
Almanac
Singapore, Republic of


Surgeon General
BG (DR) Lee Wei Ting
701 Transit Road #06-01
SINGAPORE 778910
Pictures and Graphics: Wikimedia Commons
Brief introduction to the Singapore Armed Forces
The Singapore Armed Forces (SAF) is responsible for protecting the territorial integrity and defending the security interests and sovereignty of the Republic of Singapore. The SAF has a total of four service branches: the Army, the Air Force, the Navy, and the Digital and Intelligence Service. Amongst her neighbours in Southeast Asia, Singapore stands out for the “technological sophistication of its armed forces and for its model of military mobilisation”.1
Overview of the Singapore Armed Forces Medical Corps
The SAF Medical Corps is the Joint military medical service of the SAF. The SAF HQ Medical Corps establishes and directs the policy functions covering medical human resource and professional matters; medical operations (covering both current and anticipatory operations) and safety; medical logistics procurement, warehousing and distribution; medical capability development; force health policy and standards; medical bioinformatics; medical biodefence policies; and medical inspectorate and audits.
The execution of these medical policies, directives, and regulations are carried out by (1) the various Medical Services of each Service Branch of the SAF (i.e. Army Medical Service, Air Force Medical Service, Navy Medical Service, and Digital and Intelligence Service Medical Branch), (2) MMI that oversees the governance and operations of the SAF Medical and Dental Centres across Army and Joint bases, (3) the SAF Medical Training Institute which undertakes all of the basic and advanced professional and leadership training of medical vocationalists, and (4) Medical Classification Centre which undertakes the medical screening of every pre-enlistee in the SAF and assigns them a medical grading classification, which will in turn inform their assignment to specific vocations across the SAF.
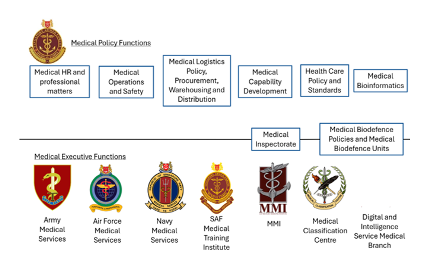
Figure: Overview of the Medical Policy and Executive Functions in the SAF Medical Corps
Source: Ministry of Defence Singapore
The mission of the Singapore Armed Forces (SAF) Medical Corps is to provide excellent and comprehensive health care for our soldiers, protect their health, and optimise their combat performance in order to enhance the SAF’s operational edge. Our vision is to be a world-class Medical Corps that is a leader in Military Medicine.
Three broad strategies underpin the SAF Medical Corps’ approach to achieving our organisational mission and vision:
(1) Seek - Seek to build partnerships with Whole of Government and strategic partners in this dynamic and resource tight environment;
(2) Save - Save lives through ensuring high operational readiness and effectiveness; and
(3) Serve - Serve the nation and the SAF through the provision of timely and quality health care, and giving our service personnel a pleasant medical experience that is at least on par with the standards of national public healthcare institutions.
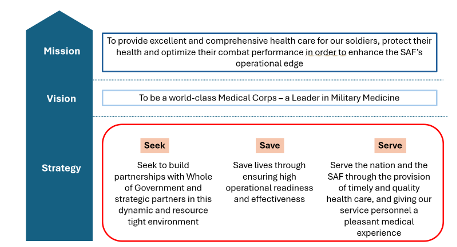
Figure: The SAF Medical Corps’ Mission, Vision, and Strategy
Source: Ministry of Defence Singapore
Overview of the SAF Medical Corps’ Ecosystem
The SAF Medical Corps exists within the nation’s wider healthcare ecosystem. In a way, this embodies the spirit of Singapore’s ‘Whole of Government approach’ to finding an integrated and streamlined process to solving complex issues. For instance, the SAF does not operate its own military hospital and instead relies on the excellent healthcare infrastructure and care provided by the nation’s public healthcare institutions. As such, in peacetime, service personnel who need secondary and/or tertiary-levels of care are referred to one of these public healthcare institutions.
An example of this is the SAF’s Cardiac Fitness Centre (SCFC), which is physically located and operated by the Singapore General Hospital’s National Heart Centre Singapore.2 The SCFC provides dedicated, expedited specialised cardiac service for the SAF. By significantly shortening the waiting time for a cardiac appointment at a public healthcare institution, the creation of SCFC has served to reduce enlistment wait times for pre-enlistees and minimise training and deployment downtimes for enlisted personnel. A second example of this ‘Whole of Government approach’ is played out in ensuring medical supply chain resiliency (in peace and operations) as the SAF Medical Corps partners with the Ministry of Health and her key supply chain partners to procure and stockpile common pharmaceutical and medical supplies. This will allow economies of scale and ensure supply chain resiliency by tapping on larger ecosystems for common items. A third and final example is the education and training of the SAF’s medical vocationalists to pursue specialist training, professional accreditation, and upgrading courses in partnership with local tertiary educational institutions.
On top of this, the SAF Medical Corps has a holistic quality management ecosystem that entails audits of our healthcare system, medical logistic system, medical IT systems, and safety system. Our quality management system looks at our people, our processes, and our system. All medical, dental, and nursing professionals, and paramedics in the SAF Medical Corps adhere to the national licensing requirements and professional practice standards. There is also a clear system of qualification and accreditation for our front-line healthcare providers (paramedics and medics). For example, all medics undergo an annual proficiency test to assess their individual competency in basic resuscitation skills. Each medical centre undergoes an evaluation of the entire medical team to assess each team’s preparedness and ability to work as a team to manage medical emergencies.
The SAF’s Peacetime Healthcare Services
The SAF provides in-house primary care and a selection of specialist services of relevance to the military. This includes aviation medicine, hyperbaric medicine, orthopaedics, psychiatry and sports medicine, among others. Peacetime healthcare services are primarily governed and provided by MMI for all SAF personnel. The specialist military medical domains are anchored by their respective Medical Service. For instance, Sports Medicine is anchored by the Army Medical Service, Aviation Medicine is anchored by the Air Force Medical Service, and Hyperbaric Medicine is anchored by the Navy Medical Service. The SAF’s force health is professionally governed and is aligned with national clinical standards and best practices.2
Peacetime healthcare services are provided through a network of Medical and Dental Centres covering all SAF facilities. These centres provide primary and emergency care as a baseline. Regional Health Hubs are also being developed, which offer advanced diagnostic capabilities and specialist services tailored to the military population being served.
In terms of clinical governance, the SAF has a three-tier civilian medical advisory framework comprising nationally renowned experts in their respective fields of medicine. The framework is made up of the (1) SAF Medical Advisory Board, (2) SAF Specialist Advisory Boards, and (3) SAF Visiting Consultants. The SAF Medical Advisory Board advises MINDEF/SAF on key medical policies, provides advice on the development of health services in the SAF, and facilitate cooperation with the national public health institutions. The SAF Specialist Advisory Boards are specialty specific and advises the SAF on medical policies and clinical best practices in Cardiology, Emergency Medicine, Respiratory Medicine, Psychiatry, and Infectious Diseases. The SAF Visiting Consultants comprise medical and dental specialists from a wide range of sub-specialties that may not be available in the SAF, and they provide expert opinion on the management of complicated clinical cases.
Since 1995, the SAF has relied on electronic healthcare records. The SAF’s electronic medical records system is called the Patient Care Enhancement System or PACES for short, which allows central archiving and access to the health information of all SAF service personnel irrespective of the medical facility at which they have visited. PACES (currently in its third iteration, and works are underway to develop the next iteration) is connected to Singapore’s National Electronic Health Record (NEHR) system that allows SAF healthcare professionals to view patients’ records across the national healthcare network. This ensures seamless and efficient information transfer for servicemen as they transit between the SAF and public healthcare system.
The SAF’s Mental Health Ecosystem
As a conscript army, it is recognised that national servicemen in the SAF would experience a period of psychological and emotional adjustment as they transition from civilian to military lifestyle. Common issues they might face include, but are not limited to, homesickness, coping with regimentation, managing relationships with superiors and peers, difficulties in coping with physical training demands, and adjusting to communal living. These could, either singly or in combination, precipitate the onset of mental health conditions. To mitigate and prevent poor mental health outcomes during National Service (NS), all pre-enlistees are screened for pre-existing mental health conditions at the Medical Classification Centre (MCC) so they can receive professional help and treatment during their National Service.
The Mental Health Office (MHO) was established in December 2022 bringing together the Psychological Health Group (PHG) from Defence Psychology Department (DPD), SAF Counselling Centre, and MMI’s Psychological Care Centre (PCC) under the operational control of the Chief of Medical Corps (CMC), as Director MHO to improve coordination of mental healthcare services across the Ministry of Defence (MINDEF) and the SAF. With its mission to provide mental health services to service personnel to enable them to be deployed optimally towards operational effectiveness; MHO seeks to enhance the SAF mental health ecosystem by ensuring holistic delivery of psychiatric, psychological, and counselling care services to service personnel through a multi-pronged approach guided by the MINDEF/SAF Mental Health Framework.
The four strategies in the MINDEF/SAF Mental Health Framework are Prevention, Detection, Support, and Evaluation and Research. These four strategies represent a shift from a reactive and resource-intensive approach to care and treatment to one that is more upstream and proactive. Such strategies have been shown to be efficacious in preventing poor well-being and result in better treatment outcomes due to early intervention. The Prevention strategy seeks to enhance mental health literacy, protective factors and modify risk exposure to reduce the incidence of mental disorders and poor well-being. The Detection strategy seeks to establish an ecosystem of checks to enable accurate and early identification of service personnel with mental health concerns, to provide appropriate care and avert mental health crises. The Support strategy focuses on a layered approach to care. At the baseline, psychological first aid is taught to service personnel to facilitate responsive support and referral to professional mental health care. The Evaluation and Research strategy focuses on ensuring high standards and a data-driven approach to mental health care.
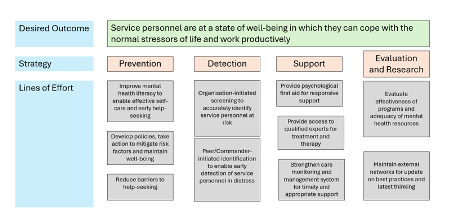
Figure: MINDEF/SAF Mental Health Framework
Source: Ministry of Defence Singapore
The SAF’s Health Promotion Efforts
The Singapore Armed Forces (SAF) recognizes the critical importance of health promotion among its service personnel, given the significant impact on both individual well-being and national health outcomes. Each year, all eligible young Singaporean males are enlisted into National Service, providing a valuable opportunity to instil lifelong healthy habits that can mitigate chronic disease burdens.
To this end, the MINDEF Healthy Lifestyle Steering Committee (MHLSC), established in 1991, oversees workplace health promotion policies and initiatives within MINDEF/SAF
The MHLSC aims to foster a culture of health through targeted programs and activities that promote physical fitness, mental wellness, and healthy lifestyle choices. Key components of SAF’s health promotion efforts include:
(1) Physical Fitness Programs - Regular fitness training and assessments ensure that all SAF personnel maintain optimal physical health. Programs such as the Individual Physical Proficiency Test (IPPT) and regular physical training sessions are integral parts of the SAF.
(2) Nutritional Guidance - Balanced and nutritious meals are provided at SAF dining facilities, with continuous efforts to enhance the nutritional quality of food. Educational campaigns on healthy eating habits complement these initiatives.
(3) Mental Health Support - The SAF prioritizes mental wellness through comprehensive support systems, including counselling services, psychological resilience training, and stress management workshops. The Mental Health Office (MHO), established in 2022, coordinates these efforts to ensure holistic mental health care.
(4) Preventive Health Screenings - Regular health screenings and medical check-ups are conducted to detect and address health issues early. These screenings cover a wide range of conditions, from cardiovascular health to mental health assessments.
(5) Health Education Campaigns - Continuous health education initiatives aim to increase awareness and knowledge about various health topics. Workshops, seminars, and informational materials are used to educate service personnel on the benefits of a healthy lifestyle.
(6) Innovative Health Solutions - Leveraging technology, the SAF has implemented telehealth services and digital health platforms to provide accessible healthcare support. The integration of wearable health devices allows for real-time monitoring and personalized health interventions.
By fostering a comprehensive health promotion ecosystem, the SAF strives to enhance the overall health and readiness of its personnel, thereby contributing to the operational effectiveness and resilience of the armed forces.
The SAF’s Service Specific Medical Services
Army
The Army Medical Service (AMS) is one of the formations of the Singapore Army and provides medical support to the Army throughout the entire continuum of operations from peacetime to war.
The Medical Response Force (MRF) is an elite medical force under AMS that is trained to provide medical support to casualties following chemical, biological, radiological and nuclear incidents. An MRF response team is capable of not only providing a level of medical care equivalent to an Army Battalion Casualty Station, but also CBRN-specific decontamination and treatment capabilities. Equipped with the modern Medical Decontamination and Treatment Vehicle (MDTV), the MRF is able to respond swiftly to such incidents and bring advanced medical care to the front-line to enhance the survivability of casualties.3 Although MRF’s main role is to support SAF, the MRF is also operationally ready to respond to national level CBRN incidents as part of the wider ‘Whole of Government’ response (led by the Singapore Civil Defence Force, SCDF) when activated. Notably, MRF has been tasked to provide CBRN medical support for major national events such as the annual National Day Parade.
In the area of battlefield medical support, the AMS seeks to provide a trauma management system on the battlefield. In its ongoing transformation, AMS aims to provide advanced trauma life support within the “golden hour” and timely damage control surgery and primary or definitive surgery. Key developments in the transformation journey include the equipping of front-line combat medics, paramedics and Medical Officers with a suite of resuscitation and life support equipment at the Battalion Casualty Stations; and deploying Mobile Surgical Teams to provide forward, life-saving surgery where it is most needed.4
The Army’s Combat Surgical Hospitals comprise the pinnacle of the SAF’s battlefield medical facilities where damage control or definitive surgery can be provided. Each CSH comes with operating theatres, a high-dependency care unit, a radiology unit and field laboratory, fully transportable by land, air, or sea to give greater flexibility for deployment options. On land, the hospitals are deployed in integrated and rapid-deployable platforms, comprising customised, expandable containers and inflatable tent systems.
To meet the challenges of casualty evacuation, the AMS maintains a fleet of wheeled and tracked ambulances, augmented by rotary air assets of the Republic of Singapore Air Force.
Air Force
The Air Force Medical Service (AFMS) supports the Republic of Singapore Air Force’s (RSAF) effectiveness across its full spectrum of missions through comprehensive medical and psychological support, including specialist aeromedical expertise and human performance maximisation.
HQ AFMS formulates operational medical doctrine and oversees the planning and execution of medical support for the RSAF’s operations. These range from primary healthcare and preventive medicine for all RSAF personnel, to operational medical support for RSAF ground and flying operations and exercises (both local and overseas). HQ AFMS also oversees strategic Aeromedical Evacuation (AME) for the SAF - from operational doctrine development and training in AME for its medical personnel, to the planning and execution of fixed-wing AME operations. For rotary-wing medical evacuation, 1 Medical Squadron (under the RSAF’s Participation Command) supports the nation’s 24/7 Search and Rescue (SAR) standby operations in support of the Singapore Flight Information Region (FIR) and oversees the operational readiness of heli-medevac operations through continuous doctrine development, capability development, and training.
The RSAF Aeromedical Centre (ARMC) is AFMS’s aeromedical specialist centre for the RSAF, and is a regional Centre of Excellence in aviation medicine. Inaugurated in 1982, it is a one-stop aeromedical specialist centre for clinical and operational aviation medicine and aviation physiology training5 for the RSAF, with branches overseeing (i) clinical aviation medicine; (ii) aviation psychology; (iii) aviation physiology training and crew safety; and (iv) performance maximisation. The consolidation of aeromedical expertise at ARMC has provided the platform for the progressive refinement of medical and psychological screening and selection for the RSAF, performance maximisation research and trials, and the conduct of aeromedical evacuation.5
The RSAF’s aviation physiology training (APT) programme supports flight safety by providing didactic and experiential learning to aircrew on the limits of human physiology, and the potential degradation of physical and mental performance during flight or exposure to altitude. It is conducted with a comprehensive suite of physiology training equipment - namely the Human Training Centrifuge (HTC), Spatial Disorientation Trainer (SDT), Hypobaric Chamber, Air Force Night Vision Integrated Laboratory (ANVIL), and Ejection Seat Trainer (EST). The RSAF APT programme has been accredited by the US Air Force (USAF) since 1998, and the RSAF ARMC continues to maintain the operational relevance of APT by onboarding and inducting new capabilities to enhance the training experience of aircrew. This includes the incorporation of dynamic flight simulation for HTC training, and using a Virtual Terrain Image Generation System for night vision training.
The RSAF ARMC is nationally-accredited and the biggest training centre for aviation medicine in Singapore. It has been responsible for the training and qualification of successive generations of aviation medicine specialists and aviation psychologists in Singapore.
Navy
The mission of the HQ Navy Medical Service (NMS) and Medical Flotilla (MEDFLOT) is to provide excellent medical support and comprehensive healthcare for the Republic of Singapore Navy’s (RSN) sailors, in order to contribute to mission success.Today, the Republic of Singapore Navy’s (RSN’s) medical support is provided by two entities. HQ NMS provides medical policy guidance and Specialist Staff Officer (SSO) support to the RSN. Following NMS redesign efforts, the Medical Flotilla (MEDFLOT) was inaugurated in Aug 2023, MEDFLOT has assumed the planning and execution of operational medical support for the RSN’s units.
Together HQ NMS & MEDFLOT (1) provide comprehensive medical support for RSN’s full spectrum operations; (2) ensure and optimise the health of the Navy and (3) positions the RSN as a regional leader in underwater medicine.
MEDFLOT is responsible for the provision of ashore and afloat medical support to the Naval Diving Unit (NDU), Fleet and Maritime Security Task Force, and the Maritime Security Command (MARSEC). Ashore, a range of primary healthcare and emergency healthcare services are provided at three Navy medical centres to navy personnel. Equipped with the latest RSN Operational Deployed Medical Equipment (RODME) stores, the Shipboard Medical Team, working together with the ship’s First Aid Party, is able to provide both primary healthcare and advanced trauma life support to the crew during missions and deployments.
Surgical capabilities afloat have been deployed on RSN vessels to support overseas deployments, and humanitarian aid and disaster relief missions. One of the RSN’s rapidly deployable and scalable surgical capabilities is the Rapidly Deployable Maritime Container (RDMC) system, which was operationalised in 2016. The RDMCs provide a modular and scalable maritime surgical capability for the RSN. Key features of the RDMC include: (1) Operational flexibility that allows deployment on land or at sea; (2) Corrosion resistance for enhanced survivability at sea; (3) Adaptability through a universal coupling system that allows the RDMC to tap on the vessel’s electrical, water and sewage systems for continuous operations, and (4) Hospital grade High-Efficiency Particulate Air (HEPA) filter and laminar air flow system, which reduce the risk of infection, enhance patient safety and maximise survivability of casualties.6
Shipboard Surgical Teams also perform damage control surgeries in confined spaces on the frigates and landing ship tanks (LST). For instance, through ingenious design the medical centre on board the Formidable-class frigates can be dual-roled into an Operating Theatre (OT), and the dining room can be rapidly converted into an Intensive Care Unit (ICU). These innovative solutions increase operational flexibility, and expand the frigate’s mission profiles.
The RSN maintains a niche expertise in Underwater Medicine. MEDFLOT operates two multi-place hyperbaric chambers with Transfer Under Pressure (TUP) and Intensive Care Capabilities at the Naval Hyperbaric Centre to provide recompression treatment. From 1984 to 1987, when the first Mass Rapid Transit (MRT) underground tunnels were dug, NMS’ provided essential compressed air works consultancy and on-site recompression treatment using a COMEX hyperbaric chamber during Singapore’s MRT tunnelling project. In 2009, NMS together with the Singapore General Hospital (SGH) established the SGH Hyperbaric and Diving Medicine Centre, to provide a one-stop diving and hyperbaric medical facility with access to tertiary level medical care and specialist services. The SGH Hyperbaric and Diving Medicine Centre treats military and civilian divers, provides education and training for medical personnel and conducts underwater medicine research.6
Distressed Submarine (DISSUB) scenarios due to underwater incidents or technical failure will require collective rescue or individual escape of its crew. The RSN maintains a submarine rescue suite on MV Swift Rescue. The rescue suite includes a submersible (DSAR6) which is capable of mating with a DISSUB and rescuing up to seventeen crew at once; a remotely operated vehicle capable of underwater search and delivery of life-support supplies to a DISSUB; recompression chambers on MV Swift Rescue which allowed Transfer-Under Pressure (TUP) from DSAR6; an eight-bed high dependency and ten-bed general ward; and a patient elevator and helipad to facilitate helicopter-evacuation. RSN’s submarine rescue suite has since drawn accolades from the international submarine rescue community, resulting in several submarine rescue agreements with regional navies. RSN has positioned herself as the submarine rescue hub in the region. Since then, MV Swift Rescue has been deployed in support of regional Search and Rescue efforts for distressed submarines, and downed aircraft.7
Digital and Intelligence Service
The SAF’s fourth service, the Digital and Intelligence Service (DIS), was inaugurated in October 2022 to provide accurate, relevant and timely intelligence for early warning, decision making, and to support the full spectrum of SAF’s operations. The DIS plays a critical role in defending Singapore from threats in the digital domain, and allows the SAF to operate better as a networked and integrated force to deal with a wider spectrum of external threats to enhance and safeguard Singapore's peace and sovereignty.
The DIS Medical Branch (DMB), newly established within DIS HQ, is tasked with providing medical expertise for policy development and designing operational medical doctrine for this nascent service. The DMB plays a crucial role in maintaining the cognitive health and mental well-being of personnel who operate in high-stress, technologically advanced environments and sustained surge operations.
DMB’s core strategy is to integrate health as a fundamental tenet of the DIS Guardian’s journey. A robust Occupational Health Programme aims to minimise attrition by managing workplace hygiene and enhancing performance through optimised ergonomics. By leveraging design thinking, active health promotion, and tailored lifestyle programs, physical health will be maintained not only as a protective measure but also as a foundational base to support and enhance cognitive health.
Protecting the mental well-being of service personnel in the digital and intelligence domains is paramount for the DIS. In collaboration with DIS psychologists, a comprehensive mental health framework will be developed to build mental resilience at both individual and team levels, with an additional focus on maximising cognitive performance.
Force Health Protection Against CBRN Threats
The SAF Medical Corps is committed to medical protection against chemical, biological, radiological and occupational health hazards. The three key thrusts for the SAF’s biodefence philosophy, against chemical, biological, radiological, and nuclear (CBRN) threats, are Early Warning, Protection, Detection and Diagnosis, Containment, and Recovery.4 The Singapore Armed Forces (SAF) has reorganized its force health protection capabilities into the Force Health Group (FHG) to enhance its response to these threats. The FHG is dedicated to ensuring the highest standards of health protection and readiness across the SAF. The SAF’s key biodefence accomplishments, in the realm of biological threats, include eliminating Malaria risk from Pulau Tekong (an offshore island designated for military training) in 2007, formulating the SAF pandemic response plan during the 2009 H1N1 outbreak in Singapore, managing the Zika virus outbreak in August 2016, and more recently managing the SAF’s responses to the COVID-19 pandemic.
Key elements of the Force Health Group's mandate include:
(1) Early Warning and Surveillance - The FHG employs advanced biosurveillance systems to detect and monitor potential CBRN threats. This proactive approach allows for early identification and timely intervention, minimizing the impact on SAF personnel.
(2) Detection and Diagnosis - The FHG collaborates with strategic partners such as Clinical Diagnostic Services Laboratory, Defence Science Organisation (DSO) National Laboratories, in utilizing state-of-the-art detection technologies and diagnostic tools to identify CBRN agents accurately. This capability ensures rapid response and effective containment of any CBRN incidents.
(3) Collaboration and Research - The FHG collaborates with local and international health authorities, research institutions like the National University of Singapore’s Saw Swee Hock School of Public Health, and strategic partners to stay at the forefront of CBRN defence. Continuous research and development efforts are undertaken to enhance biosurveillance, diagnostic capabilities, and medical treatments.
(4) Integrated Public Health Policies – The FHG is responsible for the development and implementation of public health and force health protection policies for the SAF. Working closely with the Ministry of Health and other national agencies, the FHG ensures that SAF’s public health policies align with national standards. This integrated approach enhances overall force health protection and resilience.
The SAF Medical Training Institute
The SAF Medical Training Institute (SMTI) is the centre of excellence for Military Medicine training in the SAF. Its mission is to provide high quality and comprehensive training in military medicine. The high standard training enhances the SAF’s operational edge in both Peace and in times of War.8
SMTI conducts a diverse range of training, ranging from pre-hospital emergency care, primary healthcare to tactical combat casualty care and trauma injuries management, to both Active and NS servicemen in the SAF. Since the 1990’s, SMTI has conducted the Emergency Medical Technician (EMT) course, which is accredited by the Justice Institute of British Columbia (JIBC) and SkillsFuture Singapore (SSG), to train Medics to be deployed in operational units and the medical centres. In addition to developing individual competencies, SMTI also trains servicemen at the team and unit levels such as the BCS Platoon, Medical Companies, and Combat Support Hospitals to ensure that the medical teams are proficient in their operational deployment.
In 2015, the National Paramedic Training and Education roadmap was launched by the SAF and Singapore Civil Defence Force (SCDF) to establish a long-term professional programme to strengthen the competencies of paramedics in Singapore, and chart the many pathways that paramedics can take to pursue professional upgrading. This multi-agency effort provides multiple pathways for paramedics to deepen their expertise and better equip them with the medical knowledge and practical skills to support the SAF’s wide range of operations. For instance, selected EMTs undergo job rotations with the SCDF’s Emergency Ambulance Services and the Emergency Departments of various public sector hospitals respectively.
While the Emergency Medical Technicians (EMT) form the main bulk of SMTI’s trainees pool, the Medical Officers, Dental Officers, and Nurses also go through leadership and vocational training to be competent in their various roles. SMTI is also a recognised training centre to conduct ATLS training for both military and civilian doctors. In addition, SMTI conducts medical skills training for all servicemen in the SAF, such as CPR and AED training, which are accredited by the Singapore Resuscitation and First Aid Council (SRFAC).
In May 2022, SMTI was recognised as an Authorised NAEMT Training Centre for Tactical Combat Casualty Care (TCCC). This enables SMTI to benchmark itself to international standards in TCCC. The additional skill also equips our medical vocationalist with capabilities that raise the standards of pre-hospital emergency care in austere environments to support military operations.
SMTI remains committed to sustaining its high standards and continuously raising the bar in training. This commitment is reflected in its proactive approach to seeking new opportunities for improvement and innovation. In alignment to the Army’s pivot to Transform Training, SMTI had adopted a “Teach Better, Learn Better and Perform Better” approach to elevate training outcomes and performance. As part of the “Teach Better” initiatives, SMTI actively utilises web-based and mobile applications to enrich the learning journey of the trainees. The development of educational bots, hosting content such as combat casualty aid, CPR and AED protocols, enables trainees to have ready access to content that is presented in an interactive method that aids retention and application. Another example is the use of a web-based software ‘Twine’ to craft case scenarios based on established medical treatment protocols for medics and allow trainees to select their course of action based on the presented information. This web-based app is accessible through trainees’ personal electronic devices and allows them to learn at their own convenience and hone their decision-making skills when faced with a casualty.
To “Learn Better'', SMTI constantly reviews its training methodologies and employs the latest pedagogies and learning science to ensure relevancy and raise overall training effectiveness and standards. SMTI has modernised its training approach, taking into consideration the profile of the newer generation of learners and advancement in technology. This represents a paradigm shift where the new curriculum will be increasingly learner-centric with the focus on addressing the learner’s needs. This entails more self-directed learning and the creation of a flexible learning environment where there are no barriers to where and how one can learn through the incorporation of technology. For instance, SMTI equipped every learner with a laptop/tablet to access the Next-Gen Learning System (NGLS) courseware from an integrated learning portal. The modules are curated to enhance learning and assessment at the individual levels, at the trainees learning pace. Upkeeping with times, the adaptation of Artificial Intelligence and Machine Learning (AIML) tools in Medic training such as the Digital Intravenous Application (DIVA), allows for a learner – centric training environment which enhances the psychomotor skills of the medic trainees. The tool offers trainees a flexible and safe platform for self-practice with live feedback to correct incorrect postures, cultivating good clinical skill sets.
SMTI is dedicated to advancing medical training through the integration of cutting-edge technology and simulation learning methodologies to “Perform Better”. The introduction of the Next-Gen Medical Simulation System (NGMS) framework is designed to immerse medical personnel in diverse and challenging scenarios, refining their clinical acumen, fostering complex decision-making skills and enhancing their ability to manage uncertainty effectively. SMTI leverages on the state-of-the-art tools such as cut suits and various Augmented Reality (AR) technologies as these innovative resources enable SMTI to provide her trainees with realistic simulation experiences, compensating for diminishing opportunities for real-world training. By embracing these advancements, SMTI ensures that the medical professionals are equipped with the skills and confidence needed to excel in dynamic and unpredictable healthcare scenarios. SMTI’s Medical Simulation and Training Centre (MSTC), which was established in 2012, was able to meet the early SAF‘s medical simulation training demands. As part of the NGMS effort, MSTC together with the other training facilities in SMTI will undergo an overhaul to eventually incorporate Next-Gen Medical Trainer Simulator Systems (with VR/AR capabilities), together with Data Analytics and management tools to provide high fidelity, immersive training with performance analysis in a fail-safe environment.
The SAF Medical Corps’ Operations Other Than War
Despite its relatively small size, the SAF Medical Corps has actively contributed to national civil emergencies (such as the collapse of Hotel New World in 1986), overseas humanitarian assistance and disaster relief (HADR) efforts, and over twenty overseas Peace Support Operations. As Singapore has limited resources and manpower, Singapore's approach is to focus our contributions in niche areas, where the SAF has expertise and which our international partners find operationally useful.
Her first overseas HADR mission comprised a medical team deployment to East Pakistan (now known as Bangladesh) in 1970, in the aftermath of a devastating cyclone that swept the country. Since then, the SAF Medical Corps has contributed medical relief following earthquakes, floods, and other natural disasters in the region. It mounted its largest HADR operation following the Indian Ocean tsunami of 2004, where more than 1,200 SAF personnel, together with medical and surgical teams deployed to Aceh in Indonesia. As part of the Whole of Government approach, the SAF Medical Corps’ latest HADR mission was the deployment of a combined medical team (including doctors and nurses from public health institutions) to Gokarna, Nepal, in late Apr 2015 in the aftermath of an earthquake.
Likewise, as part of the Whole of Government/SAF’s HADR efforts, forensic teams have been deployed to identify disaster victims. Till date, the SAF has deployed her forensic odontologists to five Disaster Victim Identification (DVI) efforts in the region: (i) 1997 Silk Air Flight MI185 crash in Palembang, Indonesia;9 (ii) 2004 Boxing Day Tsunami in Phuket, Thailand; (iii) 2011 Christchurch Earthquake, New Zealand; (iv) 2015 AirAsia QZ8501 crash in Surabaya, Indonesia; and (v) the 2015 Nepal Earthquake.10
Since 1991, the Medical Corps has deployed numerous teams to support United Nations and Multi-National Peace Support Operations (PSO). To date, the SAF Medical Corps has been deployed to Cambodia, Guatemala, Timor Leste, Indonesia, Iraq, Afghanistan and the Democratic Republic of Congo. Our officers have also served in the medical section of the United Nations Department of Peacekeeping Operations (DPKO).
For example, under the Ops Blue Ridge (OBR) series of deployments (starting from 2007 to 2013), the SAF Medical Corps established a dental clinic at the provincial hospital in Bamiyan, Afghanistan, in 2007.11 In addition to providing much needed dental care to over 500 patients, the SAF dental team also conducted training courses to train the local dental assistants and the sole local dentist as part of a skills transfer and sustainable development project jointly undertaken with the local Afghan health authorities. Subsequently, the SAF Medical Corps deployed another five medical teams and one surgical team in a multi-national Role 2 hospital to Tarin Kowt, in Afghanistan, to provide primary healthcare and surgical support.
The SAF’s Defence Relationships with Foreign Military Medical Services
Even before the COVID-19 pandemic, health had become an important area for international engagement. In the military healthcare context, military medical diplomacy efforts can prove to be an effective and ethical platform for bi-lateral and multi-lateral engagement between foreign military medical services.12
In 2010, military medicine was identified as one of the five areas for collaborations amongst ASEAN and the Plus nations with the establishment of the ASEAN Defence Ministers’ Meeting Plus (ADMM-Plus) Experts Working Group on Military Medicine (EWG-MM). Singapore and Japan Co-Chaired the first cycle of the ADMM-Plus EWG-MM, which culminated in the finale exercise of the ADMM-Plus HADR/Military Medicine Exercise, held in Brunei Darussalam, in 2013. This was a significant milestone in the ADMM-Plus co-operation when for the first time, eighteen countries came together to participate in this exercise. The next full-troop exercise deployment under the ADMM-Plus EWG-MM ambit (co-chaired by Brunei Darussalam and Australia) took place in the Philippines in October 2023, where the SAF Medical Corps contributed a dental team to provide primary treatment and a CPR/BCLS trainer to train the local community healthcare workers in Basic Cardiac Life Support (BCLS) and use of an automated external defibrillator (AED).
In addition, the SAF Medical Corps routinely attends and present research findings at various military medical conferences and meetings. These include, but are not limited to, the ASEAN Chiefs of Military Medicine Conference (ACMMC), International Committee of Military Medicine (ICMM) World Congress on Military Medicine, the FDI World Dental Federation’s Section of Defense Forces Dental Services (SDFDS) meetings, and participating as an Observer Nation at the plenary meetings of the Committee of Chiefs of Military Medical Services in NATO. The SAF Medical Corps has also chaired and co-chaired regional military medical conferences, such as the Asia Pacific Military Health Exchange (now called the Indo-Pacific Military Health Exchange) with the US INDOPACOM in 2017, the Military Civilian Health Security Summit with the US INDOPACOM and the Australian Defence Force in 2022, and the Asia-Pacific Defense Forces Dentistry Forum in 2015.
The SAF Medical Corps also regularly participates in medical socio-civic missions to enhance defence relations with regional militaries. Social Civic Missions (SCM) have formed the bedrock of medical operations undertaken by the SAF Medical Corps throughout the years that regularly feature the deployment of medical, dental, and nursing/paramedic teams. The SAF medical teams deployed in SCMs would partner regional military counterparts to provide opportunistic healthcare for the local populace. Depending on the needs of the local populace, such missions may occasionally include the provision of complex treatments like cleft-lip repair, which would have been otherwise too costly for remote villagers. Dental deployments usually involve the provision of (1) school outreach oral health education programmes; (2) primary dental services, such as simple and complex dental extractions, fillings, scaling; and (3) sometimes even secondary dental services, such as wisdom teeth surgeries. These missions provide an excellent platform for practical cooperation and facilitate inter-operability amongst various medical services and enhance relationships with the partners in the region.
More recently, the SAF Medical Corps deployed an Emergency Medicine specialist and a Peri-operative nurse (who is also a paramedic and Independent Duty Corpsman) to provide medical support to Gazans affected by the ongoing Israeli-Hamas conflict. This two-man team deployed onboard the French Armed Forces’ hospital ship, the FS DIXMUDE, and contributed to the French Armed Forces’ medical humanitarian efforts. The team was mainly involved in the initial management of trauma patients which included post-operation wound management, management of infections, and administration of medications.

Photos: SAF Medical Team Treating Civilians from Gaza in Egypt.
(Source: The Straits Times, 22 January 2024)
Way Ahead for the SAF Medical Corps
The military and civil healthcare landscape is evolving rapidly, and the SAF Medical Corps will continue to transform herself to meet demands of operations and the healthcare needs of her soldiers. To this end, the SAF Medical Corps will adopt a fundamental shift in our healthcare philosophy to move “Beyond Healthcare to Health” by proactively maintaining the health of our servicemen rather than to provide treatment only when they are unwell, spanning pre-enlistment, active and reservist phases of our servicemen. The SAF Medical Corps will focus on force health readiness for the SAF’s full spectrum of operations through preventive health measures that cover both infectious diseases and non-communicable diseases and embark on a fundamental review of our medical classification system to optimise the deployment of every service personnel in support of the SAF. Second, the SAF Medical Corps will reorganise our healthcare delivery system from peace (primary and emergency care) to war (combat casualty care). The new delivery system will improve access to care, casualty flow, clinical quality, and patient experience.
The envisaged changes will be underpinned by two lines of efforts. Firstly, the SAF Medical Corps will work with our national healthcare partners to enhance overall healthcare surveillance and preparedness, sharing of data, as well as cooperation in the research space, looking into medical and dental disciplines, including but not limited to psychiatry, heat injuries, biodefence, musculoskeletal injuries, and dental conditions, and improved pedagogies in military medical education. Secondly, the SAF Medical Corps will focus our efforts in the developments of medical informatics – namely the modernisation of our PACES Electronic Health Record system, and the exploitation of longitudinal health data to inform medical policies and enhance quality of healthcare.
The SAF Medical Corps remains committed to her vision of being world class military medical service.
REFERENCES
- Huxley T. (2004) Defending the Lion City: The Armed Forces of Singapore. Talisman Publishing: Singapore.
- Lim HB, Tung B, Chong G. SAF’s force health transformation. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:18-24 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Jion I, Tan A, Ong SWX. Force medical protection in the SAF. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:58-65 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Poon BH. The Army combat casualty care system. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:25-30 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Gan WH, Lim S. Paradigm changes in aeromedical support for the Republic of Singapore Air Force. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:40-46 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Chow W, Liow MHL. Advancing maritime medical support for the Republic of Singapore Navy. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:31-39 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Teo KA, Chong TFG, Liow MHL, Tang KC. Medical support for aircraft disaster search and recovery operations at sea: the RSN experience. (2016) Prehospital and Disaster Medicine;31(3):1-6. PMID: 27018529https://doi.org/10.1017/S1049023X16000194
- Lo HY, Chia D. SAF Medical Training Institute – saving lives since 1966. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:47-57 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
- Tan PH, Wee KP, Sahelangi P. Remembering the Musi-SilkAir Flight MI 185 Crash Victim Identification. (2007) Annals of the Academy of Medicine Singapore;36:961-6. PMID: 17987240.
- Chong G. Forensic dentistry in the Singapore Armed Forces. Military-Medicine Journal. 04 Jan 2019. Available at: https://military-medicine.com/article/3629-forensic-dentistry-in-the-singapore-armed-forces.html
- Tan PH, Chew B, Lee CW, Tan B. A land untouched by dentistry - singapore brings dental care to afghanistan. (2011) Singapore Dental Journal; 32(1):39-48. Epub 2012 Jan 25. PMID: 23739286. https://doi.org/10.1016/S0377-5291(12)70015-9.
- Lee WT, Tan MY. Military Medical Operations in the SAF: A new paradigm. (2017) POINTER (Official journal of the Singapore Armed Forces) Monograph No.11:12-17 published to commemorate the 50th anniversary of the SAF Medical Corps. Available at: https://www.mindef.gov.sg/oms/imindef/publications/pointer/monographs/mono11.html
(status: 20th September 2024)











