

Article: T.J. Ligthelm, L.A. Wallis, S. Martin, P.J. Van Aswegen (South Africa)
Mass Casualty Aero-Medical Evacuation: From the Nigerian Building Collapse back to South Africa
The article discusses the use of military aircraft for a mass casualty aero-medical evacuation of civilian casualties over a long distance. Structured approaches of a pre-determined team with pre-planned equipment are explained. The positioning of patients in the plane is planned according to a loading plan with specific triage priorities placed at specific levels. The lessons learned during the evacuation of 25 civilian patients after the Nigerian building collapse over a distance of 4500 km back to South Africa are highlighted.
Introduction
During September 2014 at least four organised groups totalling more than 100 people, travelled from South Africa to attend services at the Synagogue Church of All Nations (SCOAN) under the charismatic leadership of its pastor, T.B. Joshua, in Lagos, Nigeria.
On Friday, 12 September 2014 at approximately 12:44 local time (1)a guesthouse on the premises of this church collapsed, injuring an undeclared number of casualties and killing 115. Amongst the injured were a large number of South Africans. Casualties were evacuated from the site in an uncontrolled operation to an unknown number of hospitals in Lagos. No accurate name list was maintained by the church and no central information system was created by the Nigerian authorities.
Lagos, with an estimated population of 21 million (2)is served by approximately 54 hospitals (3) (4).
The initial information received was that there was a possibility of three South Africans injured in the event. This picture slowly started to evolve and by 15 September, it was clear that a substantial number of South African citizens were either killed or injured in the event. No information, however, was available on the condition of the injured or the care they had received or required.
As more information became available, the South African Government by 16 September, appointed an Inter-Ministerial Committee to manage the event under the chairpersonship of the Minister in the Presidency and activated its joint planning structure. This structure consisting of all applicable government departments, the South African National Defence Force and the South African Police Service, is a well-established coordinating capability and was tasked to manage the response. Within this coordinating structure, a health cluster was formed of the National Department of Health and the Military Health Service.
Response
This Health Cluster adopted the classic command algorithm of CSCATTT approach (5) (6) to address the medical needs of the situation, namely:
- C: Command.
- S: Safety.
- C: Communication.
- A: Assessment
- T: Triage
- T: Treatment
- T: Transport
Command
A joint co-command was established, consisting of military and civilian personnel, working together as a team. This included a command element from the South African Military Health Service and a co-commander from the National Department of Health. This grouping immediately started compiling a mass evacuation plan for possibly transporting a large grouping of casualties back to South Africa.
Safety
Both the intelligence community and the Police Service assessed the safety of victims as well as possible relief teams, in view of the political and security turmoil in Nigeria. This included an assessment of the possibility of terror threats from the Boko Haram grouping in Nigeria. It was concluded that the situation in the Lagos region is stable and that a relief operation could be launched.
Simultaneously, the health cluster assessed the health risks for such an operation. A case of Ebola Virus Disease was introduced into Nigeria on 20 July 2014 when an infected Liberian man arrived by aeroplane into Lagos. The man, who died in hospital 5 days later, set off a chain of transmission which infected a total of 19 people, of whom 7 died (7). Nigeria was only declared Ebola-free on 20 October 2014 (8).Numerous allegations and non-substantiated statements were made at the time that pastor Joshua had claimed to be able to cure Ebola and was able to “wash off Ebola” from people exposed to the disease. As the grouping in the building at the time of the collapse were unknown, it was possible that Ebola patients from Sierra Leone, Guinea or Liberia, where the Ebola outbreak occurred or from Nigeria itself, may have taken a pilgrimage to the church for healing. As the outbreak in Lagos was also not yet under control, the risk was that casualties may also have been exposed to Ebola in the hospitals in Lagos after the event. These allegations, which could be neither substantiated nor proven false, held the risk that some of the casualties may have been exposed to Ebola Virus Disease.
As many patients with other serious health conditions were on a pilgrimage to the church to seek healing, the risk for other communicable diseases such as extreme drug resistant tuberculosis, needed to be considered. As no information was available on the health conditions of the South Africans who travelled to the church, or the infection control measures in the hospitals they were admitted to, communicable diseases were identified as a serious health safety risk and the need for precautionary measures planning was identified.
Communication
To enable proper planning; communication was established with frequent combined planning meetings. These meetings included a health cluster meeting, followed by a meeting of the joint planning structure with role-players from all the government departments and agencies involved. The first planning meeting took place on 16 September 2014 at 15:00. In the initial stages of the response these meetings occurred three times per day. 14 meetings were held over a period of 10 days prior to the operation.
The South African Consul General in Lagos was activated and a communication link between the Consulate and the joint planning group was established. After the assessment team arrived in Lagos, an Operational Room was established in a hotel in Lagos with telephone communication lines back to South Africa.
Within South Africa, a communication centre with a 24-hour telephone line was established at the Department of International Affairs and Cooperation (DIRCO) where family members could enquire about their next-of-kin. This was later expanded to a social service response line.
Assessment
As information was very limited on the number and condition of casualties it was decided to deploy an assessment team to Lagos to join-up with the South African High Commissioner’s staff, in order to execute an accurate evaluation of the impact of the event. It was clear from the onset that the medical condition of the injured will need to be assessed specifically to determine possible requirements and to determine the need for evacuation of the injured back to South Africa.
On Thursday, 18 September 2014, Prof Lee Wallis, Head of Emergency Medicine at the Universities of Cape Town and Stellenbosch, was deployed by commercial airline to Lagos to assess the medical condition of the injured and to advice on evacuation. He arrived in Lagos on Friday19 September 2014and joined-up with the rest of the assessment team consisting of various government departments and the SA Police Service.
As it was unclear at that stage how many South Africans were injured or where they were treated, he had to work systematically through all applicable hospitals in Lagos tracing possible South African patients.
By Saturday morning 20 September 2014, Prof Wallis gave the feedback that he had identified 26 South African patients from the incident in 5 hospitals.
Additionally one uninjured orphaned child would need to be evacuated along with an injured sibling and a spouse who needs to travel with a patient.
It was clear from the assessment that the patients were seriously injured, some with serious co-morbid health problems, which required urgent medical interventions. The best-practice interventions required were not necessarily readily available within Nigeria.
Based on the feedback from the assessment team, the South African Government opted to evacuate the injured back to South Africa through a mass aero-medical evacuation. Various options were appreciated and the most feasible option was identified to utilise a rigged C-130 aircraft from the South African Air Force and staffed with a Mass-Casualty Aero-Medical Evacuation Team from the South African Military Health Service (SAMHS).
Triage
The assessment team assessed each patient clinically and a triage priority was allocated utilizing the military Priority 1, 2 and 3 approach. This information was captured in a database and each patient allocated a patient number. This database with basic clinical information was sent back to South Africa where the Health Cluster received the first accurate data on 20 September 2014 at 00:34B–8 days after the incident. These patients were listed and evaluated as:
- Priority 1: 6
- Priority 2: 16
- Priority 3: 4
Based on the triage categories and clinical information a mass casualty aero-medical evacuation team was then placed on a six-hour stand-by, whilst the planning for over-flight clearances for a military aeroplane over at least three countries, was conducted by the South African Air Force and DIRCO.
The assessment team also evaluated each patient for the possibility of exposure to Ebola Virus Disease as well as co-morbid conditions, which may influence air-evacuation. The assessment team warned that Ebola precaution measures were only in place in one of the hospitals visited. Although all patients were within the 21-day incubation period for Ebola, since their arrival in Nigeria, none of them had any increased temperature. This risk was continuously assessed by a specialist advisory team from the National Centre for Communicable Diseases (NICD) in South Africa. As none of the patients met the case definition for Ebola, the decision was taken to only take adequate personal protective equipment along, but not to transport any patient in an isolator (three negative pressure transport isolators were brought into readiness as a contingency).The co-morbid communicable diseases were also assessed and the assessment team found that none of the patients had a known high-risk communicable disease.
The triage assessment was therefore limited only to clinical injuries and co-morbid non-communicable diseases.
| Case No | Gen-der | Primary Injury | Comments | Other Concerns | Prio-rity* |
| 1 | F | Left Below Knee Amputation | Healthy wound; mobilising slowly | None | 2 |
| 2 | F | Left Above Knee Amputation | IV antibiotics; ready to mobilise | Left arm soft tissue injury | 2 |
| 3 | M | Right Below Knee Amputation | IV antibiotics; ready to mobilise | Urine catheter | 2 |
| 4 | F | Right pneumothorax; ICD in situ | IV antibiotics | | 2 |
| 5 | F | Right upper arm wound | Infected wound; IV antibiotics | Non-Insulin Diabetes | 2 |
| 6 | F | Le Fort III fracture | Moderate facial swelling; taking oral fluids; mouth laceration sutured; ready for surgery; IV antibiotics | 3 units blood transfused; HCT 33% | 1 |
| 7 | F | Pelvic injury – no fracture | Ready for discharge | Soft tissues injuries | 3 |
| 8 | F | Left orbital blow out fracture | IV antibiotics | Left hand injury – soft tissue | 2 |
| 9 | F | Right pelvic injury (? Fracture?) | Hematemesis Thursday two episodes; rib fractures suspected but no pneumothorax; IV antibiotics | Right knee ligament injury for PoP backslab; catheterised | 1 |
| 10 | M | Right bi-malleolar ankle fracture with talar shift | Below knee PoP backslab; apparently minor abrasion over fracture; IV antibiotics | Hypertensive on medication | 2 |
| 11 | M | Crush injury | Acute kidney injury on haemodialysis; needs dialysis Sunday morning | Spinal injury neurological fall out both legs; catheterised; right shoulder fracture | 1 |
| 12 | F | Soft tissue injuries both legs | IV antibiotics; Enoxaparin | Hypertensive on medication | 2 |
| 13 | F | Soft tissue injuries | Recovered | | |
| 14 | F | Chest wall injury | Rod through right breast exit right back; IV antibiotics; infected wounds | Insulin dependent; Hypertensive on medication | 1 |
| 15 | F | Right bi-malleolar ankle fracture | Below knee PoP backslab; needs surgery | | 2 |
| 16 | F | Left arm injury | Elevation for swelling | Parotic laceration – missed injury; closing by secondary intention; honey dressing. | 2 |
| 17 | F | Back injury no fracture or neurology | Ready for mobilisation | Non-Insulin Diabetes | 2 |
| 18 | F | Fracture right tibia | Above knee PoP backslab; IV antibiotics; Enoxaparin | Deteriorated later in day; confused; febrile. | 1 |
| 19 | F | Leg and back pain | No fractures or neurology; mobilising | | 3 |
| 20 | F | Back pain | No fractures or neurology; bed rest; catheterised; Enoxaparin | | 2 |
| 21 | F | Back pain | No fractures or neurology; bed rest; Enoxaparin | | 2 |
| 22 | F | Left medical malleolus fracture | Below knee PoP backslab; Enoxaparin; being mobilised | Pelvic pain no fracture | 2 |
| 23 | F | Leg and back pain | No fractures or neurology; bed rest; Enoxaparin | | 2 |
| 24 | F | Right scaphoid fracture | PoP front slab; may convert to split full PoP; IV antibiotics for hand wounds | Hypertensive on medication | 2 |
| 25 | F | Left arm and both legs injury | Soft tissues; lacerations | Hypertensive on medication | 3 |
| 26 | M | Gangrene left 4 toes | Spreading infection; dry dressings; IV antibiotics; needs amputation | Multiple abrasions and bruises | 1 |
Table 1: Patient List | * Priority for aero-medical evacuation
Treatment
In preparation for the aero-medical evacuation, limited treatment was initiated in Lagos by the assessment team. This was limited to treatment advice to the local clinicians, as the assessment team was not registered for practice in the country. This situation necessitated the aero-medical evacuation team to prepare to initiate treatment at the airport prior to evacuation.
Due to the nature of the injuries, especially the serious orthopaedic injuries, a military orthopaedic surgeon was included in the team to initiate treatment. Additionally the hospitalisation needs were assessed and communicated to South Africa in order to enable the receiving hospital to adequately prepare.
The Aero-Medical team was informed of the need to establish a temporary Resuscitation Post at the airport in Lagos to stabilise patients for evacuation.
Transport
An evacuation plan was compiled and the team was briefed on the plan.
Doctrinal Approach
A mass casualty aero-medical evacuation was planned according to the military health service doctrine (9). Theoretically, a Hercules C-130 can carry 72 stretchers but in this full-configuration, extremely limited movement space is available with limited seating for crew and little space for equipment. Due to these limitations, the SAMHS utilises only the central rigging of stretchers and not the stretcher positions on the outer sides of the plane. This space is reserved for team members and equipment. The aft stretcher rigging positions are also not used to allow space for high-care platforms.
According to the SAMHS doctrine the rigged C-130 is divided in port and starboard sides. Each side is structured in columns identified by alphabetical letters from the front and then rows identified by numerical numbers from top to bottom. Staff is allocated according to this layout with:
- an emergency care practitioner per row of maximum five stretchers,
- a nursing officer is then allocated for every two rows; and
- a medical officer per side of the plane.
A Priority 1+ area is established in the back of the plane with up-to four high care platforms. Each high-care platform is allocated a nursing officer and a medical officer is allocated per two high-care platforms.
Each side of the plane is also staffed with a warrant officer who co-ordinates and controls loading and off-loading as well as a technical officer who maintains oxygen supply and electronic equipment.
An overall Military Health commander is appointed for the plane with a warrant officer to support him/her. The commander is specifically not a clinician to ensure that command and control is maintained without being sidetracked by clinical needs of patients in evacuation.
In total, a Mass Casualty Aero-Medical Evacuation Team consists of 23 members (9).
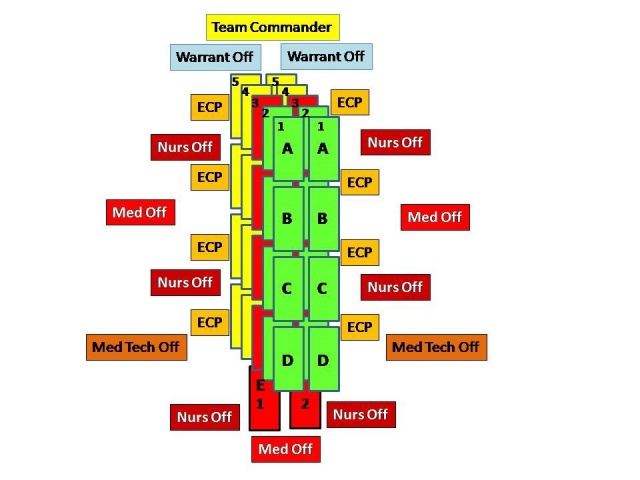 Fig. 1: Outlay and Staffing Aeroplane
Fig. 1: Outlay and Staffing Aeroplane
This team is supported by a minimum of two loadmasters from the Air Force.
This doctrine was practiced and tested by the SAMHS 2 months prior to the event, which enabled the team to apply the doctrine, and the lessons learned during this operation.
Aero-Medical Evacuation Team
Although the triage assessment only indicated 26 patients for evacuation, the risk existed that more patients may be found in the chaos following the incident or that neighbouring countries may have found some of their citizens and requests South Africa to evacuate these citizens back to Southern Africa as well. For this reason the decision was made to prepare the plane for the full load of 40 stretchers in the rigging and 2 high-care platforms.
The team was therefore constituted to address the full planeload of patients and not necessarily only the patients on the triage list.
The Mass Casualty Aero Medical Evacuation Team mobilised for this operation was adapted to reflect the expected patient’s profile. Only one technical officer was available. The team for this operation consisted of:
- Commander
- 5 X Medical Officers (Including Orthopaedic Surgeon)
- 6 X Nursing officers
- 8 X Emergency Care Practitioners
- 1 X Technical Support Officers
- 2 X Warrant Officers
Initially a Paediatrician was also included but after reviewing the information of the injured child it was found not necessary.
The team reported to the Air Force base on 21 September 2014 at 02:00B ready for deployment. The plane took-off at 03:56B– 9 days after the event.
Food parcels were provided for the team for three meals in flight and adequate drinking water was made available.
Equipment
The doctrinal approach for equipment was adhered to (9). In this approach standard resuscitation equipment, monitors, suction and oxygen are packed per column of five stretchers. Additional support equipment to replenish this first line of equipment is added per side of the plane. These include mass infusion packs with additional fluid as well as drugs.
Each high-care platform carries its own oxygen, suction and resuscitation equipment. Four high-care platforms were available, but based on the assessment teams’ findings only two were loaded.
A central emergency blood bank with fresh frozen plasma and packed cells in portable refrigerators was taken along. No platelets were taken along due to a logistical challenge.
Comfort equipment such as bedpans, urinal-bags and a chemical toilet was also packed per side of the plane. Due to the nature of the injuries, six scoop stretchers were included to transfer patients from ambulance stretchers to the aeroplane stretchers and four vacuum mattresses were taken for spinal injuries.
Standard NATO-design canvas stretchers were used throughout the plane for all the columns. These stretchers were equipped with a linen pack with pillow, sheets and a blanket. An aluminium space blanket was used underneath the patient for isolation and additional blankets were available to keep patients warm. (The patient compartment of the C-130 plane’s temperature can be adjusted to ensure patient and staff comfort. This system however often overheat the forward part of the cabin, to ensure a comfortable temperature in the aft.) It was decided that due for the duration of the flight, all patients and the uninjured child will be transported as stretcher cases, as adequate space was available.
Two small orphaned children, aged 2 and 6 were amongst the patients. A donation of a teddy bear and a gift pack per child was received from a private hospital group prior to the flight and taken along. A nursing officer was appointed to take care of these children in-flight.
To adhere to custom regulations, all equipment had to be declared to the custom authorities prior to the operation. This was a very time consuming process.
Road Transport Plan and Pre-Flight
Treatment in Lagos
The Assessment Team compiled a meticulous transport plan to transport all the patients from the 5 hospitals to the airport, based on clinical condition. All hospitals were within an 8 km radius from the airport. Each patient was allocated a number and these numbers were attached by identification bracelet to the patient. The very limited number of six ambulances (3 from the church, 2 private and one hospital ambulance) and one minibus were planned optimally to move the less serious patients to the aircraft first and then return to transport the more serious patients last. The purpose of this plan was to limit the out-of-hospital time of the critical patients to the minimum.
On confirmation of the landing time of the plane in Lagos this plan was activated. One patient decided not to return on the flight and to return to the church, resulting in 25 patients and 2 uninjured passengers evacuated.
The C-130 landed on 21 September 2015 at 14:43B on the military apron of the Lagos International Airport. An aircraft hangar space was made available to the team by the Nigerian Air Force to establish a re-triage and resuscitation post. On arrival the team commenced with the final rigging of the plane and preparing all stretchers for receiving patients. All equipment was moved to in-flight positions and checked. The resuscitation area was prepared to receive patients.
 Fig 2: Preparation Patients for Evacuation
Fig 2: Preparation Patients for Evacuation
Within 2 hours after landing, the patients started arriving. Patients were transferred from the ambulances to the pre-determined triage and resuscitation area. Prof Wallis re-triaged the patients and briefed the clinicians on the patient’s condition.
In the triage area, the patients were assessed for:
- Severity of injuries.
- Type of transport support required such as vacuum mattresses or standard stretchers.
- Requirements for pre-flight treatment.
During the assessment patients who had spinal injuries were placed on vacuum mattresses to assist with in-flight stabilisation, comfort and safety during loading; four (4) patients were immobilised on vacuum mattresses.
Numerous patients also required anti-emetics and analgesics pre-flight. Where applicable intravenous lines were established and the administration of blood products commenced. All chest drains were connected to one-way valves for the flight.
Two seriously ill patients required special pre-flight treatment. The first patient had an iron rod piercing her thorax with an accompanying haemo-pneumothorax. She had no intercostal drain in situ and this had to be inserted before flight in the back of an ambulance by torch light.
The second severely ill and unstable patient had a Glasgow Coma Score of 6/15 (E1V1M4) and required endotracheal intubation. The patient had a pre-morbid mass lesion in the pharynx and thus presented with an extremely difficult airway to manage. This patient was intubated and placed on a high-care platform, which allowed intensive care quality monitoring and support.
The patient with the Le Forte III fracture was placed on the second high-care platform as this allowed the patient to be positioned in Fowlers position during the flight.
 Fig 3: High-Care Platforms positioned in the aft of the aircraft
Fig 3: High-Care Platforms positioned in the aft of the aircraft
All patients were re-assessed for increased temperature as result of the Ebola risk, but no patient had any signs.
The warrant officers commenced with compiling the loading plan for the plane, utilising patient numbers against stretcher positions. A system of colour-coded rows per column of stretchers was utilised.
Loading Plan
The most critical (often ventilated patients) are identified as Priority 1+ to be loaded on the high-care platforms. Two of these platforms were available and patients were identified for these positions.
Each column of patients are then planned, with planning the priority 1 patient at eye level for a sitting attendant, a priority 2 patient below and the priority 3 patients above. This allowed easy access to the priority 1 and 2 patient in flight, while the priority 3 patients who required less care in flight were in the less-assessable positions. Due to the limited number of patients (no additional patients were identified), only four stretchers per column were used for this flight.
The Warrant Officers were guided by the clinicians, compiling a loading plan by allocating specific patient numbers to each stretcher position. As soon as the complete loading plan was available, loading started per side of the plane, from the front to the back. The team, supported by the Nigerian Air Force staff, were grouped into stretcher parties and the stretchers carried on-board. (Attempts in the past to use wheeled base stretcher-carriers have proven not effective and manual stretcher parties remain the most effective method for loading). The Warrant Officer and a loadmaster checked and had to confirm that each stretcher was properly secured.
 Fig 4: Limited space available within the aircraft
Fig 4: Limited space available within the aircraft
Due to limited space within a fully rigged C-130 our experience is that it is very difficult to manoeuvre stretchers past already loaded stretchers, therefore each column is fully loaded before the next column is started. The high-care platforms are moved into position lastly and the critical patients brought on-board last. Loading a mass casualty evacuation aircraft is a labour intensive operation, which requires muscle strength from all members to carry and lift stretchers into position.
Due to bureaucratic challenges within Nigeria the assessment team advised the plane to take-off as soon as possible, putting severe strain on the crew-duty time of the air crew.
The average time to load a C-130 during exercises was130 minutes (5, 7 min per patient/side). In Nigeria due to the condition of the patients and the need for stabilisation intervention, this process took 245 minutes (19, 6 minutes per patient/side).
By 22:30B all patients were loaded, the high-care platforms positioned and the two critical patients loaded. On 22 September at 00:05B the plane departed from Lagos International Airport.
In-Flight Care
The in-flight evacuation was fairly uneventful due to pre-flight intervention. One patient was ventilated in-flight utilising a transport volume-cycled ventilator with a FiO2 of 100% and a PEEP of 5-10 to maintain saturation. Saturation was effectively achieved throughout the flight. The other patients maintained saturation > 90% on cabin air and did not require any additional oxygen administration. Oxygen was however available at every column of stretchers.
It was possible to mount intravenous infusions to the stretcher position above utilising basic S-hooks. Very limited turbulence was experienced in-flight and no challenges were experienced with this mounting method.
A fuel stop was done at Kinshasa Airport taking 45 minutes, allowing staff to do a full re-assessment round of all patients. The fuel stop also allowed staff to use restroom facilities.
Except for basic contact precautions protective equipment, no special personal protective equipment was used during the evacuation.
Each child received a soft toy to comfort them in-flight and a specific nursing officer cared for the children in flight.
Lighting in the passenger compartment of the plane is limited and headlights were used by all staff members.
Clinical observations were measured and recorded throughout the flight. Due to the time spent preparing patients followed by the 10-hour in-flight care, the clinical team was exhausted. A rotation system with 2-hour shifts was implemented to allow the staff a rest break. This assisted with ensuring quality patient care.
No patient passed-away or seriously deteriorated during evacuation.
Arrival and Off-Loading Plan
An off-loading plan was compiled for arrival at the Air Force Base in South Africa.
A Receiving Commander was appointed and a group of 30 stretcher-bearers was mobilised to be in position on arrival at the Air Force Base.
Thirty civilian and military ambulances were mobilised to be in position on landing. Ambulances were grouped based on available staff and equipment into Priority 1 ambulances and priority 2 and 3 ambulances. Each ambulance carried its own crew, which was independent of the stretcher-bearer parties. This allowed for off-loading to continue without delaying ambulance evacuation.
The plane landed on 22 September at 10:43 in Pretoria. On arrival of the plane, Port Heath procedures for mosquitoes and custom procedures were adhered to. Due to another activity, a secondary air force base in Pretoria had to be used. This base had to be officially declared a temporary Port of Entry for custom procedures. All equipment had to be re-checked by customs authorities and all foodstuffs left over, had to be collected as it may not be brought back into the country. A massive media presence was experienced and a specific media area was earmarked in advance.
The off-loading plan was then activated. A road-cone corridor was marked out around the plane and pickets positioned to prevent any ambulance from coming too close to the plane and to ensure a one-way circle route from parking to exit. (Antennas from ambulances had damaged planes in the past during loading and off-loading of patients).
In coordination with the Aero-Medical Team commander, the Receiving Commander called ambulances forward, based on the re-triage priority of the patients. The high-care platform’s patients were off-loaded first and dispatched to the receiving hospital. This was followed by a structured off-loading process simultaneously on both sides of the plane. Ambulances were called forward, the patient off-loaded by the bearers and the in-flight staff handed the care and clinical notes over to the ambulance crew. As far as possible, only one patient, with their personal luggage, was loaded per ambulance. As the ambulances were loaded, they formed up in a convoy and were escorted by traffic police to the receiving hospital.
 Fig 5: Off-loading drills with bearer-parties
Fig 5: Off-loading drills with bearer-parties
The orthopaedic surgeon was transported to the receiving hospital immediately after arrival to brief clinical staff on the condition of the patients. Special arrangements were made for the orphaned children on arrival. A specific team accompanied them to the hospital where a social worker was waiting to receive them.
A separate fatigue team with a truck was provided to offload all the equipment, while a team was also pre-positioned at the receiving hospital to collect all stretchers and equipment as patients were off loaded onto hospital gurneys.
A large group of government dignitaries were accommodated to welcome the patients back to South Africa. These dignitaries were only allowed access to the plane by the Receiving Commander after the critical patients were off-loaded and dispatched to the hospital.
A massive amount of personal luggage of the patients was delivered by the Nigerian authorities to the airport. This provided a serious challenge with space, but it was loaded on the loading ramp of the plane and therefore had to be off-loaded first on arrival before any patient could be off-loaded.
Hospitalisation Plan
Due to the high publicity of the event, as well as condition of the patients, a decision was taken to transfer and admit all patients initially to the Steve Biko Academic Hospital in Pretoria, 12 km from the Air Force Base. This decision allowed for easy record keeping, full re-assessment of all patients, availability of high-technology capabilities for critical patients, proper debriefing of all victims and a coordinated reception by government at a single facility. The management and clinical staff of the hospital were briefed prior to the operation, to ensure the hospital was ready to receive patients.
A re-uniting process with social work support for next-of-kin was planned at the receiving hospital. No next-of-kin were allowed at the air force base and all re-uniting occurred in controlled circumstances out of public view, at the receiving hospital.
Within 120 minutes after landing of the plane all patients were admitted to the receiving hospital.
From take-off to admission to hospital, the entire operation was executed in 12 hours.
Lessons Learnt
Pre-planning a mass casualty aero-medical evacuation and practicing the process, with pre-packed equipment, is of critical importance for the successful execution of such an operation. The sub-division of the plane into zones with staff and equipment allocated per zone not only enhances control but ensures that patient care is structured during flight. The team must be drilled in the procedure and be in possession of the required travel documents and vaccination records.
Proper triage and assessment (if possible prior to dispatching the team) is essential to ensure that optimum care and equipment is available on-board the flight. In a large mass casualty evacuation, an assessment team must be dispatched in advance to evaluate, triage and prepare patients for evacuation. Stabilisation prior to evacuation remains the cornerstone of successful aero-medical evacuation.
The proper loading plan, based on triage categories and utilising column and row numbers is of the utmost importance for mass evacuation.
The loading and off-loading of a mass casualty evacuation plane is a labour intensive operation, which requires effective control and a large number of staff, physically able to lift and load stretchers.
Evacuating patients over such a long distance requires the use of additional staff to allow rest/sleep as the team in this event were totally exhausted on arrival. Additional staff must be planned for loading and off-loading.
The use of military transport planes remains a solution to evacuate large numbers of lying patients in a mass casualty event. The number of stretchers loaded must however be balanced with space to accommodate a proper number of clinical staff and support staff and allow for access to all patients. Our experience is that a C-130 can optimally only accommodate 40 rigged stretchers and two high-care platforms or 50 rigged stretchers.
Mass casualty evacuation entails a large volume of equipment. Separate vehicles must be planned with a team to load and off-load this equipment. Placing a separate vehicle with staff at the hospitals to collect all equipment ensured that no equipment was lost in this operation.
Planning to accommodate the personal luggage of patients must be included in the plan. Space must be planned for and a vehicle and team to handle luggage proved essential.
Small children require special planning for evacuation, especially if they have minor injuries and are aware of their surroundings. The availability of soft toys, such as a teddy bear, comforts them in flight. Special precautions need to be taken with orphaned children to ensure proper management and care.
An information system for next of kin with a re-uniting plan with social work support is an integral part of a mass casualty evacuation plan.
Conclusion
Military medical air transport assets and teams can be utilised effectively in civilian mass casualty incidents, to evacuate large numbers of patients, over long distances, on condition proper assessment and planning is done. The CSCATTT concepts itself serves as a guide to plan such an operation.
Mass Casualty evacuation is a time consuming operation. This is not a hot-extraction capability, as it required a secured airhead with time and human resources to assemble, prepare and load patients in a structured approach.
Bibliography
Date: 07/14/2015
Source: MCIF 3/15











