
Article: MCM BRICKNELL, AJ WALKER (UK)
The Operational Patient Care Pathway
This paper introduces the UK Defence Medical Services Operational Patient Care Pathway.
The Operational Patient Care Pathway is a unified approach for clinical care to all operational patients arising from the Defence Population at Risk (PAR), exposed to the ‘all-hazards environment’, deployed on military operations. It comprises three organisational models: the Healthcare Cycle, the Chain of Care and the Operational Patient Care Pathway. It is supported by a number key definitions including: the ‘All Hazards Environment’, the Defence Population at Risk, and the 7 Capabilities of Operational Healthcare. Key new clinical concepts include: Tactical Field Care, Care under Fire, Enhanced Field Care, Prolonged Field Care, Progressive Resuscitation and Enhanced Diagnostics. The Operational Patient Care Pathway has been introduced to embed the medical lessons from the last decade of military operations into concepts and doctrine for the UK Defence Medical Services of the future.
Introduction
The last decade which has seen highly challenging military operations in Iraq and Afghanistan during which clinical care for combat trauma patients has been transformed. The UK Defence Medical Services (DMS) are now widely acknowledged to be international leaders in this field. Incremental improvements in the system of care have led to a significant number of unexpected survivors compared to the performance of civilian trauma systems (1). The Operational Patient Care Pathway set out in this paper provides a series of unifying concepts that articulate the clinical requirements for the UK military health services support (HSS (footnote 1)) system on operations. This includes clinical care for the ‘medical’ or ‘non-trauma patient’ as well as trauma care, and also covers to the specific challenges faced by the CBRN (Chemical Biological Radiological and Nuclear) threat. The Operational Patient Care Pathway has been published as DMS policy, however it will be reviewed prior to formal publication in the next version of UK medical doctrine.
The Operational Care Pathway builds upon a concept for ‘A Unified Emergency Care System (2)’ and maximises existing doctrine. It utilises imagery, mnemonics and other aids to learning that capture the key clinical and medical operational concepts to be taught to all members of the UK DMS. The UK will use the Operational Patient Care Pathway as the basis for discussion for developments in medical doctrine within NATO.
Context
The Operational Patient Care Pathway is set within the context of the holistic description of the whole DMS system contained within the Healthcare Cycle. The clinical outcomes required from the Operational Patient Care Pathway are described in the Chain of Care.
The Healthcare Cycle. The Healthcare Cycle is the ‘patient-centred’ provision of Health Services Support to the Defence Population at Risk (PAR) throughout their career by the Defence Medical Services. It is summarised at Figure 1. Defence medical operations and capability (DMOC) are those activities carried out by Medical Force Elements (Med FE) in order to provide HSS to the Defence PAR deployed on operations. Med FE are Force Generated (FGen) by the Service Commands (SCs) and are controlled by the Chief of Joint Operations (CJO) through the operational chain of command. The Surgeon General (SG) is the end to end Process Owner for the whole Healthcare Cycle and is responsible for assuring the quality of healthcare delivered to Service and other entitled personnel. The DMOC is shaded in purple. Prior to, and on deployment, the DMS supports the provision of Force Health Protection (FHP) measures to Service personnel from the Defence PAR. Service personnel who become operational patients are supported by the seven capabilities of operational healthcare (defined later) and, if necessary, are medically evacuated from the theatre of operations. Patients are accepted into the NHS under the Reception Arrangements for Military Patients (RAMP) and are usually admitted to the clinical unit of the Royal Centre for Defence Medicine (RCDM). Those that require specialist rehabilitation are transferred to the Defence Medical Rehabilitation Centre (DMRC); those requiring less specialised rehabilitation will be managed at regional rehabilitation units (RRUs) within the Defence Primary Healthcare (DPHC) organisation. Mental health support is provided by Departments of Community Mental Health. In all cases, after completion of care within the DMOC, Service personnel return to the Defence PAR under the purview of DMS Firm Base medical activities and capability; administration is undertaken by their own unit, or through Personnel Recovery Units or Centres (PRUs and PRCs) that form the Defence Recovery Capability (DRC). Firm Base clinical services are provided on a joint basis through Defence Primary Healthcare (DPHC), Defence Dental Services (DDS) and Defence Healthcare Commissioning.

The Chain of Care. The Chain of Care is the description of the clinical outcomes required from the Operational Patient Care Pathway. It is summarised at Figure 2. The Chain of Command and the DMS collectively contribute to the application of health protection measures to the Defence PAR as described in the Defence Health Strategy. If health protection fails, operational patients become sick or injured. First aid measures are essential to save life, limb and eyesight. The training of all personnel in essential first aid and a proportion of military personnel in extended first aid is the responsibility of the Chain of Command supported by technical training assistance from the DMS. The DMS trains clinical personnel to provide pre-hospital emergency care (PHEC) in order to take clinical responsibility from non-professional healthcare providers, and institute life-saving measures. Progressive Resuscitation extends these emergency measures from the pre-hospital environment to the capabilities of Deployed Hospital Care (DHC). As the patient stabilises, the clinical focus shifts to restoring physiological function through clinical care and medical evacuation. Once the patient is physiologically stable, care shifts to promoting healing through wound care, nutrition and psychological support. Finally, the patient leaves hospital care. The DMS and the Chain of Command support the patient in rehabilitation and return to physical, psychological and social function enabling them to return to duty or prepare for discharge from Service on medical grounds. The size of the ovals is indicative of the scale of organisational effort (including, but not solely, numbers of personnel involved, proportion of command effort, financial cost etc) required to provide the clinical outcomes at each stage in the chain of care.

The Operational Patient Care Pathway
The Operational Patient Care Pathway is a unified approach for clinical care to all operational patients arising from the Defence Population At Risk (PAR), exposed to the ‘all-hazards environment’, deployed on military operations. It encompasses the 7 Capabilities of Operational Healthcare and underpinning clinical concepts.
The Operational Patient. The term Operational Patient is an individual from the Defence PAR with physical, psychological or social ill-health who requires clinical care from the DMS on deployed operations encompassing battle casualties or disease and non-battle injuries (BC, DNBI). This definition has specifically been selected (vice Combat Casualty) to widen the focus from care of trauma patients to holistic care of all patients who require HSS on operations. The term Casualty is an Operational Patient prior to their admission to a medical treatment facility, thus the commonly used terms ‘Casualty Collection Point’, ‘Casualty Decontamination Area’ and ‘Casualty Clearing Station’ are retained.
The Defence Population at Risk (PAR) on Operations.
Eligibility for DMS medical support for a specific operation will be articulated in Medical Rules of Eligibility (MRoE) within operational orders. Members of all 3 Services are entitled to medical support, as are members of the Reserve forces, the Royal Fleet Auxiliary and civil servants deployed on operations. Captured personnel (CPERS) are also entitled. MOD contractors and nationals from NATO, the EU or other troop-contributing nations may be included, depending upon standing or other agreements. Eligibility for medical care for the wounded and sick is primarily derived from the provisions of the International Humanitarian Law. Therefore, the deployed medical contingent requires the capability to appropriately treat the UK military Population at Risk (PAR), non-UK military personnel and civilians (including children and the elderly). The DMS follows the general obligation to treat others; and for treating civilians in certain circumstances, abides by The Geneva Convention 1, Article 12. The healthcare needs of non-UK military and civilian populations may demand some capabilities which are not routinely available from the Regular component of the DMS. The DMS will have the organisational competence to manage medical support to the Defence PAR including access to competent medical personnel (Regular, Reserve, civilian or contracted), clinical equipment and clinical training.
The All-Hazards Environment. The All-Hazards Environment is the list of potential hazards to the Defence PAR summarised by the mnemonic CBRNE3T. The Defence PAR may be at risk from a range of potential Hazards on military operations. A confirmed Hazard is defined as a Threat for a specific operation (footnote 2). This expands on the CBRNE acronym widely used in the civilian world for major incident planning and emphasises the importance of Disease and Non-Battle Injury (DNBI) as the primary cause of health-related restrictions to human performance on operations. DMOC must be capable of supporting military operations whilst exposed to this All-Hazards Environment and be capable of providing clinical care to patients suffering from the consequences of exposure to one or more of these threats. The Force Health Protection estimate for a specific operation will determine the CBRNE3T threats to the Defence PAR defined in the MRoE. This will cover the impact of these threats across the 3 domains of health; physical, psychological and social. The CBRNE3T hazards are:
Chemical. This covers conventional chemical agent threats plus Toxic Industrial Chemicals, Riot Control Agents and chemical hazards derived from pharmaceuticals.
Biological. This covers live organisms, toxins and biological hazards deliberately employed to harm the Defence PAR.
Radiological. This covers material or events that release ionising (alpha, beta, gamma radiation and neutrons) and non-ionising radiation (including directed energy).
Nuclear. This covers weapons or events that result in nuclear fission/fusion reactions.
Explosive (and ballistic). This covers all consequences of explosive activity on human bodies including gunshot wounds, indirect fire, improvised explosive devices, shells and bombs.
Environmental. This covers environmental conditions likely to cause harm such as heat, cold, and altitude.
Endemic. This covers infectious diseases (Biological Agents of Operational Significance) that pose a hazard to the health of the Defence PAR that are not deliberately released.
Trauma. This covers the trauma element of non-battle injury threats to health in order to complement the Explosives (and ballistic) threats that also cause injury.
The Operational Patient Care Pathway
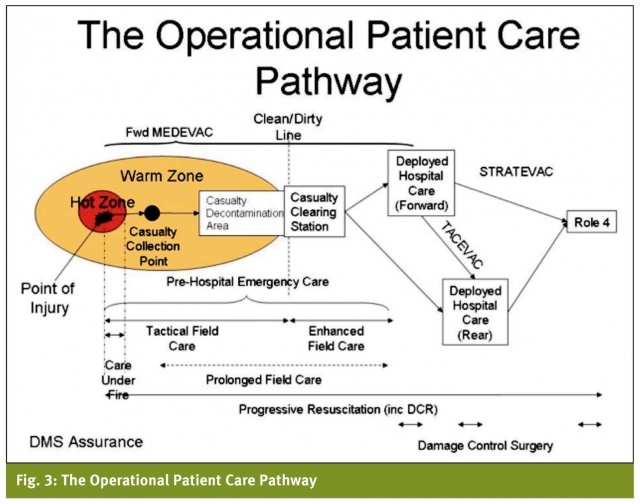
The Operational Patient Care Pathway combines concepts from incident management for trauma patients and CBRN patients, links these to the clinical capabilities described in the 7 Capabilities of Operational Healthcare and illustrates the continuous, seamless, escalatory increase in clinical care provided to the operational patient. It is summarised in Figure 3. There is a deliberate overlap in the boundaries between pre-hospital emergency care (PHEC) and progressive resuscitation in order to provide the maximum doctrinal freedom to medical operational planners in the specific employment of the clinical personnel and equipment in medical units. The key to successful delivery of the operational patient care pathway is the continuous and incremental provision of clinical care to meet the needs of the operational patient, independent of organisational boundaries.
The principles additionally apply to clinical support to the Defence PAR conducting training and other military activities but does not encompass additional clinical capabilities that are uniquely the purview of Firm Base health services support (even if delivered outside the United Kingdom, footnote 3).
There are two Zones of Care:
Hot ‘non-permissive’ Zone. The Hot Zone is a non-permissive environment representing an immediate threat to personnel from direct fire or a known environmental threat. Clinical care is limited to ‘Care Under Fire’ covering only those techniques necessary to provide immediate life-saving interventions whilst the patient is being extracted. This is likely to be provided as self administered or buddy-buddy first aid.
Warm ‘semi-permissive’ Zone. The Warm Zone is a semi-permissive environment representing a specific secondary threat to personnel from indirect fire or other CBRNE3T threat. There is not likely to be a demonstrable ‘hard edge’ to the Warm Zone. Clinical care is described as ‘Tactical Field Care’ covering those interventions necessary to save/stabilise life and prepare the patient for medical evacuation. The Casualty Collection Point is likely to be within the Warm Zone. Conceptually the ‘clean/dirty’ line for the handover of casualties from the Casualty Decontamination Area is the edge of the Warm Zone and the Casualty Clearing Station is outside the Warm Zone.
The area outside the ‘warm’ zone has explicitly NOT been labelled. There may be potential threats to the Health Services Support system but these are not sufficiently specific to extend the radius of the Warm Zone.
Care of the casualty starts at the Point of Injury (POI) in the Hot Zone. The casualty receives care under fire during extraction from the hot zone which extends to the remainder of the tactical field care capability. Casualties are amalgamated at the casualty collection point. After initial triage, casualties are transported to a casualty decontamination area where they are ‘sanitised’ to remove any threats to their health or that of their carers. If it is not possible to medically evacuate (MEDEVAC) them directly to deployed hospital care, casualties are transported to a casualty clearing station for enhanced field care pending MEDEVAC to deployed hospital care. Deployed hospital care (DHC) may be organised in echelons of care, illustrated schematically as ‘forward’ and ‘rear’. Prolonged Field Care is provided to casualties if there is likely to be a delay in meeting the 10-1-2 Medical Planning Guideline. The movement of operational patients between DHC facilities is TACEVAC and their movement from the Joint Operational Area to Role 4 in the Firm Base is STRATEVAC. The DMS Inspector General is responsible for DMS Assurance of the Operational Patient Care pathway under the direction of the Surgeon General.
10-1-2 Medical Planning Guideline. The 10-1-2 Medical Planning Guideline is the guideline for the location of clinical capabilities by time in the Operational Patient Care Pathway. It is the default for medical operational planning and any excursion from this guideline must be owned by the Operational Commander. The speed and quality of medical care can reduce the mortality and morbidity of operational patients. The ideal is always to deliver expert care as soon as possible after wounding. Evacuation should be to the most appropriate facility for the treatment of the casualty, noting that the most appropriate facility may not necessarily be the closest.
All time delays carry clinical risk for patients. It is for commanders, advised by their medical staff, to balance these risks with operational and other factors and to determine whether or not the risks are acceptable. To achieve this in practice, medical planning timelines guide decision-making regarding the configuration and location of the MEDEVAC and treatment assets needed to provide appropriate medical coverage to the supported force. Whilst primarily expressed as time for the trauma patient the principles apply to the non-trauma patient. The benchmark in civilian practice is rapid access within 8 minutes and hospital based surgery within one hour of injury. Evidence from accumulated experience in lraq, Afghanistan and earlier campaigns shows that there are three key timelines from Point of Injury (PoI) to first surgical intervention and a fourth for in-theatre specialist clinical care (specific terms are defined in the section on Deployed Hospital Care).
10 minutes – Enhanced first aid. Enhanced first aid is those immediate life saving measures that are applied by personnel trained in military first aid. Bleeding, airway control and administration of personal medical countermeasures for the most severely injured patients is to be achieved within 10 minutes of wounding (the so-called "platinum ten minutes"). For the UK setting, the 10 minutes is predominantly met by the use of Team Medic qualified personnel, although DMS medical personnel may be tactically located to support this requirement.
1 hour – Enhanced Field Care (EFC). EFC measures must be commenced by DMS medical personnel within 1 hour of wounding.
2 hours – Damage Control Surgery (DCS) and Critical Care Unit support. Patients that require surgery should be under treatment in a facility manned and equipped for DCS (noting the complexity of injuries on operations). Depending on the specific and individual requirements the aim is to be able to provide DCS within 1 hour, but no later than 2 hours of wounding. DCS should always be supported by Critical Care Unit support.
Further (Primary) Surgery and extended diagnostics should be available for the severely injured and may require deployment of in-theatre specialist capabilities if STRATEVAC timelines prevent this guideline being met.
The 7 capabilities of operational healthcare
The 7 Capabilities of Operational Healthcare are the essential capabilities required for HSS on operations. The DMS must be able to FGen MedFEs with these capabilities mission-tailored to the scale and complexity of a specific operation. Med FEs with these capabilities from environmental components will be integrated into a single HSS plan for the Joint Force. This may involve the use of multinational contributions to the HSS plan. The 7 Capabilities of Operational Healthcare are listed below:
Medical Command, Control, Communication, Computers and Information (Med C4I). Med C4I is the authority, processes, communications architecture and information management resources employed in managing the DMOC system.
Force Health Protection (FHP). FHP is defined as the conservation of the fighting potential of a force so that it is healthy, fully combat effective and can be applied at the decisive time and place. It consists of actions taken to counter the debilitating effects of environment, disease and selected special weapon systems through preventive measures for personnel, systems and operational formations. It considers force preparation measures, environmental health advice, in-theatre preventive measures, post-exposure measures and rehabilitation of the force. FHP must include competent medical advice in FHP for CBRN threats (in addition to the ’E3T’). FHP incorporates Medical Intelligence. Medical Intelligence is intelligence derived from medical, bio-scientific, epidemiological, environmental and other information related to human or animal health.
Pre-Hospital Emergency Care (PHEC). PHEC is the continuum of emergency care provided to a casualty (by individuals or teams) from first clinical intervention at point of injury through to reception of the operational patient at Deployed Hospital Care. The primary clinical output within PHEC is Progressive Resuscitation.
Progressive Resuscitation (incorporating Damage Control Resuscitation (DCR). Progressive Resuscitation (PR) is the use of multiple techniques drawn from technical and organisational advances in clinical care including administration of antitoxic therapies for the restoration of physiological function for the operational patient. It extends from point of injury until departure from the Critical Care Unit capability (including the Critical Care Air Support Team functions and CCU in Role 4). The Critical Care Unit is the specific area in a DHC facility designated for the continued provision of PR after initial treatment pending medical evacuation to the next level of care. PR incorporates DCR for care of the trauma patient. DCR is defined as ‘a systemic approach to major trauma combining the ABC (catastrophic bleeding, airway, breathing, circulation) paradigm with a series of clinical techniques from point of wounding to definitive treatment in order to minimise blood loss, maximise tissue oxygenation and optimise outcome.’
PHEC comprises 4 clinical phases and 2 clinical nodes of care.
Tactical Field Care (TFC). TFC is those interventions necessary to save/stabilise life and prepare the casualty for medical evacuation. It can be provided by any ’extended-trained’ individual (incorporating Team Medic or other authorised extended qualification plus all DMS clinical personnel). TFC incorporates Care under Fire: CUF is those techniques necessary to provide immediate life-saving interventions to the casualty in the Hot Zone while the patient is being extracted. The requirement for CUF is the basis of all first aid training taught to all members of the Armed Forces.
Enhanced Field Care (EFC). EFC is that emergency clinical care usually provided by a clinical team made possible by a more permissive environment using Battlefield Progressive Trauma Life Support (BATLS (3), CBRN-Emergency Medical Treatment and other progressive clinical techniques (as prescribed in JSP 999 CGOs).
Prolonged Field Care (PFC). PFC is those additional techniques that sustain the casualty if the 10-1-2 Medical Planning Guideline is likely to be exceeded (footnote 4).
Casualty Collection Point (CCP). The CCP is the first location where operational casualties from an incident are collected after evacuation from the Hot Zone at which TFC is undertaken. It is likely to be in the Warm Zone and manned by one or more designated DMS individuals. The Land environment equivalent is a Company Aid Post. The Maritime equivalent is the First Aid Post afloat.
Casualty Decontamination Area (CDA). The CDA is the location where contamination by threats (CBRNE3T) is removed from a casualty in order to remove any future threat to the health of the patient or the operational patient care system. This is NOT a clinical node of care and may be performed by non-medical personnel trained for this role, especially in a CBRN threat environment.
Casualty Clearing Station (CCS). The CCS is the location of a Med FE that delivers Emergency Team Care to operational patients, usually under the supervision of an independent practitioner. The environment specific FE is likely to be a Unit Aid Post (Army), Medical Reception Station (Army), Sick Bay or First Aid Post (RN), Role 1 (5) (RAF).
Primary Health Care (PHC). PHC is those general medical services, occupational health, dental services and intermediate care peripatetic services (e.g. mental health, rehabilitation, GU medicine) provided outside deployed hospital care that contribute to the maintenance of the health of the force. It is often delivered from Med FEs that provide the CCS function.
Deployed Hospital Care (DHC). Deployed hospital care is those clinical services provided by clinical personnel usually employed within hospitals. Access to DHC within the 10-1-2 Medical Planning Guideline is an essential component of the Operational Patient Care Pathway. Where time/distance precludes provision by a single DHC facility, DHC may be echeloned into DHC facilities illustrated as ‘Forward’ and ‘Rear’ facilities though an individual may be treated in more than two DHC facilities (footnote 5). DHC Forward facilities are likely to be mobile to enable the provision of Progressive Resuscitation and Damage Control Surgery within 2 hours. DHC Rear facilities are likely to be static and focussed on the provision of primary surgery and extended diagnostics. DHC covers the following specific clinical concepts:
Damage Control Surgery (DCS). DCS is a range of surgical interventions where completeness of the immediate surgical repair is sacrificed to achieve haemorrhage and contamination control, in order to avoid deterioration of the operational patient’s condition. It consists of emergency surgical procedures and treatment to stabilize casualties, in order to save life, limb or function, including rapid initial control of haemorrhage and contamination, temporary closure, and resuscitation. DCS techniques are applied when the magnitude of tissue and organ damage are such that surgery is likely to exceed the casualty's physiological limits. The concept is that only the minimum is done to deal with immediate life-threatening problems. Examples include: methods for rapid control of bleeding, control of enteric spillage without restoration of gut continuity, thoracotomy for penetrating lung injury, external stabilization of fractures, rapid amputation of a mangled limb in the presence of other equally serious injuries and temporary restoration of blood flow to a limb using vascular shunts. These procedures depend largely on the ability to provide progressive resuscitation and are therefore an inter-disciplinary effort rather than solely a surgical challenge. They call for proper pre-operative planning as well as good peri-operative coordination between the various involved specialists. DCS should be followed later on by primary surgery, which is delayed until the various physiological and other relevant parameters have been restored to as close to normal as possible. It can only occur within a DHC unit. This usually requires a combination of general and orthopaedic surgery and should include burns & plastic surgery wherever possible.
Primary Surgery. Primary surgery is the range of surgical procedures directed at repair of local damage caused by wounding, rather than correcting the generalised effects of trauma. Whenever the operational circumstances and the patient’s condition permits, it should be performed ideally within the first hour of trauma management and certainly within 4 hours, as the delay to the initiation of primary surgery may allow further generalised effects to develop that may lead to an increase in mortality, morbidity and residual disability. The provision of primary surgery may require the deployment of surgical sub-specialist teams including ophthalmology, neurosurgery, head and neck surgery or maxillo-facial surgery.
Extended diagnostics. Extended diagnostics are those clinical support activities (e.g. CT scan if not available as part of DCS, interventional radiology, and specialist laboratory support including biochemistry, haematology and microbiology testing) that enable clinical therapies to address the specific cause of injury or illness that are additional to generic stabilising therapies.
PAR specific/condition specific clinical capabilities (footnote 6). PAR specific/condition specific clinical capabilities are those clinical and clinical support capabilities within the Operational Patient Care Pathway that are mission-tailored for each specific operation dependant on the CBRNE3T threat and the MRoE. DHC will need to care for the full Defence PAR and for the specific clinical conditions arising from the threats determined by the FHP estimate. It may be necessary to deploy additional clinical specialists to manage PAR specific/condition specific cases including CBRN medicine, tropical medicine, paediatrics or maternal health specialists.
Medical Evacuation (MEDEVAC). MEDEVAC is the movement of operational patients under medical supervision in a designated transport platform equipped for role. MEDEVAC is controlled by a Patient Evacuation Co-ordination Cell (PECC) that operates under the authority of the battlespace owner to ensure that MEDEVAC platforms conform to the tactical environment. The PECC is responsible for ensuring the right patient is collected from the right pick-up point, transported to the right destination in the right platform, with the right medical escort in the right time. There are 3 categories of MEDEVAC.
Forward MEDEVAC which is the movement of casualties from point of injury to deployed hospital care (including to/from the CCS).
Tactical MEDEVAC (TACEVAC) which is the intra-theatre movement of patients between deployed hospital care facilities.
Strategic MEDEVAC which is the movement of patients from the theatre of operations (usually to Role 4).
Medical Logistics (MedLog). MedLog is the process of procurement, storage, movement, distribution, maintenance and disposition of medical material and pharmaceuticals, including blood, blood components and medical gases, in order to provide effective medical support and the application of this process in planning and implementation.
Conclusion
The Operational Patient Care Pathway described in this paper is designed to provide a series of unifying concepts that articulate the clinical requirements for the UK military health services support system on operations. It captures the key concepts developed over the past decade of military operations and provides the framework upon which to develop future military medical capabilities.
Date: 01/22/2014
Source: MCIF 1/14











