
Article: Brig (Dr) Harjinder s Bhatoe M, Ch
Prehospital Algorithm in Gunshot Injuries of the Brain
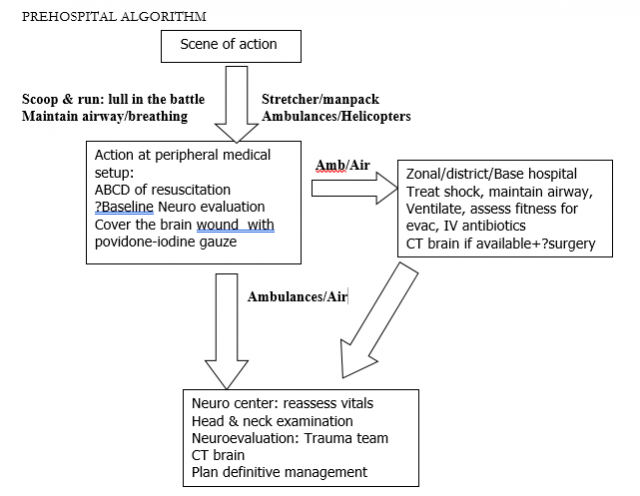
Immediate care rendered to a patient with craniocerebral missile injury (CMI) depends upon the place of injury (roadside accident site or battlefield, rural or urban setup, etc) and consequently the resources available at the nearest medical setup. A sniper or an assassin deliberately aims at the head to ensure death or at least permanent disablement. On the other hand, soldiers in the battlefield are likely to sustain CMI due to high velocity missile (HVMs) as well as low velocity missiles (LVMs); here the CMI is generally part of polytrauma involving neck, chest, abdomen, pelvis and limbs. Since HVMIs are largely incompatible with life, survivors are few and those who do so, would have sustained grazing injury. Most of the survivors would have sustained injury due to LVM. In the civilian CMIs, the missile is often a shotgun or a country-made weapon (katta), and the injury is generally due to LVMs. Injury due to exploding devices are being seen more often in violence in urban areas or in areas with armed militancy. These devices generally inflict multiple missile injuries to the head and neck.
TRIAGE AND ACTION AT THE SITE OF INJURY:
DEALING WITH MASS CASUALTIES
In a battlefield scenario, treatment of CMI begins at the site of injury, with basic first aid, application of shell dressing by the paramedics or other soldiers. The patient is then transported to the regimental aid post (RAP) located close to the forward defended location, where he is evaluated first time by a physician. Airway should be cleared and respiration supported by mouth to mouth breathing if necessary. Since immediate apnoea may be reversible, it is important that his fact is understood by paramedics, police and fire personnel and other people capable of rendering first aid. Open wounds are covered and the patient should be transported in three quarters prone position, so that the oropharynx remains clear of secretions and tongue falling back. “Scoop and run” as a policy has much to recommend in such a situation. During war and in a war-like scenario, casualties are multiple and there may be a delay of hours before medical aid can reach the injured depending upon the intensity of the battle. Once there is a lull in the battle, the casualties are collected and prioritized. The term ‘triage’ is derived from the French word trier meaning “to sort” and was anglicized after the Napoleonic wars. The practice of triage creates a situation whereby the greatest good for the greatest number can be accomplished. The four-tiered triage system (Table 2) was evolved during the Korean War. This lead to significant improvement in survival among the war-wounded soldiers (Hughes 1976). Triage may be based on physiological parameters or on those based on anatomical factors and mechanism of injury. Physiology-based triage systems manage patients with current clinical instability, while anatomy-based systems are used to identify those patients who have potential for deterioration and may require early surgery (Garner et al 2001). Various triage scoring systems used are summarized in Table 3. Garner et al (2001) retrospectively reviewed four trauma classification schemes (CareFlight, Simple triage and Rapid Treatment, modified Rapid Triage and Rapid Treatment, Triage Sieve). They found that the motor component of GCS and systolic blood pressure were strongest physiological predictors associated with critical injury.
After stabilization and resuscitation, patient is evacuated to the next echelon in the chain of evacuation, the advanced dressing station (ADS). Transfer to forward surgical section (FSC) is affected by ambulances, where basic surgical care is rendered. Evacuation to neurosurgical centre is undertaken by ambulances and helicopters. The intervention undertaken at each of these echelons depends upon the resources of the military units they care for. CT scan and facilities for neurosurgical procedures are generally available at rear echelon facilities (Base/Command Hospitals). Unlike closed head injury due to roadside accident, CMI in civilian or services set up elicits panic and shocked disbelief among the people around, which leads to loss of vital moments when the patient is potentially salvageable during the period of apnoea. Our resources in civil still do not match the recommended ‘Golden Hour’ concept. Most of the civilian CMIs reach neurosurgical care between 16 and 24 hours after the injury; partly the delay is due to poor transportation facilities in the rural hinterland of India and partly to the medicolegal procedures involved (Ramesh et al 2001). In the services setup, there is progressive shortening of the period of evacuation to a neurosurgical center due to better transportation facilities including availability of helicopters when required.
Table 1: Chain of evacuation in battlefield
| Level | Role |
|---|---|
| RAP ADS FSC Base/Command Hospital | Expert first-aid ‘ABC’ of resuscitation Life and limb saving surgical intervention Neurosurgical care |
Abbreviations: RAP – Regimental aid post, ADS – advanced dressing station, FSC – forward surgical section
An account of immediate condition of President Abraham Lincoln after he was shot in the head by John Wilkes Booth, was provided by Capt (Dr) Charles Leale, an Army Surgeon, seated about 40 feet from Lincoln:
I commenced to examine his head (as no wound near the shoulder was found) and soon passed my finger over a large, form clot situated about one inch below the superior curved line of the occipital bone. The coagula I easily removed and passed the little finger of my left hand through the perfectly smooth opening made by the ball…..
He was able to regain a pulse and started breathing again.
Table 2: Priority in management:
| Priority | Description |
|---|---|
| PI PII PIII PIV | Patient requiring immediate resuscitation Patients requiring early surgery Walking wounded Moribund patients, unlikely to survive |
Table 3: Triage Scoring systems (Wiseman et al 2002)
| Scoring system | Parameters |
|---|---|
Trauma index
Neuropsychiatric triage
Mechanisms of injury | injury type, respiratory, cardiovascular & CNS based on modified simple triage & rapid treatment respiratory rate & level of consciousness systolic BP <85 mm Hg, GCS motor <5,
Loss of limb/functional cosmesis, mangled remains penetrating wounds to chest, abdomen, traumatic amputation Comorbid factors fall > 20 ft, ejection from vehicle, high-speed motor vehicle accident |
COMMUNICATION AND EVACUATION
A severely injured soldier on the battlefield needs fully equipped, state-of-the-art medical setup. This utopian requirement may prompt medical planners into ‘forward fixing’ in which surgical teams are moved more and more forward, closer to the battlefield, even though this may severely limit their role to merely that of first-aid providers. Any system placed on the battlefield must be a compromise between what is best for the wounded soldier and what is best for the conduct of the battle. The concept of ‘forward fixing’ is to reduce the time lag between the injury and surgical intervention, and in case of minor injuries, early return to the frontlines. In case of CMI, however, there is no such thing as a minor injury, and each patient has to be evaluated in detail and management planned accordingly. Neurosurgical intervention would presuppose availability of certain equipment and facilities if meaningful neurological recovery is the aim. This would mean access to CT scan, ability to carry out craniotomy and debridement, facilities otherwise taken for granted like suction, bright light and ability to achieve haemostasis by bipolar coagulator, etc. Clearly, if the basic minimum medical facility for neurosurgical intervention cannot be brought to the wounded soldier, the soldier should be brought to it, and his physical condition should be maintained till he arrives. The medical system in battlefield is racing a biological clock, and deterioration of human being after being wounded is predictable and assured. It is for these reasons that emphasis is laid on timely, efficient, rapid evacuation, preferably by air, to a neurosurgical center, where early, definitive surgery can be carried out.
Communication with neurosurgical center is vital and advance warning can minimize the reaction time of the surgical team after the patient reaches the center. In the Armed Forces chain of surgical management, where armed militancy and enemy action has continued over the past several years, the neurosurgical center is informed immediately on telephone by the surgeons working in the advance medical units about the occurrence of casualties, their clinical and neurological status and the likelihood of evacuation. The actual evacuation procedure may be affected by the tactical situation on ground, and whether air evacuation is possible in hostile conditions. In the civilian setup, similar chain of communication can be established starting from Primary Health Centers/ District Hospitals to tertiary referral centers or to neurosurgical centers in private/corporate setup. The police can ensure a “Green Corridor” for rapid surface transport of such patients. The medical resources of an entire city can be divided into zones with active participation of private nursing homes, where first aid can be rendered and correspondingly the salvageablity improved. In the times to come, with explosion of information technology, telemedicine is going to play a major role in the early management of neurotrauma, especially missile injuries. The clinical status and imaging appearances of the patient can be transmitted to the neurosurgeon and advice sought on the line of management or evacuation.
To improve outcome, it is imperative that the interval between injury and therapy be minimized (Kaufman et al 1986, Raimondi et al 1970). Kaufman et al (1986) noted that 52% of their patients were transferred from other hospitals and over 80% of the patients arrived within two hours of injury. Overall, 87% of patients arrived by helicopter. Evacuation of a stable patient is best achieved by helicopter. This was conclusively proved in the Korean conflict and Vietnam war, where often the casualties were evacuated from the scene of action directly to neurosurgical center. Helicopters were used liberally during the Op Vijay in Kargil in 1999, where the evacuation time was reduced to nearly one hour. However, this assumes that air superiority exists and helicopters would be made available. Availability of air evacuation can bypass the intervening echelons and transport the patient directly to the neurosurgical centre. In civilian CMIs, generally the distance involved is not much and patients can expect to reach a neurosurgical center within two to six hours, once a decision has been taken to that effect. Air evacuation for civilians is not yet possible in our country, and most of the patients are transported by road in ambulances.
EXAMINATION OF A PATIENT WITH CMI
CMIs should never be approached in isolation. They often are multiple, leading to multi-organ damage, and ideally, a trauma team should assess the patient. The patient is stripped and a general survey of the patient is done, often along with a general surgery colleague.
Examination of head and neck: External wounds are closely examined. Bone gragments, pulped brain, blood clots and cerebrospinal fluid leakage will be visible in most of the cases. At times, tiny puncture wounds may not be readily visible and these are often unaccompanied by significant intracranial haemorrhage or contusion. In our experience, these patients are often less severely injured since the offending missile is one with low KE. Orbitocranial and faciocranial missile injuries are often accompanied by gross swelling and discoloration due to accompanying skull base injury. There may be CSF orbitorrhoea, rhinorrhoea, and bleeding from the ear; Battle sign may be seen in petrous fractures. Orbitocranial injuries usually have permanent loss of vision due to injury to the globe or to the optic nerve. Trajectory through the sinuses are accompanied by facial swelling and subcutaneous emphysema, even though CSF leak may not be immediately evident.
The mouth and oropharynx are cleared and seen under good illumination with the help of a laryngoscope. Bleeding into the pharynx may be seen in faciocranial injuries and in skull base fractures; these patients often would have swallowed large quantity of blood.
Baseline neurological evaluation: Once the patient is received in a neurosurgical center, a baseline neurological evaluation is carried out. The thoroughness of neurological evaluation is largely dictated the neurological status of the patient. In an unconscious patient, this would mean that any abnormal posturing, and Glasgow Coma Scale (GCS) is noted on arrival, and pupillary reactions, oculocephalic reflex, facial asymmetry, obvious difference in limb movements, muscle tone and tendon reflexes between right and left sides are noted and recorded. If the patient can follow commands, his visual status can be assessed by finger counting, and ocular movements, facial movements can be ascertained. Intact phonation and ability to cough usually gives a fair idea of integrity of lower cranial nerves. Ability of the patient to correctly tell his personal number (a seven or eight digit numerical figure) and to follow commands to move his right/left limbs have been found to be a fairly accurate indicator of intact cortical function indicating less severe injury. While evaluating the severity of injury, GCS is useful for prospective grading, while retrospective grading can be accorded by indicators like duration of coma, post-traumatic amnesia, etc (Simpson 1997). GCS description can further be combined with terms such as akinetic mutism, persistently vegetative state, etc, to give a complete and accurate assessment of the neurological status. In the war zone, casualities more often suffer from polytrauma as compared with civilian injuries and closed head injuries; war head injury score (WHIS) that incorporates both – GCS and injury severity score (ISS) is an accurate predictor of outcome in the presence of multisystem trauma and CMI (Turina et al 2001).
ACTION AT PERIPHERAL MEDICAL SETUP
Depending upon the resources and expertise available, the aim at a peripheral medical setup should be to evacuate the patient to the nearest in the shortest possible time with stable vital parameters. Attention is paid to airway, respiration and circulation (‘The ABC of Resuscitation’: Table 1). After ensuring an adequate airway by oropharyngeal suctioning, insertion of airway, intubation, etc., ventilation must be commenced in apnoeic patients. When Ventilatory support is required, oral intubation should be performed. A short acting non-depolarising neuromuscular blocking agent (vencuronium 0.01 mg/kg every 15-30 minutes) and sedative agent (thiopental 4 mg/kg or midazolam 0.07 mg/kg) may be administered in semi-conscious patients to minimize rises in intracranial pressure. Pulse oximeters are becoming standard equipment on ambulances and can be used to optimize patient’s ventilatory status. Intravenous drips that will not get dislodged during transit are inserted and all external haemostasis is achieved. Fractures of long bones are splinted and open chest wounds are closed. Whether to subject the patient to CT at the nearest scanner at this stage will depend on the patient’s clinical condition. Severe head injuries are now routinely investigated by early CT, which visualizes most of the pathological lesions of immediate surgical importance. The initial clinical examination is still crucially important in triage and as a baseline in assessing progress. The prognosis depends on the findings of the initial examination and neurological status at a specified time after injury is widely used as a measure of severity of head injury. However, modern strategies of severe head injury management have brought one very important change in the protocol of clinical examination: because endotracheal intubation may have to be done as soon as possible, first neurological evaluation may never have been carried out. Hence the paramedic should be aware of the need for recording the preliminary neurological findings for future reference. Moreover, valuable as they are, the neuroradiological findings must be interpreted in the light of clinical findings. Broad spectrum antibiotic which crosses into the CSF is administered and the head wound is covered with povidone-iodine soaked gauze since infection is a major threat in these patients while they are being evacuated to neurosurgical center for definitive management. A decision is taken according to the priority of the case whether to evacuate the patient by ambulance or by air.
Table 3: Primary survey in cases of CMI
| Function assessed | Observation | Clinical parameters |
| A. Airway B. Breathing C. Circulation D. Disablity E. Expose | patent? noisy? effective? adequate? normal? other inquiries? | rate & depth, chest movements, air entry, Cyanosis? pulse rate & volume, blood pressure, skin colour, cold clammy limbs? capillary return, ext/internal haemorrhage conscious level/GCS, Pupils, limb movements limbs, neck, chest, abdomen, pelvis, back |
Preliminary medical management: Intravenous line is setup and antibiotics are administered in antimeningitic dosages soon after arrival in a medical unit, usually in the ADS in the military chain of evacuation. During the Vietnam conflict, penicillin and chloramphenicol were the most commonly used antibiotics for CMI (Hagan 1971). In the recent times, third generation cephalosporins, in conjunction with an aminoglycoside, nafcillin or vancomycin in antimeningitic dosages, have been efficacious in preventing delayed meningitis and brain abscess. Antibiotics are usually continued for 10-14 days after the injury (Aarabi 1989). We have routinely used cephalosporins and an aminoglycoside for antimicrobial prophylaxis in CMI. Since epilepsy risk is high in patients with CMI, intravenous phenytoin is administered routinely to all such patients (Weiss et al 1986). Intravenous levetiracetam is another option to prevent seizures. Intravenous mannitol and loop diuretic (frusemide) are administered once the patient is haemodynamically stable.
Illustrative case: A 45-year-old army soldier sustained multiple splinter injuries to his face, neck and chest wasll in an IED explosion. He was airlifted to neurosurgical center within six hours of injury. On arrival, his GCS was 8/15 with dilatation of right pupil, and right orbital puncture wounds. He was tachypniec with SPO2 of 75%. There was no intrathoracic injury. He was put on ventilator for 72 hours and then gradually weaned off. GCS was 15/15 after weaning off, and he was seen to have right sided ocular injury. CT brain could be done on the fourth post-injury day, which showed three pellets embedded in the right frontal lobe, and one lying in the posterior third ventricular region. He was managed conservatively, and was asymptomatic when reviewed one year later. Vision in right eye was restored by intraocular lens implantation. The intracranial splinters had not moved from their initial location.
CONCLUSION
CMI management requires an integrated team approach. During war and antimilitancy operations, neurotrauma cannot be viewed in isolation since each patient potentially suffers from polytrauma. The evacuation from the scene of action to neurological center has to be quick, efficient taking all due care to maintain airway, oxygenation and circulation. Many lives can be gainfully saved if we can evolve a system of triage, timely evacuation of these patients directly to a neurosurgical center, where detailed evaluation can be carried out and management plan chalked out by a dedicated trauma team. Baseline neurological evaluation gives vital information for prognosis and for further comparison.
REFERENCES
- Aarabi B. Causes of infections in penetrating head wounds in the Iran-Iraq War.
Neurosurgery 25:1056-1063, 1989. - Chales Leale. https://en.wikipedia.org/wiki/Charles_Leale. Accessed 16 Jan 2018.
- Garner A, Lee A, Harrison K, et al. Comparative analysis of multiple-casualty incident triage algorithms.
Ann Emerg Med 38:541-548, 2001. - Hagan RE. Early complications following penetrating wounds of the brain.
J Neurosurg 34:127-131, 1971. - Hughes JH. Community medicine. Triage-a new look at an old French concept.
Postgrad Med 60:223-227, 1976. - Kaufman HH, Makela ME, Lee KF, et al. Gunshot wounds to the head. A perspective.
Neurosurgery 18:689-695, 1986. - Raimondi AJ, Samuelson GH. Craniocerebral gunshot wounds in civilian practice.
J Neurosurg 32:647-653, 1970. - Ramesh T, Prasanna GV, Bhat AR, Mohanty S. Low velocity craniocerebral missile injuries in civilian practice: A 16-year-experience.
Neurosciences Today 2:103-107, 2001. - Rish BL, Dillon JD, Weiss GH. Mortality following penetrating craniocerebral injuries, an analysis of the deaths in the Vietnam Head Injury Registry population.
J Neurosurg 59:775-780, 1983. - Simpson DA. Clinical examination and grading. In, Reilly P & Bullock R (eds). Head Injury. Chapman & Hall Medical, London; 1997: 145-164.
- Turina D, Sustic A, Ticac Z, et al. War Head Injury Score – an outcome prediction model in war casualties with acute penetrating head injury.
Mil Med 166:331-334, 2001. - Weiss GH, Salazan AM, Vance SC et al. Predicting post-traumatic epilepsy in penetrating head injury.
Arch Neurol 43:771-773, 1986. - Wisemen DB, Ellenbogen R, Shaffrey CI. Triage for the neurosurgeon.
Neurosurgical Focus 12(3): Article 5, 2002
Date: 02/01/2018











