Article: A.-J. SCHRIJER (THE NETHERLANDS)
Planning the Impossible
LESSONS LEARNED – AFGHANISTAN
Within the medical community, the medical chain management is a topic that is not well known. Care protocols, patient treatment procedures, research and development techniques and break-troughs are more commonly shared within our community. However, the deployment of a medical chain to allow a force of a certain size to conduct operations in a less-friendly environment requires a specialized medical skill set.
Introduction What is needed, which level of care quality do we need to bring to the theatre, how many and what type of assets are required, are there national regulations that play a part? All these and many more questions have to be answered before an operation can be conducted with proper medical coverage. This article is meant to give the reader an insight in the world of the Medical Planner. In the upcoming chapters, I’ll highlight the theory behind medical planning and use NATO’s RESOLUTE SUPPORT mission in the Northern part of Afghanistan to show the theory at work. It includes a real occurred example how to adept the standing medical coverage into a specific unexpected situation. I will end this article with a number of conclusions.
1. The Theory
1.1. Opening
Medical chain management. The terminology is clear enough: managing the medical chain. Chain management in a multi-national environment of a NATO mission is above all a challenging business. The medical elements that are part of the medical chain are diverse in nationality, feasibility and usability. To combine the elements, forge them into a chain and execute successfully Command and Control over it, NATO uses a handful of documents that give guidance and direction to the forging process. AJP 4.10(b) being the basis of it all.
1.2. Introduction
Medical support is present to support the mission, wherever it is conducted. The medical
chain needs to be designed in such a way that patients that occur during these missions are treated by the appropriate medical quality level within the mandatory timeframe. Medical care, when deployed properly, enables a force to conduct operations with greater risks and still have a good survivability when the operation goes wrong. Chain management therefore has a great impact on the planning and execution of an operation. Flexibility of medical assets and the potential client is mandatory to execute medical chain management successfully.
1.3. The Theory
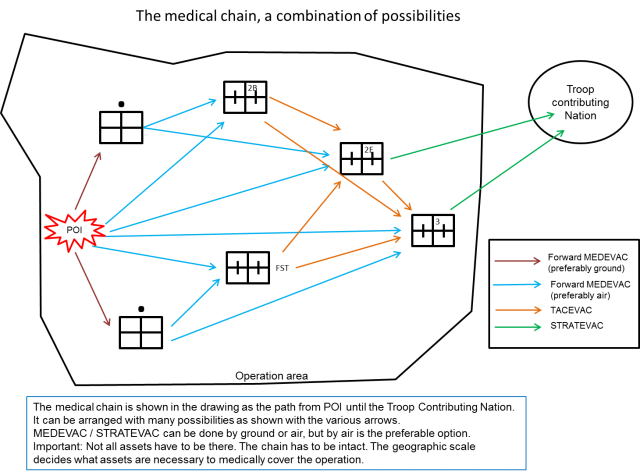
The starting point or entrance of the medical chain depends on the location where operations are conducted. For NATO the chain starts at the Point Of Injury (POI), which is the geographical point in the operations area where the patient got wounded and is not meant as the specific injury location on a patient. This point, of course, varies and is dependent on the operation that is executed during the mission. The anchor point of a medical chain is the ROLE 2E or ROLE 3. It is most of times fixed to one position and will stay on that position during the entire operation. This is also the place where the multi-national responsibility for patient handling changes to the national responsibility. STRATEVAC is within the NATO community a national responsibility. The ROLE 2E or ROLE 3 is the place from where Strategic Evacuation (STRATEVAC) can be conducted.
The chain itself is best compared with an elastic band. It can be extended to a certain point, designed into different shapes or folded up to a small circle. It pivots around the anchor point (ROLE 2E or ROLE 3) and it has a limit. Stretch it too far and the chain breaks on the weakest point. A weak point can be anything from the availability of specialized personnel (physician, surgical crew) and material (ambulance, CT-scan) to geographical (distance, high mountains) and meteorological events (dust storms, heavy rain, fog that prevents rotary wing movement). Stretching the elastic band means also that the band becomes thinner. This reflects the robustness of the chain and the availability of the assets for the Population At Risk (PAR). Stretched to the limit you lose flexibility in deploying and directing the assets to the PAR. The assets are spread and cannot be directed elsewhere without leaving PAR behind without medical care.
1.4. Responsibilities
Chain management is done in the staff element of an area responsible command level. It resides within the MED branch of the responsible level (brigade or higher) where the Medical Planner positions the various elements of the chain to fully cover the operations that are conducted in the Area Of Responsibility (AOR). A deep knowledge of the operational conduct of units (the possible client), a good view of the capabilities of all assets that form the medical chain (the elastic band) and a decent understanding of staff procedures (command and Control) are mandatory to execute medical chain management with success. In generic terms, the CJ5 department is responsible for the planning and CJ3 department is the authority for the execution of the operation, closely monitored via its Joint Operations Centre (JOC). Logistics are done by the CJ4 and the deployment of RW assets (RW MEDEVAC as well) is done within the CJ3/AIROPS. CJMED is the responsible department for force health protection (prevention measures) and medical chain management. This leads to the conclusion that CJMED is, in order to execute chain management successfully, connected with CJ5, CJ3 and CJ4 to ensure that the elements of the chain are placed on the right locations during the planning-phase of an operation, supplied
on time and is working cohesively during the execution of the operation.
1.5. Guidelines for Planning
NATO guidelines decide within what timeframe which type of element or medical intervention has to take place at minimum. The medical intervention gives the Medical planner an insight in the demanded quality of care that has to be present. It is the ultimate attempt to quantify the health structure in order to be able to use the medical expertise as a planning tool.
It is important to realize that the usability of an asset and its quality is very much depending on the ability of the personnel, combined with the availability of the equipment to apply the education and training the personnel had, to the mission. The NATO community strives to be as homogenised as possible, but nationalities differ and provide a variety in the manning, equipment, education and training and usability (caveat) of its medical personnel.
Furthermore the specific mission regulations define if there is going to be a more narrow approach to the timeframe as mentioned in the AJP4.10(b).
The risk our own troops run during the operation forms the basis for the medical support plan. The medical support plan is always a compromise between the number of available assets, their capability and quality versus the risk the People At Risk (PAR) is possibly going to have when it conducts operations. The severity of the risk is greatly influenced on the type of operation, the terrain type, weather (day-night, heat-cold) and the threat level produced by opposing forces. These factors are part of the input for the planning process the CJ 5 branch (plans) hosts to plan the operation for own troops.
Nevertheless, not being treated on time does not imply automatically that there is imminent threat of losing one’s life. The NATO medical timeline as described in the AJP 4.10(b) gives the medical planner the absolute timeframe. Medical decisions are made by physicians whether or not a patient’s survivability rate decreases if he is not treated within the mandatory timeframe. As stated before, there are a number of factors that decide how big the risk is.
2. Medical Support in North Afghanistan
2.1. Introduction to the Mission
The RESOLUTE SUPPORT (RS) mission in Afghanistan consists of seven Train Assist and Advice Commands (TAAC) commanded by the Headquarters RESOLUTE SUPPORT (HQ RS) in Kabul. The mission of the TAAC’s is to Train, Assist and Advise (TAA) their Afghan counterparts in their own area on their own procedures at Corps level. To summarize the goal is advising the Afghan partners to execute their work ‘the Afghan way’. The former mission ISAF had an active role in neutralizing threats in Afghanistan and providing aid via the Reconstruction & Development (R&D) process to its inhabitants. The RS mission has a different mandate. Afghanistan is in charge and should resolve its challenges in its own way. This process is supported by the RS community with dedicated advisors that help the Afghan National Defence and Security Forces (ANDSF) to use the national approved procedures. These procedures vary from personnel administration to planning for combined operations and logistic chain procedures. Although the process of getting used to certain procedures (in a sense: stick to the rules the government issued) is implemented in all governmental organizations, the RS community within the TAAC's focusses on the ANDSF. Above the TAAC level, HQ RS deals with the various ministerial levels and non-ANDSF organizations (Rule of law, civilian healthcare, finance, etc.).
2.2. TAAC N Medical Facts & Figures
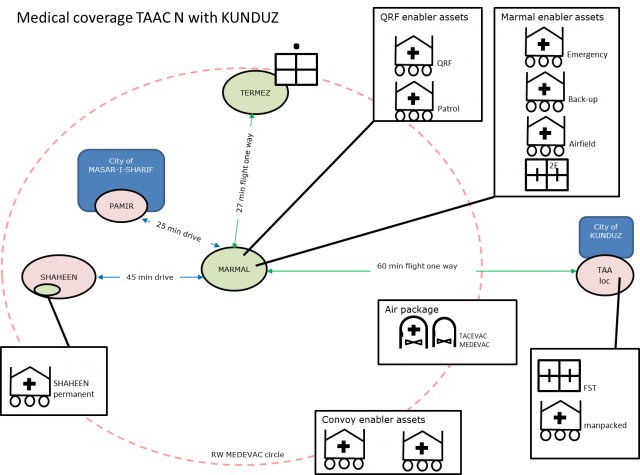
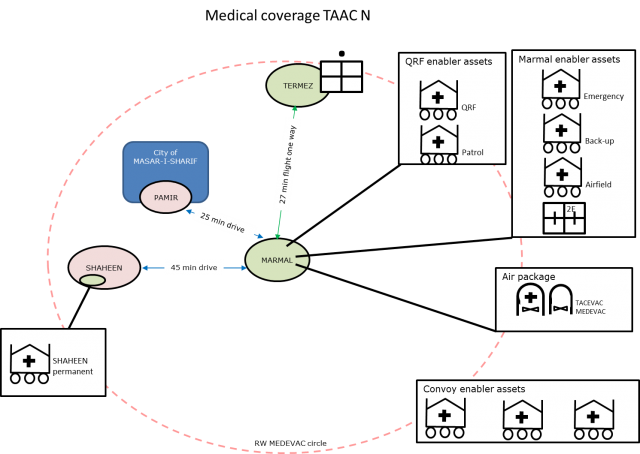
The structure of a TAAC was decided upon in advance and reflects the demand for troops to execute its mission. In TAAC North (N) the number of troops is roughly 1250 people coming from 21 different nations with Germany as lead nation. The medical forces consist of 1 ROLE 2E, 9 ground ambulances from 3 different nations with 3 levels of quality and 1 RW MEDEVAC asset. They are tasked by the Patient Evacuation Coordination Centre (PECC). The PECC tasks the MEDEVAC assets (ground and air) whenever there is a need for a medical evacuation. The Joint Operations Centre (JOC) coordinates all efforts and makes sure that the ambulances get protection from the manoeuvre force when they are driving ‘outside the wire’, or RW MEDEVAC is not using the same airspace as unmanned flying surveillance assets.
2.3. TAAC N Working Areas
The daily operations in TAAC N are to perform TAA to several locations in and around the city MASAR-I-SHARIF. For this purpose, TAAC N has 85 advisors that are moved with rotary wing and ground force to their respective locations. The medical chain provides medical coverage for the areas around the main base Camp MARMAL and the locations Camp PAMIR and Camp SHAHEEN, both TAA locations. There is besides at Camp MARMAL a permanent NATO presence at Camp SHAHEEN. Germany has as
lead nation a small footprint in the neighbouring country Uzbekistan (TERMEZ) that is covered with medical assets from Camp MARMAL as well. Although it is not part of the RS mission, the support for it is a TAAC N responsibility.
2.4. TAAC N Medical Support Plan
The medical plan to support TAAC N operations was specifically designed for the RESOLUTE SUPPORT mission. It had enough assets to cover the TAA operations. RW MEDEVAC covered the different locations, with ground-MEDEVAC to support the convoys in those areas where the RW cannot provide coverage. For me as medical planner the only thing left was to control the chain for any weak spots. The assets in the chain performed as expected and due to the threat level the number of patients was rather low, with Non Battle Injuries being the common patient type. The only difference in conjunction with the AJP 4.10(b) was the narrowing
of the MEDEVAC timeframe. Commander R ESOLUTE SUPPORT decided that from POI to ROLE 2 would not exceed 1 hr. For TAAC N not a problem as all operations were well within 30 minutes flying time.
3. And then there was KUNDUZ
3.1. Introduction to the Topic
After 4 months since my arrival in theatre, insurgents captured the city KUNDUZ in North Afghanistan. It came for many as a surprise. ANDSF were overwhelmed quickly and withdrew from the city. Refugees went to all directions and ended mainly on the airstrip in KUNDUZ where they desperately tried to get a plane to the city of MASAR-I-SHARIF. Insurgents effectively blocked the only highway, which connects the KABUL region with the North. Kunduz city was cut off from Afghanistan by road and air and the insurgents had the city under control. If this situation wanted to be solved it had to be done by the ANDSF forces in the North being the only ones that could go there. Within 24 hrs, the ANDSF reacted and started to consolidate their positions in order to prepare themselves to push the insurgents back and out of the city. Our Afghan mentees, the Corps commander and the key persons form his Corps staff went to KUNDUZ to assist and lead the ANDSF forces in that region. Within 24 hours after the taking of KUNDUZ our TAA mission area was expanded from a relative secure and small area into a very large area with a more hostile and remote spot 83 Nautical Miles (Nm) from Camp MARMAL. For the RESOLUTE SUPPORT TAA force, that location was at more than 1 hrs flight, unreachable by ground move and most likely the new Centre of Gravity for our operations for the coming month. It seemed at first sight impossible to cover this additional area.
3.2. Challenges for the Medical Plan
Setting up a medical chain from scratch on short notice with limited means that already have a standing task is possibly the biggest challenge a medical planner can face. No matter how you plan or divide the assets, if the number of operations increases the medical chain needs to grow with it. Without an increase of the right assets, there will always be a gap in the coverage. If RW MEDEVAC is flying to Kunduz, locations TERMEZ, PAMIR and SHAHEEN will be outside of timely MEDEVAC coverage. Leaving subsequently the people present at the risk of not being treated on time if anything happens. Ground MEDEVAC assets can cover that time gap, but only for PAMIR and SHAHEEN. TERMEZ and KUNDUZ are as mentioned before not reachable by ground.
3.3. Planning Facts & Influencing Factors
During the planning, cooperation with the CJ5 and the CJ3/AIROPS is crucial to understand what the operational manoeuvring concept is going to be and what your RW assets can. For obvious reasons the use of ground assets was not an option to support the KUNDUZ region. International law regarding flying conditions, mandatory crew rest, airfield medical support, etc. set the boundaries, which you cannot bypass. The ongoing operations have their own desired movement times concerning flying on the same time as the TAA work is done in other locations or additional cargo that has to be brought to various locations. The multinational environment has its own challenges. English language skills, national restrictions and caveats, mandatory requirements for ambulance crews put a strain on the planning process.
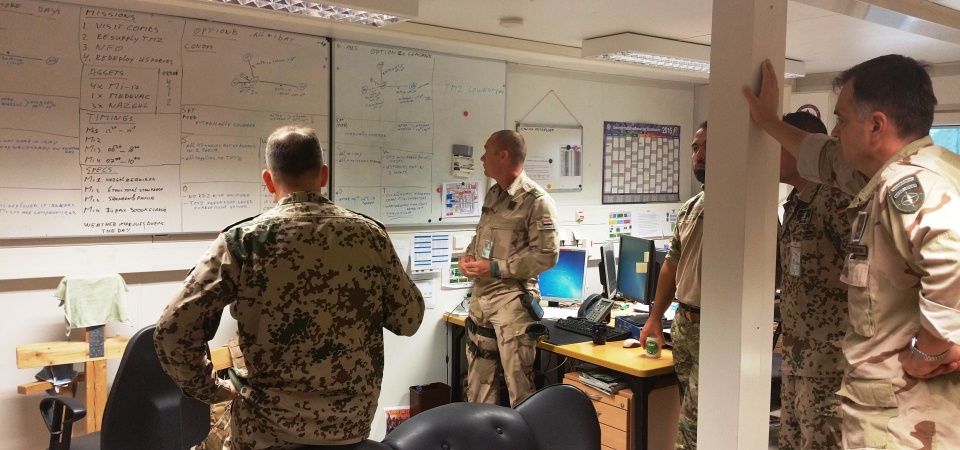
3.4. The Planning Process
During the planning process that is orchestrated by the CJ5 cell we got to the point
where we started to look into neighbouring TAAC’s to see if they could have feasible assets we could borrow. An FSE, FW TACEVAC or RW MEDEVAC would be very helpful. We even looked in to dividing our ROLE 2E in 2 parts to be able to put surgical crews in the Kunduz region. We refined the standing medical support to the ongoing operation, which still was to support the TAA effort in SHAHEEN and in PAMIR and provide medical support to MARMAL. All these factors were brought forward during the planning process and used to come up with a valid operational idea. Every operational idea was measured for its operational and medical feasibility, bringing sometimes the emotions of the planners to a boiling point when an idea, that looked promising at start, turned out to be unsupportable by the medical community without creating big coverage gaps. The risk of not getting sufficient medical care within the NATO medical timelines was transformed in a few options and put forward to the commander. He decided to decrease the standing operations if necessary and give the Kunduz region the higher priority.
3.5. The Biggest (Personal) Challenge in the Planning Process
One of the biggest challenges I faced was the misunderstanding regarding the “golden hour”. Many of the operational (non-medical) planners used it to describe a restriction in MEDEVAC timings. They would put a limit to an operational idea because it was more than one hour away from the home location of the ROLE 2E in MARMAL. However, the definition of the “Golden hour” is not reflecting the medical chain management. It is above all a term used to describe the survivability rate of a wounded person.
3.6. The Outcome of the Planning Process
The planning process ended with an operational plan that embedded the additional task in the Kunduz region into the standing tasks and was covered by sufficient medical assets. ROLE 1 support was created out of an ambulance team that deployed as a man packed ROLE 1 crew. A Forward Surgical Team (FST) borrowed from the neighbouring TAAC was brought into Kunduz to have DCS capability at the location with the RW MEDEVAC that were already in TAAC N in MARMAL to act as TACEVAC if necessary from Kunduz to the ROLE 2E in MARMAL. The FST is comparable to the NATO FSE, but is a US forces asset.
3.7. Contingencies
During the time the RW MEDEVAC was not available for the MARMAL region because of flying to KUNDUZ, crew-rest, maintenance or non-flying weather conditions, the ambulances were attached to the most critical tasks in the area. They provided sufficient medical support to patrols, ground moves to SHAHEEN and PAMIR with every convoy and compound protection. PAR that could not be reached in time was ordered to stay in their safe havens until the coverage was up again. Putting ambulances to every convoy task and having one asset away to Kunduz automatically meant that the TAA effort to PAMIR and SHAHEEN were reduced. There were fewer convoy possibilities for the advisors to go to their TAA locations.

4. Closing Remarks
4.1. Summary
Based on the NATO guidelines, changes in threat level, operations, PAR, climatological circumstances, geographic disposition or availability of assets require an adjustment of the medical chain to be able to deal with these changes. As part of an operation, it influences the manoeuvring possibilities a commander has. If the medical chain has to be spread out over a vast area, the ability to react timely and adequately to unexpected large patient numbers becomes a challenge, which results in a risk at itself. A risk that has to be forwarded to the commander’s attention. It is up to the commander to decide if he is willing to take that risk. If he does so and the risk becomes a reality, the medical chain has to and will deal with the outcome of this reality. With normal medical procedures if possible, executing MASCAL procedures if necessary.
4.2. Personal Opinions
- A robust presence in the responsible staff level helps the medical chain to be the force enabler instead of the showstopper. A thorough knowledge of the operational conduct of the manoeuvring elements is mandatory to be able to support the force properly.
- If you position the right surgical assets at the right geographical place and have it supported by adequate medical transport means with the right quality of personnel and equipment that manage those means and assets, the “elastic band” can stretch very far. It will mitigate the risks the commander has accepted in his plan and is
able to deal with possible casualties that result from the execution of the operation. - Medical planning is about fusing the medical coverage into the operational manoeuvring concept. The medical chain is defi
nitely not about stopping operations, it is about being prepared to treat personnel that saw accepted operational risks turn into reality.
Date: 01/19/2016
Source: MCIF 1/16