Article: M. Ph. KEILBERTH, Ch. NICLAS, Ch. SPARWASSER (GERMANY)
Renal Trauma
Actual Aspects of Diagnostics and Treatment
At first glance, the therapeutic algorithm for renal trauma seems to be simple –hemodynamic instability, entire organ-destruction, avulsion of the renal hilus or severe complications, all require an operative intervention. An indication for conservative treatment is a stable patient with a structurally preserved anatomy of the kidney, which is found in most cases of blunt renal trauma. However, a "gray area" exists where it may be difficult to decide which grade of renal injury can be managed conservatively and which one requires surgical intervention. This article highlights difficulties with classification and therapeutic decision of renal injuries as well as the question how to facilitate the decision-making.
Introduction
Over recent years there has been a paradigm shift in the treatment regimes of acute renal trauma; while renal injuries were in the past very often treated surgically, nowadays some even more serious renal injuries are being treated conservatively - without any increase in the occurrence of complications [1, 2, 3, 16].
There is no doubt, however, regarding the indication for the surgical treatment of haemodynamically unstable patients with renal injuries or patients with the most severe renal injuries and organ destruction. Assessing which of the more serious renal injuries can be treated conservatively and therefore without further trauma, without causing any additional morbidity for the patient is a major challenge, especially in acute situations in the trauma room. This is due not least to the many influencing factors that can determine the progress and ultimately the treatment of a renal injury - including the distinction between blunt and penetrating renal injuries, the presence of concomitant injuries and vascular involvement.
Epidemiology
Around 250,000 renal injuries occur each year worldwide [3, 4]. They affect mostly younger people (70 - 80 % of patients with renal injuries are < 44 years of age) [3, 5]. The main causes are road traffic accidents, sporting accidents, work-related accidents and criminal violence.
In the context of all injuries, renal trauma is somewhat rare due to the protected, retroperitoneal location of the kidneys. Only 2 - 5 % of (poly-)traumatised patients also suffer a kidney injury [3, 5]. Given the protected location of the kidneys, they are usually only injured following major external force and are therefore also frequently associated with injuries to other organ systems (20 - 94 %) [8].
Since the Vietnam war, military medicine has also undergone a significant change in terms of the incidence of renal injuries. The use of safety vests has meant a significant drop in the number of kidney injuries to date. While in Vietnam 32 % of all urogenital trauma involved the kidneys, this figure was only 17 % in the Gulf war. This is highlighted further by the percentage of renal injuries (33 %) compared to the total number of urogenital injuries sustained by Kuwaiti soldiers during the Gulf war, who did not have access to adequate safety vests [6, 7].
Classification of renal injuries
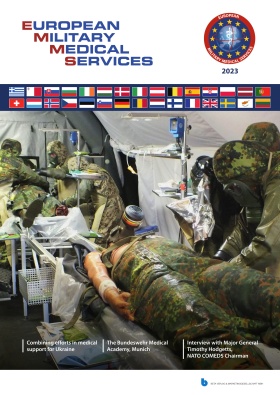
The American Association for the Surgery of Trauma took a key step in the classification of renal injuries in 1989 with the development of a five-stage Organ Injury Severity Scale for the kidneys.(AAST) (3). Recently, the recommendations for diagnostic procedures and treatment have been based on this classification system (see Tab. 1, Fig. 1) [10].
 Fig. 1: Classification of renal injuries.
Fig. 1: Classification of renal injuries.
| Grade | Type | Description |
| I | Contusion Haematoma | Micro-/macro-haematuria, imaging unremarkable Subcapsular and stable, no laceration |
| II | Haematoma Laceration | Perirenal / stable, limited to perirenal retroperitoneum < 1 cm depth of the parenchymal tears, no urine extravasation |
| III | Laceration | > 1 cm depth of the parenchymal tears, no involvement of the renal pelvicocaliceal system, no urine extravasation |
| IV | Laceration Vascular injury | Extends to the medulla and renal pelvicocaliceal system Renal artery / vein injury with stable haematoma |
| V | Laceration Vascular injury | Complete renal destruction Hilar avulsion, kidney no longer perfused |
Tab. 1: Classification of renal injuries.
Diagnosis
The patient's condition determines the nature and timing of diagnostic procedures. Note should be taken first of all of any external signs of renal injury, such as flank haematoma, flank pain, rib fractures or entry / exit wounds in the abdominal or flank area. The cause of the accident can also provide vital information. In case of high-speed or deceleration trauma, for example, or following a fall from a great height, the possibility of renal injury must always be considered.
Urine testing
Haematuria - microscopic or macroscopic - is a very common symptom of renal injury. In (poly-)traumatised patients in the trauma room, a finding of haematuria must always raise the suspicion of injury to the urogenital tract and therefore also of injury to the kidneys.
Haematuria is not always present in renal injury, however. Severe, grade IV/V injuries especially demonstrate no evidence of haematuria in up to 18 % of cases [3, 5].
Computer tomography (CT)
Provided the patient is stable enough, CT is regarded as the gold standard for diagnosing renal injuries.
The aim of imaging is to
correctly categorise and classify the renal injuries
diagnose potential pre-existing renal pathologies
assess renal function (on the respective sides)
evaluate likely concomitant injuries (in up to 90 % of cases) [14]
In response to the question "CT yes / no?", classification into blunt and penetrating renal injury must first be carried out. If the constellation of findings raises the suspicion of penetrating injury, a CT is always indicated (provided it is available and the patient's condition permits it). If there is a suspicion of blunt renal trauma, the procedure set out in Fig. 2 should be followed. The rationale for this procedure is the fact that patients with renal trauma with just micro-haematuria and a systolic blood pressure of > 90 mmHg have a significant renal injury in only 0.2 % of cases [13, 14]. If the patient's condition does not permit a CT scan because he or she must be taken into theatre immediately, a one-shot intravenous pyelogram can be carried out during surgery.
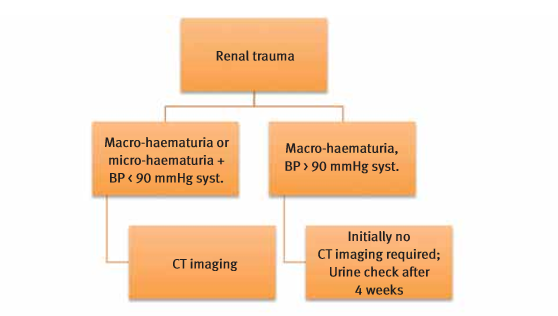 Fig. 2: Flow chart - imaging in the diagnosis of blunt renal injuries.
Fig. 2: Flow chart - imaging in the diagnosis of blunt renal injuries.
It is important for CT diagnostic purposes that it includes an early arterial phase, in order to assess the extent of the renal injury and also to possibly reveal any active bleeding present. On the other hand, CT diagnosis - where possible - should also include a urographic phase approx. 10 - 20 minutes after the administration of contrast medium in order to visualise injuries to the renal pelvicocaliceal system with contrast medium extravasations.
Re-evaluation with CT imaging is only recommended for grade IV and V injuries [3, 14]. This should generally be carried out 36 - 72 hours after the trauma. Grade I - III injuries do not normally require CT re-evaluation, provided the patient is stable and the kidneys are intact. Figures 3 and 4 show a grade I injury and a grade IV injury. Figure 3 also shows a blood-filled liver as a manifestation of a concomitant injury.
Intravenous pyelogram (IVP)
If a CT scanner is available, IVP is no longer relevant for acute diagnostic purposes in the trauma room since it has significantly less informative merit compared to CT. The positive predictive value for the presence of renal injury is between 65 and 95 % for IVP [14]. Grade IV injuries of the kidney remain undetected in up to 25 % of cases on IVP [11]. Nowadays, IVP only offers benefits in the diagnosis of renal injuries when used intraoperatively as a "one-shot IVP" where CT scanning was not possible, for example due to the patient being haemodynamically unstable and requiring immediate laparotomy. The procedure involves an X-ray 10 - 20 minutes after the IV bolus administration of contrast medium (2 ml / kg). This allows to assess the function of the contralateral, uninjured kidney, the injured kidney, any urine extravasation or dystopic renal position.
 Fig. 3: Grade I injury (contusion) of the right kidney and injury to the liver.
Fig. 3: Grade I injury (contusion) of the right kidney and injury to the liver.
Ultrasound
Ultrasound plays a secondary role in the precise diagnosis and in particular classification of renal injuries. However, in orientational diagnostic procedures in the trauma room ("first assessment" / "FAST" (Focused Assessment with Sonography for Trauma")), ultrasound has high importance. Ultrasound can at least offer indicators as to the presence of renal injury. It is used as a tool when answering the question of whether or not further exploration with CT is required.
Ultrasound also plays a major role in the assessment of progress in the development of urinomas, haematomas or urinary retention.
MRI
G
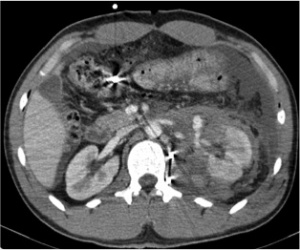 Fig. 4: Grade IV injury with deep laceration and haematoma of the left kidney.
Fig. 4: Grade IV injury with deep laceration and haematoma of the left kidney.
iven the long duration of the procedure, MRI is not an option for the acute diagnosis of renal injuries and struggles to demonstrate possible urine extravasations [14]. A pre-existing allergy to contrast medium, for example, is another contraindication.
Angiography
In the age of CT scanning, angiography is no longer a primary diagnostic tool in the diagnosis of renal injuries; however, it is pioneering and essential in the context of radiological interventions performed for haemostasis with embolization.
Treatment
Looking back over recent years/decades, a trend has become apparent moving away from surgical treatment towards the minimally invasive or purely conservative management of renal injuries.
If both of a patient's kidneys are injured, or if a solitary kidney is affected, attempts must always be made to save an injured kidney [3].
Conservative treatment of renal injuries
Grade I - III renal injuries are almost always treated conservatively. It is only when a patient with a grade III injury becomes unstable that intervention is indicated in this group.
Over recent decades, however, grade IV / V injuries have increasingly also been treated conservatively, resulting in a reduction in the number of nephrectomies performed [1, 3, 15, 16]. In conservative management, the following procedure is recommended [3]:
CT re-evaluation 36 - 72 hours following the trauma for grade IV and V injuries.
Intensive care monitoring for grade IV and V injuries.
Bed rest until clinical stabilisation or until any macro-haematuria present subsides.
Antibacterial prophylaxis/treatment - be aware of the haematogenic spread of bacteria with indwelling urinary catheters and/or IV accesses (secondary infection of primarily sterile urinomas or haematomas) [17].
Physical protection and avoidance of physical exertion for at least six weeks following the trauma.
According to information contained in literature, around 7 % of renal injuries that were initially treated conservatively eventually require surgical treatment. Failure of conservative measures is usually evident within the first 24 hours following the trauma. Much more important, however, is the realisation that none of the patients who were initially treated conservatively and then still went on to have surgery as a result of failure of the initial therapeutic approach sustained any additional harm [16].
Urine extravasations or urinomas that can occur in the context of renal injuries resolve spontaneously in 70 - 90 % of cases. Interventional procedures such as nephrostomy or ureteric stents are therefore only required in exceptional cases (e.g. superinfection, persistent/progressive urinoma) [20].
Surgical treatment of renal injuries
Few situations require immediate surgical treatment. Those that do include active, persistent bleeding demonstrated through imaging in patients who are haemodynamically unstable, a retroperitoneal haematoma which is growing in size and renal pedicle avulsion [3]. If the patient's condition necessitates immediate surgical laparotomy without imaging and an expansive retroperitoneal haematoma is discovered during the procedure, exploration of the affected kidney is also indicated [3].
Where there are penetrating injuries of the kidney also, more recent literature has demonstrated a trend towards a conservative approach to treatment, provided there is no absolute indication for surgery [3]. For many more severe injuries that do not require immediate surgical intervention, embolisation of the affected renal vessels can achieve adequate haemostasis. However, this technique is not available in the field.
 Fig. 5: Surgical specimen of a grade V renal injury.
Fig. 5: Surgical specimen of a grade V renal injury.
Generally speaking, as the severity of the injury increases, the nephrectomy rate also rises sharply. According to Aragona et al. [1], the nephrectomy rate in the group of grade III injuries is lowest at 9 % and highest in the group of grade V injuries at 83 %, as expected. According to these figures, grade IV injuries are associated with a nephrectomy in 22 % of cases (see Fig. 5).
Since today more severe renal injuries are also being successfully treated with conservative measures, criteria need to be found that make it easier to decide in favour or against surgical intervention for the treatment of renal injuries. One option is to classify them into low-risk and high-risk injuries by adding in other risk factors independent of the classification described above. The sub-classification of grade IV injuries into low and high risk would be of benefit in this context since this group represents a 'grey area' in which both conservative and surgical therapy have equal merit [8, 11]. In a small, retrospective study, this approach to classification demonstrated that, as the number of risk factors increases (haematoma > 3.5 cm, contrast medium extravasation from vessels and complex lacerations), the likelihood of surgical intervention increases markedly [12]. Another study demonstrated that, in cases where the mechanism of injury involved road traffic accidents or where patients with renal trauma were older than 55 years of age, conservative treatment failed significantly more often and eventually required surgical intervention [16].
Such an approach with different possible indicators could therefore be useful in the decision-making process deciding on conservative or interventional therapy.
Key steps in the surgical treatment of renal injuries include:
Exposure of the kidney - always in its entirety, so not to miss any injuries
Debridement / necrosectomy - dead tissue harbours the risk of infection
Bleeding control through ligature of vascular injuries
Oversuturing of the opened renal pelvicocaliceal system ("water-tight" closure)
Renorrhaphy, renal pole resection to treat renal lacerations with the aim of preserving the kidney
Interposition e.g. of omentum to compartmentalise the kidney and avoid later complications such as fistulas in the case of complex injuries (additional injury e.g. of the intestine, pancreas, stomach).
Some authors recommend vascular control as the first step in the surgical management of renal injuries in order to stop bleeding and therefore create a clear field of view for exploration and, where possible, repair of the kidney [3, 10, 11, 18]. This approach also allows existing abdominal injuries to be evaluated and treated more effectively in up to 90 % of cases.
The median laparotomy should be chosen as the access route for this procedure (see Fig. 6). The retro-peritoneum is incised directly over the aorta above the branch of the inferior mesenteric artery and the incision extended to the suspensory muscle of the duodenum. This exposes the renal vessels for any vascular assessment that may be required [10, 18]. In cases of injuries to the arteries of the renal pedicle, revascularisation procedures with repair of the artery are not recommended [3, 19] since their percentage failure rate is too high; also, they are very time consuming and can consequently further increase the morbidity of patients with renal injuries. Exceptions to this rule are of course solitary kidneys and bilateral renal injury. If vascular repair is indicated, the ischaemia time limit of two hours must be kept in mind. Beyond this limit, the success of revascularisation is highly unlikely [3].
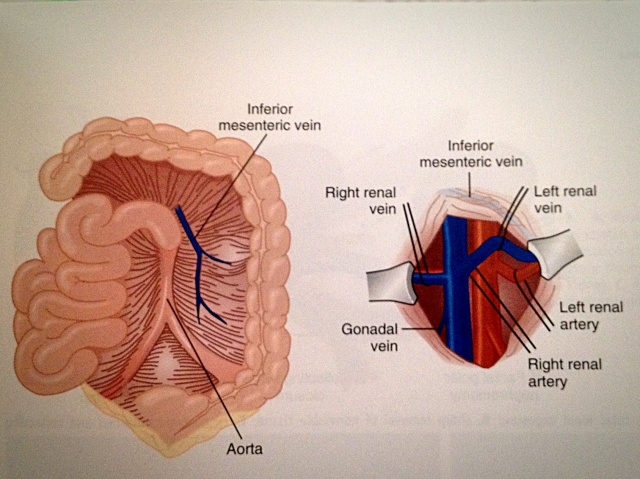 Fig. 6: Vascular assessment via a median laparotomy
Fig. 6: Vascular assessment via a median laparotomy
For injuries to the segmental arteries, embolization should be considered as the treatment of choice.
Angiography / embolization
Highly selective embolization of bleeding branches of the renal arteries demands a high degree of radiological expertise, which is not always available, and is a highly effective, minimally invasive means of arresting haemorrhagic renal injuries. The goal of haemostasis is achieved in 70 - 80 % of cases. Where successful, there is a significantly lower rate of loss of the injured kidney compared to surgical treatment [3, 14]. To achieve the goal of haemostasis, however, secondary interventions are commonly (80 - 90 %) required [3, 12].
Complications
Possible complications of renal injuries will be only touched upon here and include:
(Infected) urinoma, urinary fistula, perinephric abscesses
Arterial (renal) hypertension
AV fistulas with the risk of secondary haemorrhages (even decades after the original trauma)
Renal failure - at least 1/6 of the kidney must be preserved in the course of the treatment of renal injuries in order to prevent progressive glomerulosclerosis and therefore progressive functional impairment of the affected kidney [14].
Often, the only solution to treat renal hypertension resulting from renal trauma is nephrectomy.
Consequences
CT scanning - a diagnostic tool also available in most of the areas in which the German Armed Forces operate - is the gold standard in the diagnosis of renal injuries.
Wherever possible, a conservative approach to the treatment of renal injuries should be aimed for - regardless of the severity of the injury
Radiological renal artery embolization - if available - plays an important role in the primary treatment of more severe renal injuries
In terms of the rate of later complications, conservative and surgical approaches do not differ significantly. Where possible, a conservative approach should be preferred in view of the more likely preservation of the kidney.
The decision in favour or against a conservative / surgical approach could in future be made easier through the use of indicators and risk factors. However, relevant indicators require further checks through prospective studies.
Mathias Philip Keilberth, Christoph Niclas, Christoph Sparwasser
From the Department of Urology (Senior Physician: Colonel Professor Dr. C. Sparwasser) of the Armed Forces Hospital in Ulm (Lead Clinician: Brigadier General Dr. A. Kalinowski)
Date: 02/03/2015
Source: MCIF 1/15