
Article
Renal Denervation as an Innovative Treatment for Resistant Hypertension – a Survey
Department I - Internal Medicine - (Head of Department: Colonel (MC) Dr U. Baumgarten) of Bundeswehr Hospital Berlin1 (Hospital Commander: Commodore (MC) Dr K. Reuter), Department of Cardiology, Cardiac Centre of Leipzig University2 (Hospital Director: Professor Dr G. Schuler) and the Medical Department, Division of Cardiology and Angiology, Campus Mitte, Charité Hospital - University of Berlin3 (Temporary Head of Department: Professor Dr K. Stangl)
Summary
Background: Owing to its significant impact on cardiovascular mortality, arterial hypertension is highly relevant both for the public and the military health systems. Effective treatment of arterial hypertension, both in terms of prevention and therapy, thus takes on an important role. Despite the availability of a variety of antihypertensives, increased blood pressure persists in a significant proportion of patients as therapy-resistant arterial hypertension.
Renal sympathetic denervation (RSDN), which uses a catheter-based system for ablation of sympathetic nerve fibres located in the adventitia of the renal arteries, has been studied as an innovative therapeutic option for such patients, including with regard to its potential use in military medicine.
Methodology: A selective PubMed literature research focusing on randomised, prospective and controlled studies was performed. Furthermore, the results of our own research at the Heart Centre Leipzig and a consensus paper of the European Society of Cardiology published in 2013 were evaluated.
Results: The initial enthusiasm that followed the first two clinical studies was significantly tempered by the negative results of a randomised study (SYMPLICITY HTN-3). However, subsequent randomised studies have once more shown RSDN to be effective. All studies, however, have in common that a certain proportion of patients do not adequately respond to RSDN in terms of a reduction in blood pressure. Current research thus focuses both on improving the efficiency of denervation procedures through further development of technical aspects (such as innovative catheter procedures) and on identifying patient populations that may particularly benefit from RSDN. There are signs that patients with less severe changes in the vascular walls (as indicated by arterial stiffness) can benefit most from RSDN.
Discussion: Beside the proof of efficacy, more effective ablation techniques and appropriate patient selection are the focus of current research. Patient selection and clearly defined indications could play a key role in ensuring treatment success.
Conclusions: RSDN appears to be an innovative interventional therapy option for select patients with resistant arterial hypertension. The current state of research suggests that such patients can be found among Bundeswehr military personnel. Establishing RSDN capability at a Bundeswehr hospital with a hypertension clinic should thus be considered.
Keywords
Resistant hypertension, renal sympathetic denervation, predictors, catheter systems, arterial stiffness
Background
As the most significant cardiovascular risk factor, arterial hypertension is highly relevant to overall health [1]. Between 5 and 30% of all hypertensive patients have hypertension that is resistant to treatment [1]. That means their arterial hypertension cannot be reduced to normal levels despite adhering to treatment with three antihypertensives, including a diuretic agent [1]. Such resistant hypertension is associated with a risk of cardiovascular events that is 50% greater than that of patients whose hypertension responds to medication [2].
There is no detailed data on the prevalence of hypertension among German soldiers. However, studies of civilian populations suggest that hypertension should be considered relevant in military medicine.
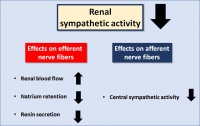 Simplified illustration of the effects of reduced renal sympathetic nerve activity (RSNA).
Simplified illustration of the effects of reduced renal sympathetic nerve activity (RSNA).
A study by Meisinger et al. analysed the differences in prevalence of hypertension in Germany, breaking it down by age groups. In the age groups relevant for the Bundeswehr (25–64 years), prevalence was 10–73.3% in men, while in women it was 4.2–60.7%. Approximately one fifth of hypertensive patients across all age groups took at least three antihypertensives [3]. A study in the US armed forces involving over 15,000 soldiers between the ages of 17 and 65 showed a hypertension prevalence of 13% on average, with that among the age group of 40–65 as high as 27.2% [4].
Based on these data and our own experience of everyday clinical practice in a Bundeswehr hospital, we can certainly assume that optimal treatment of hypertension is relevant for the German armed forces. Such treatment serves not only to preserve the health of the individual soldier but also to maintain the operational readiness of the Bundeswehr in general. The lack of relevant data does not permit definitive statements on the proportion of soldiers who have resistant hypertension.
About 50% of patients with resistant hypertension show evidence of hyperactivity of the sympathetic nervous system (SNS), particularly in the sympathetic fibres along the renal artery [5]. Increased activity of the sympathetic nervous system leads to increased renin secretion and thus to increased sodium retention [6]. This long-established connection was the reason why, in 1938, highly invasive surgical splanchniectomy was first performed in patients with severe hypertension [7]. Figure 1 shows the effects of reduced renal sympathetic nerve activity (RSNA).
Today, however, these nerve fibres in the adventitia of the renal arteries can be ablated in a minimally invasive, catheter-based and thus gentle intervention to reduce sympathetic nerve activity. This procedure is called renal sympathetic denervation (RSDN).
In recent years, RSDN has become a treatment option for patients with resistant hypertension. However, the initial enthusiasm based on preclinical [8–10] and clinical studies [11–14] has given way to a more cautious attitude as a result of the negative results of the largest randomised and blind controlled study yet (SYMPLICITY HTN-3). In that study, 535 patients were randomized at a ratio of 2:1 to RSDN (n = 364) or a sham procedure (i.e. only renal angiography) (n = 171). RSDN showed no advantage when it came to lowering blood pressure [15, 16]. The study result, potential causes and methodological flaws were discussed in detail in scientific societies and at cardiology congresses [17]. Studies that demonstrated a reduction in blood pressure and SYMPLICITY HTN-3 as well as subsequent studies, however, all share a certain proportion of non-responders to RSDN [13, 15, 18].
Patient selection is therefore the focus of current research to identify the population that could benefit most from RSDN and factors that influence ablation results.
The objective of this study is to give an overview of the current state of research.
Methodology
A selective literature search in PubMed was performed using the search term "renal denervation", with a particular focus on randomised, prospective, and controlled studies.
We were also able to use in-house research done by the working group around Desch and Lurz at the Heart Centre Leipzig.
It must be noted that for the purpose of this survey, patients were assumed to have essential hypertension. For the diagnostic procedure in case of suspected secondary hypertension, refer to recent survey studies [37].
Results
Using the search term "renal denervation" produced a total of 3,803 hits (as of 22 Dec 2016) for the period 1935–2016. Of these hits, we included any studies in English or German. In addition, a consecutive literature research was done on the basis of the references in original and survey studies, which were looked through personally. Clinical studies conducted after 2009 were given particular consideration. Also included in the literature research were animal studies and experimental studies. In particular, peer-reviewed studies published in journals with a high impact factor were consulted. Also included were statements issued by the European Society of Cardiology and the German Cardiac Society.
Procedural aspects of renal sympathetic denervation (RSDN)
 Illustration of the placement of the Simplicity catheter in the right (above) and left (below) renal artery.
Illustration of the placement of the Simplicity catheter in the right (above) and left (below) renal artery.
The antihypertensive effect of RSDN greatly depends on the success of ablation itself. The study by Kandzari et al. [20] shows a correlation between the number of ablations performed on a patient and a reduction in blood pressure. This is indicative of the importance of a technically effective procedure and appears plausible in terms of pathophysiology. In this context, knowledge of the anatomy of the nerve fibres is key. A post-mortem study by Roy could show that 77% of the nerve fibres of the sympathetic nervous system are located between 0.5 and 2.5 mm from the inside of the renal artery wall, while 22.5% are located between 2.5 and 4 mm from the inside of the renal artery wall. At the same time, nerve fibres were thicker the further they were located from the lumen [21]. Sakakura et al. were able to prove that nerve fibres are less dense in the distal segment than in the proximal segment. Nerve fibres in the distal segment, however, were also closer to the lumen of the renal artery [22]. On average, 75% of the nerve fibres were located within 4.28 mm of the lumen.
This could potentially have relevant implications for the placement of the ablation catheters, which might help in identifying particularly efficient procedures and techniques. Figure 2 shows the placement of the Simplicity catheter as an example.
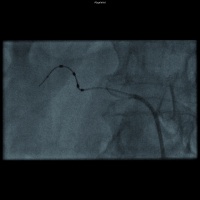 Example of ablation with a multielectrode catheter. Compared to figure 2, four electrodes (dark in the picture) are arranged here around a catheter wire in a spiral way. (Symplicity Spyral Catheter)
Example of ablation with a multielectrode catheter. Compared to figure 2, four electrodes (dark in the picture) are arranged here around a catheter wire in a spiral way. (Symplicity Spyral Catheter)
Beside radiofrequency energy delivery through a single point lesion (Fig. 2), several other techniques have emerged. There are, for instance, multi-electrode catheters such as the EnligHTNTM system (St. Jude Medical, St. Paul, MN, USA) [23] or the Symplicity Spyralä system by Medtronic (Minneapolis, MN, USA) (Fig. 3) [24]. Onetime circumferential ablation using the ReCor Paradise System (ReCor Medical PARADISE® Inc., Palo Alto, CA, USA) is another option. The system uses a cooled balloon and ultrasound to ablate sympathetic fibres [25]. There are also other, less widely used and less well-researched methods, such as cryoablation [26] or percutaneous ultrasound denervation [27]. Randomised studies that test the various systems with regard to any resulting lowering of blood pressure are not yet available. However, two studies have been published which were able to demonstrate that using a second procedure with another form of energy delivery has the effect of lowering blood pressure [26, 28].
The experience of the operator, which may affect placement of the ablation, also seems to play a role [20].
When it comes to the impact of the location of the ablation, Mahfoud et al. in a study on pigs showed denervation in the area of the distal renal artery and lateral branches to be the most effective method for reducing renal (cortical) noradrenaline levels [29].
Patient selection
Identifying patient populations that particularly benefit from RSDN is just as important as any efforts to improve the technical success of ablation. A retrospective analysis of the SYMPLICITY HTN-3 study revealed some patient-specific factors that influenced the level of response to RSDN. Patients with office hypertension were shown to benefit most from RSDN [20]. Although this may well seem plausible, it can more likely be explained by the statistical phenomenon of regression toward the mean. The study by Desch et al., however, showed that patients with mild hypertension (in the intention-to-treat analysis) benefit from RSDN, too, including when it comes to exercise blood pressure [13, 30].
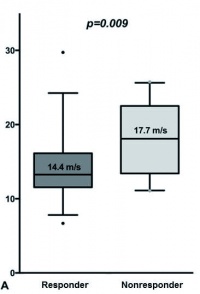 Comparison of the pulse wave velocities of responders (blood pressure reduction of at least 5 mmHg measured during the day (7:00–22:00 hrs) in 24-hour outpatient blood pressure monitoring) and non-responders. Non-responders show significantly higher pulse wave velocities.
Comparison of the pulse wave velocities of responders (blood pressure reduction of at least 5 mmHg measured during the day (7:00–22:00 hrs) in 24-hour outpatient blood pressure monitoring) and non-responders. Non-responders show significantly higher pulse wave velocities.
The working group around Ott et al. and the working group around Lurz/Desch et al. investigated the hypothesis that patients with increased arterial stiffness benefit less from RSDN. Ott et al. were able to support the hypothesis based on pulse pressure measurements (systolic pressure – diastolic pressure) [31]. Pulse pressure is a marker of arterial stiffness (in combination with isolated, systolic hypertension). Pulse wave velocity, however, is the gold standard for measuring arterial stiffness. A study from Leipzig showed that patients with increased pulse wave velocity benefit less from RSDN (based on the reduction in blood pressure determined in long-term outpatient blood pressure monitoring) (Fig. 4) [32]. Whether increased arterial stiffness is a result or a cause of hypertension, particularly of resistant hypertension, is a point of discussion in current research [33]. Mahfoud et al. were also able to produce congruent results, demonstrating RSDN had less of an effect in patients with isolated systolic hypertension [34].
The inclusion of African-Americans in the HTN-3 study has been discussed as another reason for the negative result. For one thing, African American participants were generally prescribed much higher doses of vasodilators. For another, among the sham group, African Americans experienced much greater decreases in blood pressure [15, 20]. A somewhat different pathophysiology and a distortion of results owing to differences in medication adherence have been discussed as potential reasons [15]. However, medication adherence is a fundamental factor that makes interpreting almost any denervation study difficult.
Furthermore, correlations between several biomarkers (sFLT-1, ICAM-1 and VCAM-1) and clinical response were found [35]. However, these biomarkers are usually not yet available in clinical practice and can furthermore be influenced by medication [36], so we currently see no clinical benefit.
Discussion
Preclinical and experimental studies showed RSDN to be successful in lowering blood pressure but those results could not be confirmed in a major randomized study. After the (unexpectedly) negative result of the SYMPLICITY HTN-3 study [15, 16], potential causes for this failure as well as predictors and factors of successful RSDN were thus thoroughly investigated.
Two major areas can be identified, which are not always clearly delineated, though. Firstly, there are the technical, procedural aspects of RSDN itself (not every RSDN is necessarily successful in terms of full denervation), including anatomic conditions. Secondly there is the issue of ideal patient selection.
Beside the purely technical innovations with regard to catheters themselves, a standardized ablation technique is vital to ensure that ablation is sufficiently successful in technical terms, which is a prerequisite for any clinical response. One limitation of the SYMPLICITY HTN-3 study certainly lies in the considerable proportion of inexperienced operators, as 30% of operators performed only one ablation and the success of ablation cannot be measured immediately after the intervention. The number of ablation spots as well as their location also seem to be a key factor in ablation effectiveness [20, 29].
We believe that more targeted patient selection would be a promising approach. Arterial stiffness is particularly relevant in this regard. Initial smaller studies already provide robust evidence that patients with less stiff arteries are more likely to benefit from RSDN. These patients are younger and have a lower prevalence of isolated systolic hypertension and diabetes than patients with greater arterial stiffness [32]. Overall, these results suggest that there is less arterial remodelling and thus correspond to the negative result of the SYMPLICITY HTN-3 study, in which more than 25% of patients already had coronary heart disease and 45% had diabetes and thus did not represent a patient population with less severe vascular wall changes. But just such patients with less arterial remodelling are presumably more common among Bundeswehr soldiers, so that this is where RSDN is likely to gain importance as a potential causal treatment of resistant hypertension.
Conclusion and prospects
Although the largest randomized, controlled study (SYMPLICITY HTN-3) yet did not show a significant difference between ablation and a sham procedure when it came to lowering blood pressure, we must not lose sight of RSDN as an innovative treatment of resistant hypertension. Numerous studies that focus on ablation technique and in particular on the issue of appropriate patient selection suggest this.
Continued application of renal sympathetic denervation (RSDN) will certainly depend on randomized studies yet to be completed. However, RSDN seems to be emerging as a potentially effective treatment option for a select patient population. Two large-scale studies are currently ongoing: (SPYRAL HTN OFF MED Study [NCT02439749] and SPYRAL HTN ON MED Study [NCT02439775]). A total of 240 patients (100 in HTN ON MED; 120 in OFF MED) are randomized at a ratio of 1:1 to either RSDN or a sham procedure. In the SPYRAL HTN ON MED study, participants take a thiazide, a potassium channel blocker, and an ACE inhibitor / angiotensin receptor blocker (ARB). This standardization is intended to prevent potential bias, such as the difference in vasodilator intake between African Americans and non-African Americans in the HTN-3 study. The effect of RSDN in medicated patients is conclusively investigated using a strict study design. What is interesting is that in the SPYRAL HTN OFF MED study, antihypertensives are discontinued prior to denervation while patients are closely monitored. Should systolic office blood pressure remain below 180 mmHg, the patients are randomized. After three months, antihypertensive medication is reintroduced in both groups, if required. The US Food and Drug Administration, among others, had called for such a study design. In this design, the effect of RSDN alone on hypertension can be examined, independent of any changes in antihypertensive medication adherence. This strict study design will help avoid the limitations of previous studies and conclusively determine the currently disputed effectiveness of RSDN in treating resistant hypertension.
Keeping a close eye on the further development of RSDN as a potential treatment option for soldiers with resistant hypertension appears to be in the best interest of military medicine.
Key statements
- Treatment of hypertension as a cardiovascular risk factor is a common and relevant issue for members of the German armed forces, too.
- For some years, the innovative intervention method of renal sympathetic denervation (RSDN) has been available in addition to medication for patients with resistant hypertension.
- As a result of a negative study, the initial enthusiasm surrounding this method gave way to scepticism and reluctance.
- Recent studies, however, appear to have identified patients who may particularly benefit from RSDN. This likely includes patients with less severe vascular wall changes – patients who are likely to account for a large proportion of Bundeswehr soldiers.
- Establishing the capability to perform RSDN in a Bundeswehr hospital with a hypertension clinic should be considered if the next few major studies produce positive results.
References
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34(28):2159-2219.
- Daugherty SL, Powers JD, Magid DJ, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012;125:1635-1642.
- Meisinger C, Heier M, Volzke H, et al. Regional disparities of hypertension prevalence and management within Germany. J Hypertens 2006;24:293-239.
- Smoley BA, Smith NL, Runkle GP. Hypertension in a population of active duty service members. JAM Board Famil Med 2008;21(6):504- 511.
- Esler M, Lambert E, Schlaich M. Point: Chronic activation of the sympathetic nervous system is the dominant contributor to systemic hypertension. Journal of applied physiology (Bethesda, Md : 1985) 2010;109:1996- 1998; discussion 2016.
- DiBona GF, Esler M. Translational medicine: the antihypertensive effect of renal denervation. American J Physiol Regul Integr Comp Physiol 2010;298(2):R245- 253.
- Smithwick RH, Thompson JE. Splanchnicectomy for essential hypertension; results in 1,266 cases. JAMA 1953;152:1501-1504.
- Schlegel F, Daneschnejad SS, Mavlikeev M, et al. Early effects in perivascular nerves and arterial media following renal artery denervation. Hypertension 2014;63:e123- 125.
- Rippy MK, Zarins D, Barman NC, Wu A, Duncan KL, Zarins CK. Catheter-based renal sympathetic denervation: chronic preclinical evidence for renal artery safety. Clin Res Cardiol 2011;100(12):1095- 1101.
- Steigerwald K, Titova A, Malle C, et al. Morphological assessment of renal arteries after radiofrequency catheter-based sympathetic denervation in a porcine model. J Hypertens 2012;30:2230- 2239.
- Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009;373:1275-1281.
- Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010;376:1903-9.
- Desch S, Okon T, Heinemann D, et al. Randomized sham-controlled trial of renal sympathetic denervation in mild resistant hypertension. Hypertension 2015;65:1202-8.
- Azizi M, Sapoval M, Gosse P, et al. Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 2015;385:1957-1965.
- Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014;370:1393- 1401.
- Bakris GL, Townsend RR, Liu M, et al. Impact of Renal Denervation on 24-Hour Ambulatory Blood Pressure: Results From SYMPLICITY HTN-3. J Am Coll Cardiol 2014;64:1071-1078.
- Böhm M, Hamm CW, Kuck KH, Ertl G, Mahfoud F, Schunkert H. Stellungnahme der Deutschen Gesellschaft für Kardiologie zu der Symplicity HTN-3-Studie bei Patienten mit resistenter arterieller Hypertonie nach renaler Denervation. Kardiologe 2014;8:244- 245.
- Mahfoud F, Ukena C, Schmieder RE, et al. Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation 2013;128:132 - 140.
- Mahfoud F, Luscher TF, Andersson B, et al. Expert consensus document from the European Society of Cardiology on catheter-based renal denervation. Eur Heart J 2013;34:2149- 2157.
- Kandzari DE, Bhatt DL, Brar S, et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J 2015;36:219- 227.
- Roy AK, Fabre A, Cunningham M, Buckley U, Crotty T, Keane D. Post mortem study of the depth and circumferential location of sympathetic nerves in human renal arteries--implications for renal denervation catheter design. Catheterization and Cardiovascular interventions 2015;86(2):E32- 37.
- Sakakura K, Ladich E, Cheng Q, et al. Anatomic assessment of sympathetic peri-arterial renal nerves in man. J Am Coll Cardiol 2014;64:635- 643.
- Worthley SG, Tsioufis CP, Worthley MI, et al. Safety and efficacy of a multi-electrode renal sympathetic denervation system in resistant hypertension: The EnligHTN I trial. Eur Heart J 2013;34:2132-2140.
- Whitbourn R, Harding SA, Walton A. Symplicity multi-electrode radiofrequency renal denervation system feasibility study. EuroIntervention 2015;11:104-109.
- Mabin T, Sapoval M, Cabane V, Stemmett J, Iyer M. First experience with endovascular ultrasound renal denervation for the treatment of resistant hypertension. EuroIntervention 2012;8:57-61.
- Prochnau D, Heymel S, Otto S, Figulla HR, Surber R. Renal denervation with cryoenergy as second-line option is effective in the treatment of resistant hypertension in non-responders to radiofrequency ablation. EuroIntervention 2014;10:640- 645.
- Neuzil P, Ormiston J, Brinton TJ, et al. Externally Delivered Focused Ultrasound for Renal Denervation. JACC Cardiovascular interventions 2016;9:1292- 1299.
- Stiermaier T, Okon T, Fengler K, et al. Endovascular ultrasound for renal sympathetic denervation in patients with therapy-resistant hypertension not responding to radiofrequency renal sympathetic denervation. EuroIntervention 2016;12:e282- 289.
- Mahfoud F, Tunev S, Ewen S, et al. Impact of Lesion Placement on Efficacy and Safety of Catheter-Based Radiofrequency Renal Denervation. J Am Coll Cardiol 2015;66:1766- 1775.
- Fengler K, Heinemann D, Okon T, et al.: Renal denervation improves exercise blood pressure: insights from a randomized, sham-controlled trial. Clinical Res Cardiol 2016; 105: 592.
- Ott C, Mahfoud F, Schmid A, et al.: Central pulse pressure predicts BP reduction after renal denervation in patients with treatment-resistant hypertension. EuroIntervention 2015;11(1):110- 116.
- Okon T, Rohnert K, Stiermaier T, et al.: Invasive aortic pulse wave velocity as a marker for arterial stiffness predicts outcome of renal sympathetic denervation. EuroIntervention 2016;12(5):e684- 692.
- Mitchell GF: Arterial stiffness and hypertension: chicken or egg? Hypertension 2014;64:210- 214.
- Mahfoud F, Bakris G, Bhatt DL, et al.: Reduced blood pressure-lowering effect of catheter-based renal denervation in patients with isolated systolic hypertension: data from SYMPLICITY HTN-3 and the Global SYMPLICITY Registry. Eur Heart J 2016; DOI; 10.1093/eurheartj/ehw325 (Epub ahead of print).
- Dorr O, Liebetrau C, Mollmann H, et al.: Soluble fms-like tyrosine kinase-1 and endothelial adhesion molecules (intercellular cell adhesion molecule-1 and vascular cell adhesion molecule-1) as predictive markers for blood pressure reduction after renal sympathetic denervation. Hypertension 2014;63:984-990.
- Schlaich M. Biomarkers for the prediction of blood pressure response to renal denervation: a long way to go. Hypertension 2014;63:907- 908.
- Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J 2014;35:1245-54.
The authors declare that there are no conflicts of interest.
Citation:
Okon T, Fengler K, Wenke B, Baumgarten U, Spethmann S: Renal Denervation as an Innovative Treatment of Resistant Hypertension–a Survey. Wehrmedizinische Monatsschrift 2017; 61(5): XXX-YYY
For the Authors:
Commander (MC) Dr. Sebastian Spethmann
Department I – Internal Medicine, Cardiology and Angiology Section,
Bundeswehr Hospital Berlin
Scharnhorststr. 13, 10115 Berlin
Email: [email protected]
Date: 07/30/2017
Source: Wehrmedizinische Monatsschrift 2017/5










