
Article
Non Operative Management of Gunshot Wounds to the Cervical -Trachea with Significant Tissue Loss and 3D Tracheography as a -Diagnostic Tool: 2 Case Reports
From the Department of Surgery1 and the Department of Radiology2 of the Chris Hani Bragwanath Academic Hospital – Universtity of Witwatersrand Medical School, Johannesburg, Republic of South Africa, and the Department of Surgery/Procto Surgery3 (Director: Priv.-Doz. Dr. D. Doll) of the St.-Marien-Hospital Vechta, Germany (Medical Director: Dr. O. Hagemann)
Summary
Background: Selective conservative treatment of penetrating open tracheal injury with substantial tissue loss has not been described up to now.
Case reports: We report two cases of tracheal defects following gunshot wounds in zone II of the neck. Patients and their wound healing were supervised clinically and followed by 3 dimensional CT (3DCT) reconstruction. Both defect wounds from gunshots healed without defect over a length of 2.5 cm under conservative therapy.
Discussion: Patients with penetrating tracheal trauma with significant tissue loss have been excluded from conservative treatment by now. Our cases show that there may be a subgroup of patients who would benefit from selected non operative management (SNOM) of this type of trauma. 3D tracheography has the potential to define – in addition to the clinical aspects – radiological characteristics for selection of patients with penetrating tracheal trauma for SNOM.
Conclusion: Certain tracheal defects seem to be amenable for SNOM treatment. Common aspects from these 2 patients are compiled, which need to be validated in further treatments.
Keywords: tracheal injury, gunshot wound, tracheal defect, SNOM, conservative treatment, 3DCT
Background
Isolated non iatrogenic tracheal injuries are uncommon. In many instances, tracheal injuries are often associated with oesophageal or vascular injuries and have traditionally been treated with surgical exploration and repair [7]. Newer imaging modalities, including computer tomography (CT) with 3D CT reconstruction imaging have resulted in excluding associated injury without the need for operative intervention and diagnosing and describing tracheal injury. 3D reconstructions of CT images in diagnosing tracheal injury have been shown to be comparable to bronchoscopy. Conservative (non-operative) management of penetrating tracheal injuries, described mostly for iatrogenic injuries, have become more acceptable as a definitive form of treatment if certain clinical and endoscopic criteria are met [3].
We present 2 cases of isolated tracheal firearm injuries with ventral defects up to 2.5 cm that were successfully managed conservatively. Tracheobronchial injuries described as being successfully managed conservatively in case reports and reviewed articles were mostly caused by iatrogenic penetrating or blunt injuries and not by gunshot wounds. We describe two cases of extensive isolated gunshot injuries of the trachea that were treated conservatively using 3D reconstruction CT images for diagnosis and follow up. These images gave us the opportunity to view the tracheal lumen from inside and made bronchoscopy unnecessary.
Case Description
Case 1

A 24 years old man presented with four gunshot wounds to the neck and one gunshot wound to the right upper arm. On examination the patient was haemodynamically stable and maintaining his airway. His trachea was central and he was breathing comfortably. There was tenderness and swelling in the midline of the neck but no odynophagia or haemoptysis. Surgical emphysema was palpable over the neck and there was bubbling on coughing from the superior right sided neck gunshot wound in zone II. Chest examination was within normal limits. The patient underwent a low dose X-ray (Lodox®) examination that confirmed the surgical emphysema of the neck and a normal chest.
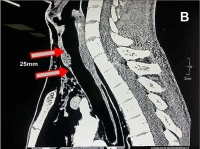
A CT angiogram of the neck and upper chest showed an anterior defect of the cervical trachea at the level of the 2 - 4th tracheal rings. The length of the defect was 2.5 cm and the width was 1 cm (Figure 1 A-B), with little soft tissue protrusion into the trachea (Figure 1 B-C). There were no associated pneumothorax, vascular, or oesophageal injury, as the bullet tract was away from the oesophagus.
The patient was advised by the trauma team on call to undergo surgical exploration of his trachea but refused as he did not have any significant symptoms. He was therefore admitted in the high care area for observation.
A 3D reconstruction of the CT confirmed the injury. He remained free of significant symptoms and signs and was discharged home on day 8 post injury after a further 3D reconstruction CT scan on day 7 showing significant healing of the injury. The patient was reviewed on day 14 when a further 3D reconstruction CT showed resolution of the injury. Figure 2 comparatively demonstrates the 3D CT reconstructed views of the trachea on day 1, 7 and 14. The patient was reviewed 3 months, 6 months and 1 year after the injury and he was free of any symptoms.
Case 2
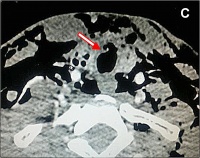 Figure 1: (A) Axial view of tracheal defect shows anterior loss of tracheal circumference on CT scan. A remaining bridge of tracheal
cartilage is seen anteriorly on the right. (B) Sagittal view shows a 2.5
cm longitudinal and a 1cm wide anterior defect of the trachea. (C)
Coronal view shows the defect with moderate soft tissue protruding into the tracheal lumen.
Figure 1: (A) Axial view of tracheal defect shows anterior loss of tracheal circumference on CT scan. A remaining bridge of tracheal
cartilage is seen anteriorly on the right. (B) Sagittal view shows a 2.5
cm longitudinal and a 1cm wide anterior defect of the trachea. (C)
Coronal view shows the defect with moderate soft tissue protruding into the tracheal lumen.
A 52 years old male patient presented 5 weeks after the first patient (case 1) with four gunshot wounds – three to the neck and one to the left flank. Of the 3 gunshot wounds to the neck, 2 were posteriorly seemingly forming a tract from left to right over the upper part of the trapezius muscle. The third gunshot wound was anterior over the midline 3 cm distal to the larynx in zone II of the neck. The patient showed a small amount of surgical emphysema over the base of his neck. He was haemodynamically stable with neither haemoptysis, dyspnoea or odynophagia, only some hoarseness was present.
On coughing there was no bubbling from the wound. The patient underwent a low dose X-ray (Lodox® AP and lateral) examination that revealed a bullet lodged in the right supraclavicular fossa just above the distal third of the right clavicle and another bullet lodged over the paravertebral muscles on the left. There were no signs of a pneumothorax.
Intravenous contrast CT scans of the neck, chest and abdomen were performed and revealed a 0.5 cm x 1 cm anterior tracheal injury. As the anterior bullet tract of the neck could not be clearly identified on CT scan, a Hexabrix® swallow to exclude oesophageal injury was performed which excluded any breach of integrity of the oesophagus.
In view of the fact that the previous patient (case 1), who had a significant loss of tracheal tissue and was managed successfully without need for surgery, it was decided to manage this patient (case 2) in a similar way. Figure 3 shows the progress of the injury on 3D CT views that were performed on day 1, 7 and 14.
The patient was discharged on day 8 after having a direct laryngoscopy that showed normal vocal cord movement. The patient was followed up for a year and remained asymptomatic.
Discussion
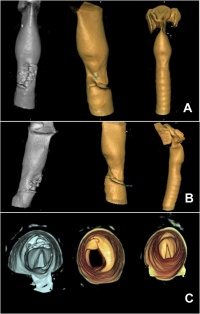 Figure 2: 3D reconstruction CT case 1; (A) anterolateral serial 3D CT
reconstructed views taken on day 1, 7 and 14 of the airway demonstrating
a defect in the trachea, anterolaterally and its healing process over the 2 week period; (B) lateral 3D CT views done on day 1, 7, 14 showing the healing process of the defect; (C) 3D CT reconstructed views showing the lumen of the trachea from inferiorly; the damaged cartilage is seen anteriorly (10 - 12 ò clock) and distal to the vocal cords on the first scan (day 1) and the repair process with the end
result can be seen on the second and third scan (day 7 and 14).
Figure 2: 3D reconstruction CT case 1; (A) anterolateral serial 3D CT
reconstructed views taken on day 1, 7 and 14 of the airway demonstrating
a defect in the trachea, anterolaterally and its healing process over the 2 week period; (B) lateral 3D CT views done on day 1, 7, 14 showing the healing process of the defect; (C) 3D CT reconstructed views showing the lumen of the trachea from inferiorly; the damaged cartilage is seen anteriorly (10 - 12 ò clock) and distal to the vocal cords on the first scan (day 1) and the repair process with the end
result can be seen on the second and third scan (day 7 and 14).
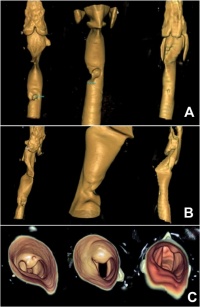 Figure 3: 3D reconstruction CT case 2; (A) Serial 3D reconstructed CT images done on day 1, 7 and 14 displaying the anterior tracheal injury with the defect progressively diminishing in size, accompanied by mild anterior scarring; (B) lateral 3D CT views done on day 1, 7 and 14 demonstrating progressive healing with conservative treatment; (C) 3D CT reconstructed views of the tracheal lumen inferiorly
to the vocal cords (day 1, 7, 14) with minimal residual defect noted on last follow up image on day 14.
Figure 3: 3D reconstruction CT case 2; (A) Serial 3D reconstructed CT images done on day 1, 7 and 14 displaying the anterior tracheal injury with the defect progressively diminishing in size, accompanied by mild anterior scarring; (B) lateral 3D CT views done on day 1, 7 and 14 demonstrating progressive healing with conservative treatment; (C) 3D CT reconstructed views of the tracheal lumen inferiorly
to the vocal cords (day 1, 7, 14) with minimal residual defect noted on last follow up image on day 14.
Isolated penetrating tracheal injuries can be life threatening and are associated with significant morbidity and mortality. Penetrating injuries, with loss of minor tissue and lack of respiratory problems, are often treated conservatively. This is the case with a large proportion of patients with stab wounds or iatrogenic injuries. Non-operative management recently has become more acceptable as a definitive form of treatment, mostly based on the experience in the managing iatrogenic injuries and reported only in case reports and reviews [2, 11, 13, 14, 15]. Particularly for iatrogenic injuries there is an increase in incidence due to the increase in diagnostic and therapeutic investigations in the tracheobronchial tree [2, 3]. Certain criteria, both clinical and endoscopic, have been proposed to be used as guidelines for non-operative treatment [11, 13]. These criteria base on the fact that the patient has stable vital signs, does not have any evidence of other significant injury related to the vital surrounding structures or evidence of complications. The application of these criteria leads to good outcomes but the type of the injury they are recommended for, are mostly tracheal tears or lacerations at the ventral face of the trachea, not exceeding 2 - 3 cm of length (ALTINOK and CAN postulate that conservative treatment is possible up to defect of 4 cm, but do not give any reason for this postulate within their review [1]). Open tracheal injuries have been excluded from conservative management though [3].
In our literature research, we have not yet found any records recommending conservative management in physiologically stable patients with penetrating tracheal trauma associated with significant tracheal tissue loss [3]. Until recently these injuries have been treated by resection of the defect and primary anastomosis (with or without distal tracheostomy) or with fashioning of a tracheostomy through the defect if it is in a technically convenient site on the trachea. We present 2 cases of penetrating trauma of the cervical trachea due to gunshot with significant tissue loss that were treated conservatively (In the first case a 2.5 cm injury and the second a 1 cm injury as measured on CT scan). There were no other clinical significant signs or symptoms other than subcutaneous emphysema. According to our unit protocol both patients with these injuries should have been operated on. The refusal of the first patient to undergo surgery mandated us to treat him conservatively. This lead to complete healing of the injury, demonstrated with serial 3D CT reconstructions and with satisfactory results during a year of follow up.
At this point it is worth mentioning that the advent of 3D CT reconstructions (also called 3D tracheography) can present an intraluminal view of the trachea and the larynx. It has been useful in diagnostics and – in follow up examination of tracheal injury – has proven comparability with bronchoscopy in defining tracheal injury, and it has certain advantages [12]. That includes the ability to be performed without the risk of potential desaturation, it can be evaluated retrospectively, it can reveal structural abnormality even at a point where bronchoscopy can hardly detect it- such as just below the vocal cords in non-intubated patients or outside the tracheal wall in intubated patients [5]. Furthermore, it can be performed without patient discomfort but with large specificity and sensitivity (75 % and 84 %) [6]. Having experienced the outcome of these two patients we are wondering if other patients, with similar clinical pictures, should be treated non-operatively even if tissue loss is found on CT scan.
We accept that our suggestion is based on the management of only 2 patients and we understand that possible failure of the treatment, leading to delayed repair, can lead to poor outcome [3, 11, 13, 14]. On the other hand, we are wondering if this risk is significant high enough to necessitate early operative management for all patients with this type of injury. What will be the clinical and radiological characteristics necessitating operative management? Is there a subgroup of these patients who would benefit from non-operative treatment?
Literature about conservatively treated isolated tracheal injury is exquisitely scarce, if not to say void [17]. Estimates are as low as 0.5 % of tracheal injuries in patients with multiple injuries treated major trauma centers [1]. Most of tracheobronchial injuries are of iatrogenic origin, and the majority of the non-iatrogenic cases is resulting from blunt mechanism [10]. While KISER et al. managed to accumulate an impressive number of tracheal injuries reported in the literature between 1873 and 1996 with n=265, only 36 of them were other than blunt injuries. Furthermore, only 4/265 touched the cervical trachea 2 cm above the carina and higher up [8]. This is also true for MADDEN, who analysed 643 tracheal injuries. He describes that most of them do occur within the 2,5 cm vincinity above the carina and further below [10]. While surgical access to and repair of the tracheal defect may be feasible up to a defect length of 2 cm, healing primarily depends on concomitant injuries of the surrounding soft tissues.
Small defects have been attempted to close with stenting or glue or a combination of both, which is associated with relatively small additional surgical trauma [4]. Nevertheless, any penetrating neck wound with the suspicion of vascular, tracheal or esophageal involvement has to be surgically explored thoroughly even bilaterally, as the benefits of early detection outweigh the sequelae of infection and attempted late repair (if possible at all) by far [16]. Up to now in cases of larger tracheobronchial defects only surgical treatment is recommended [13]. Following careful debridement und mobilisation, proper surgical closure with interrupted non resorbable sutures is applied. A flap interposition of sternocleidoid muscle may be useful to cover the trachea as to separate trachea from the injured esophagus [9]. In selected cases of isolated penetrating tracheal defects, a deviant pathway may be followed successfully, as it was demonstrated by our two case reports.
Conclusions
It is not the purpose of this report to recommend conservative management of gunshot injuries of the trachea as standard practice, but to give food for thought for the management options of future patients with this type of injury.
Table 1: Common parameters of tracheal injuries treated conservatively
- patient is perfectly hemodynamically stable
- defect not longer than 3 cm
- defect of not more than 25 % of circumference
- tracheal injuries in zone I or II, facing the ventral side
- no concommittant esophageal injury
We also know that “old habits die hard” and this “death” cannot occur with only two cases reported. There is therefore a need to have multicentre experience reported to enable us to come to a solid conclusion on the management of this type of injury.
References
- Altinok T, Can A: Management of tracheobronchial injuries. Eurasian J Med 2014; 46(3): 209 - 215.
- Carretta A, Melloni G, Bandiera A et al.: Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries. World J Surg 2011; 35(11): 2568 - 2574.
- Gomez-Caro A, Ausin P, Moradiellos FJ et al.: Role of conservative medical management of tracheobronchial injuries. J Trauma 2006; 61(6): 1426 - 1434; discussion 1434 - 1425.
- Huh J, Milliken JC, Chen JC: Management of tracheobronchial injuries following blunt and penetrating trauma. Am Surg 1997; 63(10): 896 - 899.
- Jones CM, Athanasiou T, Nair S et al.: Do technical parameters affect the diagnostic accuracy of virtual bronchoscopy in patients with suspected airways stenosis? Eur J Radiol 2005; 55(3): 445 - 451.
- Jones CM, Athanasiou T: Is virtual bronchoscopy an efficient diagnostic tool for the thoracic surgeon? Ann Thorac Surg 2005; 79(1): 365 - 374.
- Kelly JP, Webb WR, Moulder PV et al.: Management of airway trauma. I: Tracheobronchial injuries. Ann Thorac Surg 1985; 40(6): 551 - 555
- Kiser AC, O’Brien SM, Detterbeck FC: Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001; 71(6): 2059 - 2065.
- Lyons JD, Feliciano DV, Wyrzykowski AD, Rozycki GS: Modern management of penetrating tracheal injuries. Am Surg 2013; 79(2): 188 - 193.
- Madden BP: Evolutional trends in the management of tracheal and bronchial injuries. J Thorac Dis 2017; 9(1): E67 - E70.
- Massard G, Hentz JG, Wihlm JM. Iatrogenic tracheobronchial injuries. Reply [Letter]. Ann Thorac Surg 1998 ; 65: 1838.
- Moriwaki Y, Sugiyama M, Matsuda G et al.: Usefulness of the 3-dimensionally reconstructed computed tomography imaging for diagnosis of the site of tracheal injury (3D-tracheography). World J Surg 2005; 29(1): 102 - 105.
- Ross HM, Grant FJ, Wilson RS, Burt ME: Nonoperative management of tracheal laceration during endotracheal intubation. Ann Thorac Surg 1997; 63(1): 240 - 242.
- Schneider T, Volz K, Dienemann H, Hoffmann H: Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg 2009; 8(5): 571 - 576.
- Self ML, Mangram A, Berne JD et al.: Nonoperative management of severe tracheobronchial injuries with positive end-expiratory pressure and low tidal volume ventilation. J Trauma 2005; 59(5):1072 - 1075.
- Velmahos G, Degiannis E, Doll D. (Eds): Penetrating Trauma. A Practical Guide on Operative Technique and Peri-Operative Management. (2nd ed.) Springer Berlin Heidelberg London New York. Springer Berlin Heidelberg London New York: Springer, 2017.
- Welter S, Hoffmann H: Injuries to the tracheo-bronchial tree. Zentralbl Chir 2013; 138(1): 111 - 116.
Origin of all pictures: Department of Radiology of the Chris Hani Bragwanath Academic Hospital – Universtity of Witwatersrand Medical School, Johannesburg, Republic of South Africa
Citation:
Jennings VA, Dietrich Doll D, Daya S, Elias Degiannis E: Non Operative Management of Gunshot Wounds to the Cervical Trachea with Significant Tissue Loss and 3D Tracheography as a Diagnostic Tool: 2 Case Reports. Wehrmedizinische Monatsschrift 2017; 61(9/10): 240 - 244.
For the authors:
Lieutenant Colonel (Res.) Priv.-Doz. Dr. Dietrich Doll
Department of Surgery / Proctosurgery
Sankt-Marien-Hospital Vechta
Teaching Hospital of the MHH Hannover
Marienstr. 6 - 8, D- 49377 Vechta
E-Mail: [email protected]
Date: 09/06/2017
Source: Wehrmedizinische Monatsschrift 2017/9-10











