
Almanac
Australia, Commonwealth of



Surgeon General Australian Defence Force / Command Joint Health
Sonya Bennett AM RAN
Rear Admiral
Source: Ministry of Defence Australia
Campbell Park Offices
Northcott Drive
CANBERRA ACT 2600
AUSTRALIA
Pictures and Graphics: Wikimedia Commons
The Military Health Services of Australia
Australia and Defence’s National Context and Summary
Australia is one of the largest countries in the world and is surrounded by water, lying between the Pacific and Indian oceans in the Southern Hemisphere. Australia’s population of around 26.6 million people is concentrated along the eastern coast. Australia’s immediate region is in the midst of the most consequential strategic realignment since the Second World War, and trends including military modernisation, technological disruption and the risk of state-on-state conflict are further complicating our nation’s strategic circumstances.
The Australian Defence mission is to defend Australia and its national interests in order to advance Australia’s security and prosperity. Defence is jointly led by the Chief of the Defence Force and the Secretary of Defence under a diarchy reporting directly to the Minister for Defence. Defence serves the Government of the day and is accountable to the Commonwealth Parliament, which represents the Australian people, to efficiently and effectively carry out the Government's defence policy. Defence consists of both the Australian Defence Force (ADF) and the Department of Defence. Command of the ADF sits under the direction of the Minister for Defence and is the primary responsibility of the Chief of the Defence Force. Defence facilities are staffed and operated in locations around the country; however, most of the senior leadership are located in Canberra.
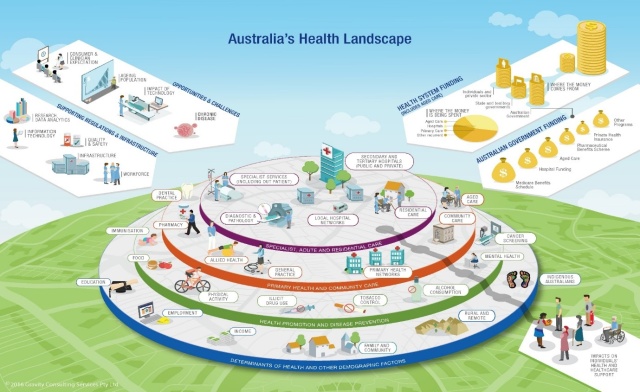
The Australian Health System
Australia’s Health System is one of the best in the world that provides quality, safe and affordable healthcare for its citizens. Medicare and the public hospital system provide government-funded or low-cost access for all Australians to most of these healthcare services. Private health insurance also provides a choice outside the public system for private healthcare.
Source: Australia’s health 2020: in brief – Australian Institute of Health and Welfare
(https://www.aihw.gov.au/reports/australias-health/australias-health-2020-in-brief/summary)
The Australian federal, state/territory, and local governments share responsibility for running the Australian health system. Australian government responsibilities include (but are not limited to): the Medicare and Pharmaceutical Benefits Schedules; supporting and regulating private health insurance; and supporting and monitoring the quality, effectiveness and efficiency of primary health care services. State/territory and local government responsibilities include (but not limited to): managing and administering public hospitals; delivering preventative services such as breast cancer screen and immunisation programs; and funding and managing community and mental health services. Shared responsibilities include (but not limited to): funding public hospital services; registering and accrediting health professionals; and responding to national health emergencies.
As a general rule, states and territories are guided by clinical service levels characterised by complexity of care. While the framework may differ depending on state and territory, the six clinical service levels tend to be similar. An example of these is provided in the following figure.
The Defence Health System
The Defence Health System includes both Operational and Garrison health support. Both Joint Health Command, Joint Operations Command and the Services (Navy, Army and Air Force) partner together to deliver health support and services that enables Australia’s warfighting capability. The responsibility for coordination of operations sits with Joint Operations Command, with the provision of operational health support being provided by the Services.
The ADF Health Strategy provides strategic direction for the health services across the ADF and guides resourcing decisions to ensure that activities (including business as usual activities) align with the objectives of the Strategy. The Strategy has two leading Pillars, [BTC1] [SPM2] Force Optimisation and Operational Health capability, with five Pillars supporting the achievement of the two lead Pillars. This ensures alignment of the strategy with Defence’s mission, Defence Corporate Plan and Defence Planning Guidance. These combine to achieve a ready, responsive and resilient Defence Health System. The two lead Pillars have stated end states, which if achieved would result in the Pillar objective being achieved. Seven key enablers are integral to supporting the achievement of the Strategy.
The Services provide technical and expert advice in military medicine. They advise Joint Health Command on reviews into their health workforce and on any training or exercise activities likely to require significant health resources.
Defence provides health care to keep ADF members medically and dentally fit to perform their military duties. Defence also provides health preparation for deployment, force optimisation, health support to operations, diagnosis and treatment of injury, illness or disability, and rehabilitation services to help ADF members return to duties or transition to civilian life.
Within the garrison setting, ADF members have access to the range of health services equitable with those provided to the Australian community including general practice, dental services, mental health and occupational psychology services, hospital care, allied health care and specialist services.
Defence will normally provide primary health care from on-base health facilities. Primary health care includes services such as preventive health, general practice, nursing, occupational medicine services, dental, mental health, occupational and clinical psychology, pharmacy, physiotherapy, collection of pathology specimens and occupational rehabilitation. In some areas, Joint Health Command provides low-acuity inpatient care. ADF members are able to access telephone-based triage and health advice 24 hours a day, 7 days a week.
Defence will normally provide access to specialised services through an off-base contracted network of health providers. Off-base specialised services include medical, dental, and mental health specialists, nursing and midwifery specialists, inpatient care, allied health services, optometry, imaging and radiology, and pathology. Garrison health personnel are responsible for providing the coordination of care, health administration and health record management that integrates the on-base and off-base health services to ensure end-to-end health care for ADF members.
The full spectrum of health care services and elective health care is not usually available within deployed environments. ADF members may be required to return to Australia or a nominated location for definitive care and, where required, Defence will provide strategic casualty evacuation to facilitate this care.
Reserve ADF members have access to the clinically necessary and relevant health services that directly enable operational preparedness for Defence activities. Joint Health Command also treats acute conditions as a result of military service when the member is unable to access the civilian health system.
Beneficiaries of Garrison health services include both permanent and reserve ADF members, foreign forces, Defence civilians and contractors, and veterans. Table 1 below provides additional detail.
Table 1. Beneficiaries of Garrison Health Services
Beneficiary | Definition | Number (as at 04 July 2024) |
Permanent | Full-time ADF members of the Navy, Army and Air Force, Reserve ADF members rendering Continuous Full-Time Service and ADF members or Reserve Forces rendering Continuous Full-Time Service in the ADF Gap Year program. | 59,310 (headcount) |
Reserve | Reserve ADF members who:
| 32,000+ (members rendering part time service) |
Foreign forces | Eligibility for Defence health services is based on the agreements that are established between Australia and the foreign nation. |
|
Veterans | Defence provides treatment and occupational rehabilitation services for illness, injury or conditions that are a consequence of Defence service until a claim is made by the Department of Veterans’ Affairs. On receipt of the determination, follow-on care is managed as follows:
|
|
Defence civilians and Contractors | Defence provides limited health support for the preparation of authorised civilians and contractors proceeding overseas on departmental business at Commonwealth of Australia expense. |
|
In addition to health service delivery, Defence also has a range of health and research capability. For example, the ADF Malaria and Infectious Diseases Institute (ADFMIDI) is a world recognised centre for malaria and infectious disease research and training. The ADFMIDI is a joint organisation that has close links with research and global health sectors, allied partners and Australian Government organisations. The ADFMIDI has a range of expertise and combination of military, public service and whole of government staff understanding studies in a range of areas including drug evaluation, vector surveillance and control testing, drug resistance diagnostics, clinical studies and surveillance, malaria research and arbovirology. Other health and research capability are listed in Table 2 below.
Table 2. Categories of Health Research and Training by Defence
Category | Description of Capability |
ADF Dental School | The School is responsible for the training of dental auxiliaries for the Navy, Army, and Air Force. The School conducts Dental Practice Manager training which focuses on requisite governance processes and staff management protocols, preparing members for oversight of a garrison dental practice. The School also conducts a familiarisation course for newly appointed Dental Officers that focuses on policy and procedures and various skillsets required when working in the ADF dental environment. |
Royal Australian Navy Medical School | The School provides Medical Officers, Nursing Officers and Medics with clinical skills and knowledge required to conduct Advanced Life Support in the maritime environment. |
Army School of Health | The School is a diverse training organisation delivering initial employment training, special health training and select career promotion courses to ADF members and Reserves. |
Health Operational Conversion Unit | The Unit delivers training to health practitioners for a range of specialisations and musterings for the delivery of health care supporting Air base operations and Aeromedical Evacuation. |
Submarine and Underwater Medicine Unit | The Unit provides expert advice on diving and submarine medicine to the ADF. The Unit also provides decompression for diving accident victims and the emergency medical system required in the event of a submarine accident. The Unit also supports the emergency treatment of civilians suffering from diving illnesses. |
Royal Australian Air Force Institute of Aviation Medicine | Commended by Air Force, the Institute is staffed by a mixture of uniformed and civilian personnel with diverse skills in Aviation Medicine, Human Factors, and Aeronautical Life Support. The Institute enhances the effectiveness and safety of ADF aviation through the provision of specialist advice in aviation medicine and fitness to fly, research into human factors and system integration and the provision of aviation medicine training to health professionals and aircrew. |
ADF Malaria and Infectious Diseases Institute | The Institute researches infectious diseases pertinent to the ADF in areas of operation and investigates measures to prevent mission failure due to infectious diseases. Areas of research include prevention and treatment of vector-borne disease through pharmacological agents or physical means. Australian Defence Force Malaria and Infectious Disease Institute |
Directorate of Health Research within the Health Protection and Policy Branch, JHC | The Directorate delivers high-quality research and supports rapid translation of research-based evidence to policy, programs and practice. The Directorate focuses on research of strategic priority to preserve the force, supporting ADF capability and optimising the physical, mental and environmental/occupational health of members over their life course. |
The ADF Health Research Framework 2021-2025 outlines the importance of health research to the ADF. The purpose of the Framework is to shape a pathway by which health research will transition from knowledge to action to maximise Defence capability.
The Framework recognises the importance of partnerships between the civilian academic sector, international partners and Defence, to optimise health research expertise and infrastructure. As implementation of the Framework has progressed, a number of academic partnerships have been funded to support the delivery of research that contributes to members’ health and ADF capability. This includes joint research projects across a number of domains, of particular note is collaboration and projects within the mental health and wellbeing domain. Defence has funded the appointment of a Professor of Military Mental Health who has led the development of a five-year programme of research in mental health and wellbeing (2023-27). The rationale of the programme is to prevent the onset and persistence of, and facilitate recovery from, mental health disorders to improve Defence’s ability to deploy ready members and reliably sustain their deployment. The Professor of Military Mental Health provides leadership in the pursuit of academic research linking best practice and innovation with policy development and service delivery.
Defence staff undertaking collaborative research projects are encouraged and supported to publish findings in a range of peer-reviewed journals including Military Medicine, Journal for Military and Veterans’ Health, and Psychological Medicine, in addition to internal Defence publications.
Overview of the ADF Health Research Framework 2021-2025
Operational Capabilities
In the Australian context, health support elements enable operational capability and maximise military effects by:
- Enabling a fit and healthy force
- Minimising preventable casualties.
- Providing wounded, ill and injured Defence members with safe and quality health support to optimise health outcomes.
- Providing healthcare, in accordance with medical rules of eligibility, to Defence civilians and other civilians deploying with or assigned to a joint task force.
- Providing healthcare to civilian populations to relieve human suffering.
- Providing healthcare to captured persons in accordance with International Humanitarian Law.
The image below illustrates the process of evacuation in the Joint Force Area of Operations (JFAO). Health support in a JFAO is task organised and designed to provide continuous care and evacuation of casualties. The role of healthcare defines the minimum clinical capability in a health facility, but does not define its capacity. Casualty regulation directs patients to facilities that can best manage the condition within appropriate timeframes. While ADF health capabilities provide independent health support to operations, they must also be capable of working in joint, multiagency and coalition environments alongside other military health elements, multi-national forces and civilian agencies.
Casualty Evacuation with en-route care
All aspects of operational (field) health support to ADF operations remain the responsibility of the individual Services – Navy, Army and Air Force. The Services are responsible to the Chief of the Defence Force to raise, train and sustain deployable health capability including personnel and equipment. Deployable health capabilities are then assigned to, and commanded by, Joint Operations Command for specific operational missions and exercises.
The Royal Australian Navy has Role 1 health support organic to its ships. It has the capacity to deliver Role 2 and Role 2 Enhanced capabilities through a small number of appropriately equipped ships within the fleet. This capability is currently provided through the Bay Class Landing Ship Dock HMAS Choules and the Canberra Class (Landing Helicopter Dock) Amphibious Assault Ships HMAS Canberra and Adelaide.
The Australian Army operational health capability is delivered via a Health Brigade establishment (2 Brigade). It force generates and provides the joint force four deployable Health Battalions with a focus on simplified Command and Control, Integrated Teams (full-time and part-time workforce) and aligned to Army’s future force structures. From a land component capability, as part of Joint Project 2060-Phase 3, 2 Brigade elements work closely with habitual sister Brigades and Aviation, Specialist and Special Forces capabilities. Army will introduce into service an entire new fleet of health materiel (including shelter solutions, medical equipment and power supply). The 2nd Brigade consists of:
- 1st Health Battalion – Close Health and Allied Health capabilities up to Role 1
- 2nd Health Battalion – Close and General Health capabilities up to R2E
- 3rd Health Battalion – Close and General Health capabilities up to R2E
- 4th Health Battalion – Close Health and Allied Health capabilities up to Role 1
The Royal Australian Air Force operational health capability is managed by its Health Services Wing consisting of an operational training unit, two Expeditionary Health Squadrons that can generate a deployable health capability up to Role 2 Enhanced and an Aeromedical Evacuation Squadron that provides a tactical and strategic Aeromedical Evacuation capability as part of the ADF Aeromedical Evacuation System. Tactical and strategic Aeromedical Evacuation is performed utilising a variety of fixed wing platforms including C-17 Globemaster, C-130J Hercules and C-27J Spartan aircraft.
Table 3. Medical operational capabilities.
Capability | Definition | Numbers | Description |
Role 2F (Fwd) | Mobile and deployable structures that may perform damage control resuscitation and damage control surgery in far-forward or unsecured environments. | 2-4 (tailored as required) | Generated from Army and RAAF operational health capabilities |
Role 2B (Basic/Small) | Mobile and deployable structures that may perform damage control resuscitation and damage control surgery. | Quantity depending on mission and task | Generated from Army and RAAF operational health capabilities |
Role 2E | Mobile and deployable structures that may perform damage control resuscitation and damage control surgery, along with expanded capabilities that may include x-ray equipment, blood banks, pharmaceutical supplies, and sterilisation equipment. | Quantity depending on mission and task | Generated from Army and RAAF operational health capabilities |
Role 3 | Deployable hospital and specialist care that incorporates CT technology and oxygen production. | 1 | Generated from Tri Service compliment depending on workforce and mission. ADF can contribute to Coalition facilities. |
Role 4 | Full-spectrum capabilities outside of the deployed environment that include reconstructive surgery, rehabilitation, and other specialized techniques. | Resides in the National Support Base | Exists within Australian Domestic health environment. |
Casualty Staging Units | Patient holding centres with nursing care that may hold and stabilize patients before transport between levels of care. | Multiple | Generated primarily via Army Land based units. |
Medical Emergency Response Team | Pre-hospital care teams that can provide care in non-combat operational environments. | Multiple – generated pending mission profile and task | Can be generated from ADF elements and Whole of Government health agencies |
Forward Evacuation | Transportation from the point of injury to an initial medical treatment facility. | Quantity not specified | Generated from ADF assets and links to Services |
Tactical Evacuation | Transportation from one medical treatment facility to another within the area of operations. | Quantity not specified | Generated from ADF assets and links to Services |
Strategic Evacuation | Transportation from medical facilities within the area of operations to medical facilities outside of the area of operations. | Quantity not specified. Range of different air platforms. | Generated via RAAF Health and Air capabilities. |
Maritime Evacuation Assets | Sea-based vehicles that may evacuate individuals from maritime or amphibious operations. | Quantity not specified | Generated from ADF assets and links to Services |
Land Evacuation Assets | Ambulances that can transport casualties over difficult terrain. | Quantity not specified. Range of land vehicle platforms. | Generated from ADF assets and links to Services |
Air Evacuation Assets | Rotary, or fixed wing assets such as helicopters and aircraft that may transport patients through the air. | Quantity not specified. Range of air platforms used. | Generated from ADF assets and links to Services (RW and FW assets) |
Since 1999, the ADF has deployed on over 100 operations.
Globally, the ADF has made significant contributions to coalition campaigns in the Middle East Area of Operations (including Iraq and Afghanistan).
Regionally, ADF personnel have operated in Timor Leste, the Solomon Islands and Bougainville. ADF personnel have also contributed to humanitarian assistance and disaster relief operations in the Philippines, Pakistan, Papua New Guinea, Indonesia, Solomon Islands, Tonga and Fiji as well as undertaking humanitarian assistance as specified by the Australian Government.
Domestically, the ADF has been involved in border protection operations, bushfire, flood and cyclone relief activities, counter-terrorism activities and the COVID-19 pandemic response.
The ADF is often called upon to contribute to highly specialised, niche medical capabilities, tailored to meet its obligations as part of a multinational force. ADF Health personnel are currently supporting forces deployed to multiple locations globally and regionally to support the Australian Government’s Regional Engagement initiatives. The ADF also extensively uses civilian health services and facilities throughout Australia, and engages with academia, and research organisations such as the Defence Science and Technology Group, the Australasian Military Medical Association, the Commonwealth Scientific and Industrial Research Organisation and others).
The ADF works in connection and collaboration with a range of military (partners, allies and neighbours) as well as civilian domestic and international organisations and maintains several partnerships to promote interoperability and knowledge sharing, including military medicine. Chief amongst these partnerships are the following treaties and alliances:
- Australia, New Zealand and United States Security Treaty (ANZUS)
- The ‘Five Eyes’ community, which includes Australia, Canada, New Zealand, the United Kingdom and the United States
- Five Power Defence Agreement (FPDA) between Australia, Malaysia, New Zealand, Singapore and the United Kingdom
- American, British, Canadian, Australian, and New Zealand (ABCA) Armies Program
Australia engages with ‘Five Eyes’ nations through a range of forums including The Technical Cooperation Program which provides an opportunity for sharing of ideas and focus on topics of strategic importance including, military medicine. In addition, Australia engages with international partners to support collaboration and research into topics of relevance to supporting military operations such as the ‘Five Eyes’ Military Exposures Working Group.
Although not a part of NATO, Australia maintains friendly nation status with this organisation and regularly contributes to knowledge sharing and lessons learnt initiatives. Australia and Japan also enjoy close working relationships on military matters, with the two nations maintaining Reciprocal Access Agreements.
The ADF has close engagement with regional partner nations to support interoperability, training, knowledge sharing and policy development. One example is ADF participation in Expert Working Group on Military Medicine within the architecture of the ASEAN Defence Ministers Meetings.
A further example of ADF health engagement is on policy and training development. The ADF maintains Allied Liaison status on the US Department of Defence Committee on Tactical Combat Casualty Care. Australia also works with other nations in the Indo-Pacific to strengthen regional cooperation in military medicine, most notably through research into tropical and infectious diseases (global engagement with ADFMIDI and the Indo-Pacific Centre for Health Security).
Military Medical Personnel
Over 4000 full and part-time ADF health personnel are employed as either doctors, nurses or allied health professionals.
The uniformed health workforce is supported by Australian Public Service (APS) employees employed in various clinical and health administration roles.
In addition to Defence’s uniform and APS health workforce, the ADF Health Services Contract provides workforce to support health service delivery in the Garrison and access to specialist and hospital care. This contract delivers on-site health services to Defence bases around Australia through the provision of approximately 1,500 clinicians and a national network of registered community-based providers consisting of Allied Health, Medical Specialists and hospitals.
Regardless of specialisation or level of qualification, all health ADF personnel go through an attestation process with Defence Force Recruiting. There are three pathways for entry into the ADF as a health professional: Graduate, Undergraduate, or general admission:
- Successful applicants who already hold professional qualifications and relevant accreditation enter service through graduate recruitment pathways designed to provide them with military training as soon as practicable after appointment, enabling them to provide military health support as early as possible.
- Undergraduate schemes take applicants part way through their studies and offer placement options upon graduation, allowing them to gain confidence and competence in their skills before integrating with units.
- The general entry pathway is utilised for in-house training options such as medics and dental technicians. Unlike Graduate and Undergraduate entry schemes, general entry enlistees complete their basic military training before conducting their specialist health training.
- The ADF also offers ab-initio training for a number of clinical trades including dental technicians, environmental health technicians, medics and physical training instructors through its own training institutions. ADF members obtain undergraduate and post-graduate health qualifications from civilian universities and other registered training organisations external to the ADF. These qualifications are realised through a combination of undergraduate recruitment schemes, single-service sponsorship and funded learning opportunities designed to meet service-specific needs.
The ADF also partners with a number of tertiary education providers to deliver research-driven, evidence-based clinical practice outcomes, designed to enhance the knowledge and application of military healthcare. To support the development of best-practice techniques, in 2011 the ADF established a Chair of Military Surgery and Medicine, integrated within the University of Queensland Burns, Trauma and Critical Care Research Centre. The research opportunities from this joint venture led to advancements in the clinical trials of cryopreserved blood products, enhanced research into predictors for successful outcomes in traumatic cardiac arrest and associations of needless repeated CT scans after transfer to major hospitals.
Civil-military relations
The Australian Civil-Military Centre (ACMC) supports national civil-military and policing capabilities to prevent, prepare for and respond more effectively to conflicts and disasters overseas. The ACMC structure focuses on concepts and capability, international and domestic engagement, business operations and governance and provision of advisors and seconded personnel. They support a range of effects including:
- Civil-military-police coordination
- Disaster management
- Women, peace and security
- Protection of Civilians
- Innovation and New Partnerships
- Leadership
- International Responses
- Humanitarian Action
- Advice services
A range of ACMC resources, publications and more information can be found at Resources | ACMC
The Defence Assistance to the Civil Community (DACC) is the formal mechanism that provides the means through which the ADF can assist State and Territory Governments, non-Defence organisations or agencies to deliver emergency or non-emergency support at a time when their own resources are not sufficient, have been overwhelmed, when no alternative for gaining this support is available or there is a mutually beneficial outcome for Defence in providing assistance. The DACC is provided via two classes – emergency assistance and non-emergency assistance. ADF members are called upon to support these efforts by Federal and State and Territory Governments.
Formal arrangements for DACC, including categories of support, policy and the DACC manual can be found at the Australian Government’s Department of Defence website.
An example of the Defence working within a civil-military medical operation is the response to COVID-19. From March 2020 to April 2022, the ADF’s Operation COVID-19 Assist contributed to the whole-of-Australian Government response to the COVID-19 pandemic, with customised support for state and territory authorities. Assistance from the ADF was coordinated through a whole-of-Australian Government emergency management response. Defence contributions included:
- Mandatory state and territory hotel quarantine program assistance for returning Australians and other international travellers.
- Emergency response planning assistance via embedded and reconnaissance planning teams.
- Police border controls logistics support.
- COVID-19 testing facility support.
- Contact tracing teams.
- Logistical support for civilian authorities.
Other DACC tasks, where the ADF provided health effects, include the response to the devastating 2019/2020 bushfires in eastern and southern Australia, support to the Aged Care sector in response to COVID-19 (2021-2022), and flood relief in Queensland and New South Wales (2022).
In terms of civil-military medical collaboration, under the ADF Health Strategy, the ADF maintains professional linkages with academic partners, industry, professional registration bodies, various national health associations and professional colleges in order to deliver a ready, responsive and resilient defence health system. In collaboration with the health industry and academic partners, the ADF works closely with these external stakeholders to ensure that the health capability of the ADF is well trained, prepared and equipped to meet current and emerging challenges.
table sources: Ministry of Defence Australia
(Status: 18 June 2025)











