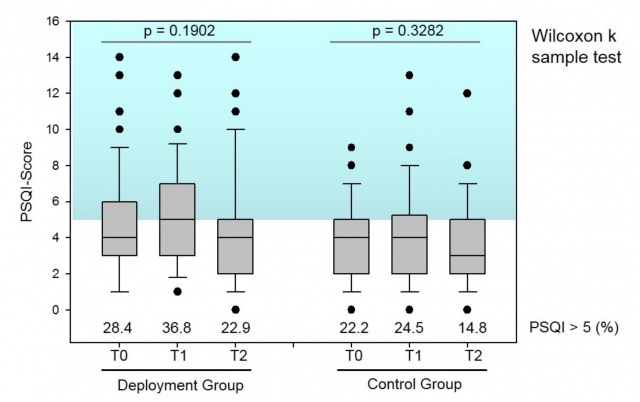 Boxplots of the distribution of Pittsburgh Sleep Quality (PSQI) scores by group and time of measurement (T)
Boxplots of the distribution of Pittsburgh Sleep Quality (PSQI) scores by group and time of measurement (T)
The percentage of bad sleepers varies between 22.9% (T2) and 36.8% (T1) in the deployment group and between 14.8% (T2) and 24.5% (T1) in the control group. Every third soldier of the deployment group had a PSQI-score which was indicative of a bad sleep. Differences between the times of measurements were not different in either group (DG: p = 0.2251; CG: p = 0.3099), effect sizes were 0.11 in the deployment group and 0.08 in the control group. A comparison of PSQI-Scores across all three times of measurements reveals that for both groups the variation of PSQI-Scores is not significantly different (DG: p = 0.1902, CG: p = 0.3282).
DISCUSSION
The aim of this study was to investigate sleep quality and daytime sleepiness prior, during and after deployment by applying questionnaires, which are validated in sleep medicine. Results were compared with data from a control group of soldiers, who were not deployed at that time.
At baseline (T0), the deployment group and the control group differed in several characteristics (see Table 1 and 2). The differences in the anthropometric variables (Table 1) correspond to the well-known north-south gradient in height in Germany [11, 13]. The soldiers of the deployment group were significantly older than the control group. The deployed soldiers had higher ranks, a higher percentage of professional soldiers, and a corresponding longer commitment period. Since sleep quality was more often impaired in the surveyed professional soldiers than in regular soldiers and volunteers, it must be assumed that higher age plays a role. The two groups did not differ with regard to health status as assessed by the modules stress, depressive and somatic symptoms of the Patients Health Questionnaire. The proportion of soldiers with at least mild depressive symptoms was not significantly higher in the deployed group (21.4%) compared to the non-deployed soldiers (16.7%). One explanation for this rather high percentage could be that a very sensitive group classification (score > 5) was applied. Stress symptoms were less prevalent, but affected more than 10% of soldiers in both groups to a moderate or higher level. All three PHQ-scores were significantly and positively correlated with the PSQI-score and the ESS-score. The correlations of the PSQI-score with PHQ-variables were: somatic complaints rS = 0.5404 (p < 0.0001), depressive symptoms rS = 0.5205 (p < 0.0001) and stress rS = 0.4358 (p < 0.0001). The correlations with daytime sleepiness were significant, but correlations were all below 0.2000: somatic complaints: rS = 0.1894 (p = 0.0026), depressive symptoms: rS = 0.1704 (p = 0.0065) and stress: rS = 0.1952 (p = 0.0017). The correlation of the PSQI- and the ESS-scores with somatic complaints and depressive symptoms, as assessed by the PHQ, is probably due to the fact that two of nine items which constitute the depression module (PHQ-9) refer to sleep (Item 2c “Trouble falling or staying asleep, or sleeping too much?”) or tiredness (2d “Feeling tired or having no energy”) are also considered in the somatic module (PHQ-15). The ten questions of the stress module, however, do not cover sleep and/or tiredness. This is an indication that stress is related to sleep problems and to a lesser extent to excessive daytime sleepiness.
The level of sleepiness was higher in the deployment group as compared to the control group, which is also reflected in nearly twice as high percentages of subjects with a score > 10 in the Epworth Sleepiness Scale in the deployment group. In this group, the lowest percentage was 20%, in the control group the highest percentage was 13.4%. The percentage of soldiers with an elevated ESS-total score was higher in both groups at all times of measurement compared to a reference value of 8.4% of healthy young men [24], and compared to 7.2% of a sample of 2.016 German adults [mittleres Alter ± Standardabweichung: 49.8 ± 18.2 Jahre; 28]. Hence, the proportion of soldiers with an elevated daytime sleepiness was up to three times higher in the deployment group than in the non-military samples [24, 28].
In a study of SHATTUCK and MATSANGAS [27] 69 active crewmembers of a USA Navy destroyer (age 21 - 54 years) completed the EpworthSleepinessScale, and their sleep was measured by actigraphs and sleep diaries for 11 days. Vigilance during the day was tested on a 3-min version of the Psychomotor Vigilance Test (PVT). Forty-two percent of the study population had elevated scores on the EpworthSleepinessScale (>10), and showed worse performance in the PVT. ESS scores were correlated negatively with time spent in bed. The authors concluded that the ESS was an indicator of personal sleep debt that varied depending on individual sleep requirement.
The increased daytime sleepiness, which was also observed in the present study in the deployment group, might in addition reflect a mode of exhaustion and of high physical and psychological demand, especially during the preparation phase for deployment and during deployment. found such an association between daytime sleepiness in the ESS, and poorer sleep quality in the PSQI, and the level of perceived stress in 350 adults, who took part in a cardiovascular disease prevention program. In the present study, similar correlations were observed although the association between stress (PHQ) and sleep quality (PSQI) was stronger than with daytime sleepiness (ESS).
Excessive daytime sleepiness (EDS) is a significant public health issue. Possible causes are different sleep disorders (sleep apnea or hypersomnia of central origin), side-effects of various medications, inadequate sleep-wake schedules (e.g., shift work) or a behaviourally induced insufficient sleep duration. The consequences of EDS are an increased risk for traffic accidents or accidents at the workplace, or impaired social functioning as well as a reduction of the quality of life [9, 17, 24]. Since soldiers have to deal with weapons and may be involved in operational scenarios up to combat missions, excessive daytime sleepiness in soldiers is a risk factor for their own as well as the health and lives of others. Therefore, military superiors and soldiers should be aware about possible negative consequences, and appropriate behavioural and structural adaptations should be intensified to reduce the risks resulting of excessive daytime sleepiness [please also refer to [30]]. In the present study, 36.8% of soldiers during deployment suffered from impaired sleep quality. This percentage was the highest value of both groups, and was significantly higher than the corresponding frequency of the control group. After return from deployment the proportion of soldiers with impaired sleep quality was still 22.9%. Shorter self-reported sleep durations and more sleep disturbances in deployed in contrast to a non-deployed control group were also observed by BAGNELL et al. [2].
Based on a study with 15,204 participants, who returned from their first deployment and filled in questionnaires twice at a distance of seven years (2001 and 2008), GEHRMAN et al.[7] concluded that sleep duration and the presence of insomnia symptoms were risk factors for the new-onset of mental health disorders following deployment. Cognitive Behavioural Therapy in Insomnia (CBT-I) on return of deployment are recommended as a treatment option to reduce mental problems [4].
Reference values on the Pittsburgh Sleep Quality Index, which were gathered from the general population, is hardly available. In an Austrian study, the prevalence of poor sleepers (PSQI score > 5) was 32.1% [32]. The sample was comprised of 1,049 subjects, who were at least 15 years old (average approximately 43 years). The authors reported that the percentage of poor sleepers increases with age and is generally higher in women than in men. The difference was greatest between females and males in the age categories from 15 to 35 years (21.5% vs. 14.1%). In the present study, the proportion of poor sleepers at baseline (T0), i.e. before deployment abroad, was 28.4% in the DG and 22.2% in the CG, and was therefore clearly higher than the 14.1% of the corresponding male age category of the Austrian study. Therefore, the prevalence of 36.8% of soldiers with impaired sleep quality, which was observed during deployment in the deployment group, was very high and exceeds the normative values of the Austrian study by far.
Compared to the frequencies of soldiers with a poor sleep quality (PSQI>5) studied by HEINRICH et al. [12] the percentages of the present sample were only minimally lower: 41% of n = 1.478 deployed soldiers and 38% of n = 880 non-deployed soldiers. The higher values in HEINRICH et al. [12] are probably to some parts a result of the higher age of the samples: 30.8 ± 7.7 years (deployed), and 30.0 ± 8.4 years (non-deployed). In the present study participants were on average four years (deployment group: 26.1 ± 5.3 years), and 24.1 ± 4.8 years (control group), respectively. Furthermore, the percentage of women was 5% in both samples, whereas in the present study only men were represented. Since women usually show a higher frequency of impaired sleep [32], the higher percentage of women in the study of HEINRICH et al. [12] could have led to a greater proportion of individuals with a bad sleep quality. A similar result was found in a study on soldiers with a mean age of 29.1 years, who had been deployed in Afghanistan and Iraq, respectively [18]: 41% reported some degree of sleep problems.
Limitations
The drop-out rate of the present study was rather high. While the number of study participants in the control group decreased continuously, the number of participants was lowest during deployment in the deployment group (53% of the baseline value). A possible explanation might be the deployment specific situation. Deployment-related burden as well as organisational reasons could be a reason for the lowest value of participants during deployment. For both groups it has to be considered that the PSQI with 19 questions in total is rather lengthy and therefore vulnerable to incomplete datasets.
Conclusions
Based on the results of a study on sleep and health resilience on a large military cohort (n = 55,012), SEELIG et al. [26] underscore the importance of sufficient sleep, since in their study, the presence of insomnia symptoms was associated with lower self-rated health and negative impacts on work and deployment abroad. GILBERT et al. [8] in their review claim that sleep is understudied in veteran populations. They underline the necessity to evaluate and treat sleep problems in PTSD (and traumatic brain injury) as an integral part of clinical management of both. PEDERSEN et al. [19] go one step further by recommending to shift the focus of military sleep research from the post-deployment period to the development of sleep health policies, and to the evaluation of sleep health programmes to promote physical and psychological health, and resilience to stress after deployment.
The present study results emphasize the need for prevention programs in soldiers already before deployment. In addition, treatment strategies like Cognitive Behavioral Therapy in Insomnia (CBT-I) should be available after return from deployment for those who suffer from impaired sleep. Prevention as well as diagnostic and therapeutic programs should be implemented to prevent psychiatric disorders and impaired health in military personnel. Appropriate programs should not only be offered after deployment, but already during the preparation phase for deployment.
In this context, the development of a sleep-coaching program for the German armed forces needs to be mentioned, which was developed within the framework of the Occupational Health Management of the German armed forces by CS and HDH. In the pilot study it became already evident that “measures of well-being”, “self-care-behavior”, and “self-care awareness” are positively influenced by sleep-coaching [20, 21]. In a subsequent project, the sleep-coaching program, which comprises four 90-min face-to-face group sessions, was implemented for the German armed forces by a clinical- and health psychologist and somnologist (CS) at four different sites. The study design corresponded to a waiting control group design. The evaluation of sleep was performed by applying ambulatory polysomnography and by questionnaires at the following four time points in both groups: a) prior to the first intervention, i.e. before the treatment group or the waiting group participated in the sleep-coaching program (t0), b) after the end of the first intervention, i.e. after participation of the treatment group in the sleep-coaching program (t1), c) after the end of the second intervention, i.e. after participation of the waiting control group in the sleep-coaching program (t2), and d) approximately three months after the end of participation in the sleep-coaching by answering questionnaires only (t3).
Participation in the sleep-coaching program led to an improvement in sleep quality at the objective as well as at the subjective level. Further positive consequences comprised a reduction of depressive and somatic symptoms measured by the PHQ. Hence, sleep-coaching is a preventional intervention option, which leads to stable effects with at the same time relatively few ressources [22, 23].
For the dissemination of the sleep-coaching, 37 psychologists of the German armed forces were trained on sound practical implementation of the program. An intra-net based version of the sleep-coaching (i-SCO) is currently developed and will be evaluated in a research project. For an overview of the development, implementation and evaluation of the sleep-coaching program for the German armed forces, reference is made to [6].
Core Statement
- Sleep disturbances and daytime sleepiness in the German armed forces are frequent phenomena
- They occur particularly frequently in soldiers during deployment. In this group, a significant difference between both time points prior and during deployment compared to a military control group at home was observed.
- Therefore, sleep disturbances especially before deployment imply a problem for psycho-physiological fitness of soldiers.
- From a preventive and psychotherapeutic perspective, the development and implementation of targeted measures to improve sleep in the German armed forces are required.
REFERENCES
- American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR. 4th Edition, Text Revision. 2000, Washington, DC: American Psychiatric Publishing.
- Bagnell ME et al.: The association of predeployment and deployment-related factors on dimensions of postdeployment wellness in U.S. military service members. Am J Health Promot 2013; 28(2): e56-66.
- Buysse DJ et al.: The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28(2): 193-213.
- Capaldi VF et al.: Insomnia in the Military: Application and Effectiveness of Cognitive and Pharmacologic Therapies. Curr Psychiatry Rep 2015; 17(10): 85.
- Cohen J: Statistical power analysis for the behavioral sciences. 1988, Hillsdale: Lawrence Erlbaum Associates Inc.
- Danker-Hopfe H et al.: Development, implementation, and evaluation of a sleep coaching program for the German armed forces. Somnologie 2017: 1-8.
- Gehrman P et al.: Predeployment Sleep Duration and Insomnia Symptoms as Risk Factors for New-Onset Mental Health Disorders Following Military Deployment. Sleep 2013; 36(7): 1009-1018.
- Gilbert KS et al.: Sleep disturbances, TBI and PTSD: Implications for treatment and recovery. Clin Psychol Rev 2015; 40: 195-212.
- Goncalves M et al.: Sleepiness at the wheel across Europe: a survey of 19 countries. J Sleep Res 2015; 24(3): 242-53.
- Gräfe K et al.: Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)“ [Screening for psychiatric disorders with the Patient Health Questionnaire (PHQ). Results from the German validation study] (in German). Diagnostica 2004; 50(4): 171-181.
- Heineck G: Height and weight in Germany, evidence from the German Socio-Economic Panel, 2002. Econ Hum Biol 2006; 4(3): 359-82.
- Heinrich A et al.: Schlafprobleme bei Soldaten und die Rolle traumatischer Ereignisse bei Auslandseinsätzen. [Sleeping problems of German soldiers and the role of deployment-related traumatic events] (in German). Z Klein Psychol Psychother 2015; 44(2): 121-130.
- Hiermeyer M: Height and BMI values of German conscripts in 2000, 2001 and 1906. Econ Hum Biol 2009; 7(3): 366-75.
- Johns MW: A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540-5.
- Kashani M, Eliasson A, Vernalis M: Perceived stress correlates with disturbed sleep: a link connecting stress and cardiovascular disease. Stress 2012; 15(1): 45-51.
- Kowalski JT et al.: Deployment-related stress disorder in german soldiers: utilization of psychiatric and psychotherapeutic treatment. Disch Arztebl Int 2012; 109(35-36): 569-75.
- Mathis J, Schreier D : Tagesschlafrigkeit und Fahrverhalten. [Daytime sleepiness and driving behaviour] (in German). Ther Umsch 2014; 71(11): 679-86.
- McLay RN, Klam WP, Volkert SL: Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med 2010; 175(10): 759-62.
- Pedersen ER et al.: Increasing resilience through promotion of healthy sleep among service members. Mil Med 2015; 180(1): 4-6.
- Röttger S et al.: Sleep coaching: An effective measure for workplace health promotion. (submitted) 2017.
- Röttger S et al.: Evaluation eines Schlafcoaching-Programms im Rahmen der Einführung des Betrieblichen Gesundheitsmanagements (BGM) in die Bundeswehr. Somnologie - Schlafforschung und Schlafmedizin 2016; 20(Suppl.): S.44.
- Sauter C et al.: Machbarkeit und Evaluation eines vierwöchigen Schlaf-Coaching-Angebots. Somnologie - Schlafforschung und Schlafmedizin 2016; 20(Suppl.): S.44.
- Sauter C et al.: Sleep coaching - a new method to improve impaired sleep in a workplace health promotion program of the German Armed Forces. (in preparation) 2017.
- Sauter C et al.: Normative values of the German Epworth Sleepiness Scale. Somnologie - Schlafforschung und Schlafmedizin 2007; 11(4): 272-278.
- Schlack R et al.: Haufigkeit und Verteilung von Schlafproblemen und Insomnie in der deutschen Erwachsenenbevolkerung: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). [Frequency and distribution of sleep problems and insomnia in the adult population in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)] (in German). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013; 56(5-6): 740-8.
- Seelig AD et al.: Sleep and Health Resilience Metrics in a Large Military Cohort. Sleep 2016; 39(5): 1111-20.
- Shattuck NL, Matsangas P: Psychomotor vigilance performance predicted by Epworth Sleepiness Scale scores in an operational setting with the United States Navy. J Sleep Res 2015; 24(2): 174-80.
- Soldatos CR et al.: How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med 2005; 6(1): 5-13.
- Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282(18): 1737-44.
- Stark R: Wenn im Dienst die Augen zufallen – zwei Fälle von Tagesschläfrigkeit [Drooping Eyelids when on Duty - Two Cases of Daytime Sleepiness]. Wehrmedizinische Monatsschrift 2017; 61(6): 118-126.
- Wittchen HU et al.: Traumatische Ereignisse und posttraumatische Belastungsstörungen bei im Ausland eingesetzten Soldaten. Wie hoch ist die Dunkelziffer? [Traumatic experiences and posttraumatic stress disorder in soldiers following deployment abroad: how big is the hidden problem?] (in German). Dtsch Arztebl Int 2012; 109(35-36): 559-68.
- Zeitlhofer J et al.: Sleep and quality of life in the Austrian population. Acta Neurol Scand 2000; 102(4): 249-57.
a German Armed Forces Office, Applied Military Psychology and Research Division, c/o University of the Federal Armed Forces Hamburg, Germany
b Asklepios Fachklinikum Teupitz, Department of Psychiatry and Psychotherapy, Teupitz, Germany
c Asklepios Fachklinikum Lübben, Department of Psychiatry and Psychotherapy, Lübben, Germany
d Department of Psychiatry and Psychotherapy, Campus Charité Mitte – Charité Universitätsmedizin Berlin, Germany
Conflict of Interest
This work has its origin in a non-third-party-financed cooperation between the Department of Psychiatry, Psychotherapy and Psychotraumatology at the Bundeswehr Hospital Berlin and the Competence Centre of Sleep Medicine at the Campus Benjamin Franklin, Charité – Universitätsmedizin Berlin. The authors declare no conflict of interest.
For all authors:
Prof. Dr. Heidi Danker-Hopfe
Kompetenzzentrum Schlafmedizin
Charité – Universitätsmedizin Berlin
Hindenburgdamm 30, 12200 Berlin
E-Mail: [email protected]
This article is also available in German.
Date: 11/02/2017
Source: Wehrmedizinische Monatsschrift 11/2017











