
Article: Michael Poppe, John Dorsch, Michael Barrie, Martijn Boosman, Roy Schoonwater, Erwin Dhondt, Karthik Sarma
Immersive Technologies Answer the Call for Sustain- able, Scalable Military Medical Simulation Training for Prolonged Casualty Care and Damage Control Resuscitation and Surgery
Background
Tactical combat casualty care (TCCC) training principles that focus on rapid casualty evaluation, lifesaving interventions, and rapid transport to definitive medical treatment have led to unprecedented levels of casualty survival in recent conflicts. However, current casualty management relies heavily on an operational environment that allows for rapid evacuation of a casualty to definitive medical management.
In preparation for Large Scale Combat Operations (LSCO) in denied environments, the complexity of medical management required for prolonged casualty care (PCC), damage control resuscitation (DCR), damage control surgery (DCS), and austere resuscitative surgical care (ARSC) in a far forward environment will require a new training paradigm. Exposure to realistic combat medicine is difficult during peacetime, as hospital exposure to trauma patients does not correlate directly to low-resource battlefield medicine. While didactic training remains the foundation of many courses, simulation exercises have been shown to have a more significant impact over traditional classroom teaching. Simulation exercises also provide a more realistic assessment environment to determine force readiness. However, traditional simulation can be difficult to scale to all service members.
Here, we outline the potential benefits of using Virtual Reality (VR) and Mixed Reality (MR) immersive technology to successfully scale casualty care simulation training.
Current simulation methods
Current simulation training for TCCC, PCC, DCR, DCS, and ARSC relies on in-person, synchronous simulated exercises. These simulations typically involve using actors trained to portray specific disease processes and presentations, manikin models, and/or live tissue models. Each model has its advantages and disadvantages. Standardized patients are more readily available for military training exercises; however, demonstrating severe injuries, such as amputations and realistic junctional wounds, is limited. Performing invasive interventions such as needle decompression on standardized patients is unethical. Additionally, standardized patients cannot demonstrate the critical physiologic findings and responses to treatment that are necessary components of medical simulation. Traditional simulation relies on conveying this information via verbal or written prompts, effectively breaking the immersion and realism of the encounter.

Figure 1: Comparison between full immersive VR and AR. (source: Martijn Boosman, SimX, Inc. (left); AI generated by the authors with Imagen 3 (right))
Manikins have been developed to fill this gap by allowing more realistic injury patterns, prompting learners with dynamic physiologic changes, and enabling participants to perform limited invasive procedures. However, the logistical challenges of bringing bulky and potentially delicate equipment into austere training environments are a significant limitation. Additionally, a single manikin can only portray a limited number of clinical scenarios. Large-scale manikin training also requires numerous manikins for a wide range of demographics, which is costly and logistically complicated.
Although live-tissue models provide unparalleled realism, their limited scalability necessitates a strategic approach to simulation. These logistically complex exercises tend to focus on training a small proportion of the force less frequently. The considerable planning, setup, and consumable costs associated with all simulation modalities often result in large-scale, full-mission profile exercises reserved as culminating capstone events.
Simulation technology such as virtual reality and mixed reality can fill the gap to provide high fidelity simulation training in preparation for full-mission profile exercises.
Immersive technology – Augmented Reality, Virtual Reality and Mixed Reality
Immersive technology platforms can address the need for logistically simple, less resource-intensive, and scalable high-fidelity simulation training. There are various immersive technologies currently available. All technologies utilize headsets (head-mounted displays) to portray digital features to the participant, but with varying ability to see the real world in the simulation. Augmented reality (AR) devices project digital images onto transparent glasses that appear like holograms in the real-world environment. Virtual Reality (VR) uses occlusive headsets to immerse participants in realistic digital environments. Mixed Reality (MR) combines virtual and real-world environments. (Figure 1)
This virtual approach significantly reduces the burden of scenario setup, breakdown, patient moulage, and consumable supplies compared to traditional simulation while offering the flexibility to train in any environment. The capabilities, strengths, and drawbacks of the technologies vary between platforms and are discussed in detail below.
MR training platforms allow for high-fidelity training with limited scalability
In MR, the participant sees a blend of the real-world environment and virtual components. Cameras and sensors on the headsets allow users to see their live surroundings and enable the headset to position virtual elements throughout the scene. This allows more flexibility to design a combat medicine scenario to meet specific training needs. For instance, a traditional manikin or cadaver can be modified with the virtual appearance of severe trauma such as a flail chest or extensive burns. Alternatively, a real-world vehicle could be modified to include active flames present. Also, realistic medical care supplies can be used in the scenario, such as intravenous line setups, medications, endotracheal intubation equipment, etc. These systems generally use hand tracking to allow participants to use real-world tools with their hands instead of controllers. This ability to incorporate a tactile training component (such as endotracheal intubation or chest tube placement) is a major strength of MR as a modality. (Figure 2)
A significant limitation of MR is its increased logistical complexity compared to other platforms, undermining a key advantage of training with immersive technology. For example, MR scenarios immersing learners in a deployed virtual environment around a physical manikin necessitate a dedicated training space with specialized colored screens to filter out the real world. Furthermore, the reliance on physical equipment like manikins and medical supplies for the simulation negates the scalability benefits of virtual environments. Consequently, current MR platforms face the same challenges as traditional simulation to scale high fidelity simulation training to a broad audience. However, this technology has the potential to add additional training benefits to simulation exercises that are already deployed for specialized team training.
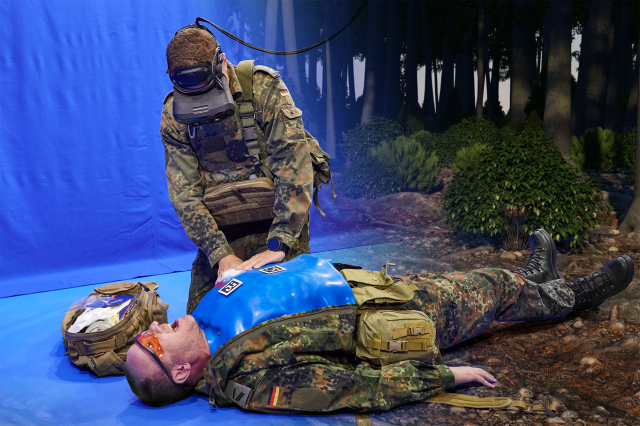
Figure 2: Example of a MR training system. (source: Christian Vogel, SimTCCC-XR, HENSOLDT)
VR training platforms allow the ability to train anywhere and anytime
In VR, the participant wears a headset that fully replaces their view of the real world. This allows for customization of environments, tools, and casualty features. Most VR headsets track head movements and do not require additional devices to be stationed around the participants’ training area. These systems use controllers or hand tracking to allow the participant to interact with the virtual world. (Figure 3)
Many VR headsets are stand-alone, connecting to the simulation wirelessly, and do not require a cable to directly link to a computer. Participants can walk around the environment naturally without complicated systems to manage cables or linked computers. A key advantage of VR training is its ability to accommodate geographically dispersed participants and further foster international cooperation by enabling joint training exercises regionally and even globally. Through networked simulation, VR enhances time and cost efficiency while expanding access to users for whom frequent travel is impractical. Furthermore, the ability for instructors to facilitate sessions remotely improves access to high-quality training on a global scale.
Limitations of VR come in the form of decreased ability to perform hands-on tasks. Because participants utilize controllers to interact with their environment, they have a limited ability to provide task training better suited for modalities with direct physical interaction and more tactile experiences. For this reason, VR simulation is largely used to train medical decision-making, team-based communication, and other cognitive tasks, rather than the procedural actions themselves. For example, a difficult airway scenario would focus on indications of cricothyrotomy and procedural sequence rather than identifying tactile feedback, such as feeling tracheal rings while placing the bougie device.

Figure 3: Full immersive VR training setup consisting of (1) moderator control screen, (2) VR headset(s) with full immersive view of the scene and (3) hand controllers. (source: SimX, Inc.)
In the search for scalable high-quality training, VR provides the solution
Given the specific need to provide realistic, immersive training for medically complex decision-making at scale, VR can offer the best balance of features relative to shortcomings to meet this need.
Commercially available solutions allow for a lightweight simulation system which includes a standard PC laptop and a VR headset for each participant. (Figure 4)
Devices can connect via the internet to perform simulation exercises while participants are co-located or connect remotely and execute the simulation with participants in separate locations. If internet connectivity is unavailable, the same multi-player scenarios can be run offline with co-located participants. These scenarios are designed to be moderated by an expert facilitator in real time. However, there are also features to allow autonomous scenario progression without the need for an expert facilitator, allowing participants to train on their own time. Incorporating automated educational content such as vital sign changes, physical exam findings, and their respective alterations based on interventions performed, decreases the facilitator’s mental load. It allows the focus to remain on participant proficiency. This lowers the barrier to entry for moderation and enables the simulation to scale more effectively. All actions can be tracked and recorded in real-time into an automatically generated after-action eport (AAR) to standardize comprehensive feedback and facilitate immediate debriefing following training exercises. VR scenarios also provide identical comparisons of training and outcomes with previous attempts. This lightweight simulation setup allows more flexibility, allowing training to happen anywhere at any time, removing barriers to high-quality simulation casualty care training.
The versatility and scalability of VR simulation make it a valuable training modality for a broad spectrum of personnel involved in military casualty care.
For Fighters/Combatants (all service members), VR offers an accessible and repeatable method for mastering fundamental TCCC skills. Its ability to create immersive and stressful scenarios allows every service member to practice critical decision-making and immediate life-saving interventions, regardless of location or access to traditional training resources such as dedicated simulation centers.
For medics (i.e. combat medics, SOF medics), VR provides an ideal platform for honing more advanced PCC and initial resuscitation skills. The technology can simulate complex and evolving patient conditions without pauses required for scene change/breakdown and setup, allowing medics to drill advanced protocols, refine assessment skills, and hone complex decision-making in resource-constrained and simulated austere environments. (Figure 5)
For doctors and nurses, VR/MR enables high-fidelity simulation of DCR, DCS, and ARSC scenarios. This modality allows participants to practice complex physiological management, collaborative teamwork, and decision-making in high-acuity situations, including the critical aspects of Crew/Crisis Resource Management (CRM).
Finally, for combined and interdisciplinary teams, a significant advantage of VR/MR is its ability to facilitate interprofessional and inter-echelon training without the need for geographic colocation. Simulating handoffs between different levels of care, identifying and mitigating communication breakdowns, and improving overall team coordination across the medical system become highly effective training objectives within a shared virtual environment.

Figure 4. Example of multi-person VR training in the field. (source: Marjolijn Lamme, SimX, Inc.)
VR is beneficial across all training backgrounds
The specific content for military medical training is well-suited to VR. Fundamental casualty management topics ranging from all service member TCCC to advanced topics such as critical care air transport (also called CCAT), as well as the handoffs required between each echelon of care, and critical CRM principles can all be incorporated into one scenario. For example, VR simulations can effectively train the dynamic interactions between a SOF operator and a SOF medic during a tactical mission that evolves into a casualty care event, emphasizing clear communication, shared situational awareness, and collaborative decision-making under pressure. Similarly, complex scenarios involving a surgeon and anesthesiologist managing a combined DCR/DCS challenge can be simulated to reinforce effective teamwork, communication of critical information, and anticipation of needs with acknowledgments for current limitations. There is also potential for more advanced procedures integrated into the simulations relating to DCR and DCS, as well as advanced medication support with realistic casualty physiology responses. The replication of such training using traditional simulation would require a large amount of expendable material usage to facilitate, which is a non-issue in the virtual space.
The platforms also allow for more unique mission sets, such as CBRN response. This degree of flexibility and breadth of possible content is possible in VR because many of the logistical complexities of standard manikin training are not required to run the simulation digitally. Other forms of immersive technology that use MR require compromises to allow real world manikins or equipment to be incorporated into the simulation. While MR may have specific use cases, such as incorporating hands-on training for specific procedural competency, VR platforms maintain the highest degree of flexibility with the lowest resource overhead.
VR in a blended learning environment
While traditional training methods like single-task trainers, cadaver labs, high-fidelity patient simulators, and live-tissue training (LTT) each offer unique benefits, VR technology is not intended to replace them entirely. Instead, it serves as a powerful complementary and integrative tool within a comprehensive, blended learning approach for military medical training. VR can provide immersive and interactive scenarios that build foundational knowledge and decision-making skills before trainees engage in more resource-intensive hands-on training with manikins or live tissue. By immersing learners in realistic virtual environments, VR can make abstract medical concepts more tangible and engaging, improving comprehension and retention compared to traditional classroom teaching alone while providing (repetitive) exposure to injury patterns and interventions that are difficult to recreate at scale using manikin or live tissue simulations. VR simulations can familiarize trainees with potential scenarios before participating in LTT, maximizing the learning potential of those limited and valuable resources. Furthermore, pre-deployment, cross-team training and team-building can begin earlier, before team members travel for deployment, to foster unit cohesion and identify potential friction early, allowing more time for directed interventions to occur prior to direct patient care. By strategically integrating VR into the existing training curriculum, educators and simulation operators can achieve a more robust, scalable, and effective “total solution” that maximizes the strengths of each modality.
Implementing VR: curriculum integration and requirements
Integrating VR/MR technology into existing military medical education and training curricula necessitates thoughtful planning and strategic adjustments. While the long-term benefits in scalability and effectiveness are significant, several key implementation areas must be considered.
The infrastructure required to support successful implementation includes the acquisition and maintenance of VR hardware, including headsets, controllers, and potentially supporting PCs. Reliable internet connectivity is essential for remote multi-player geographically dispersed scenarios, while dedicated training spaces are needed for co-located VR sessions. Instructors will require comprehensive training on how to effectively facilitate VR/MR simulations. This includes technical proficiency with the hardware and software, as well as learning to leverage the unique features of VR, such as automated task-tracking, first-person video recordings, and other tools to maximize the effectiveness of debriefing and feedback sessions. Ongoing technical support will be crucial for managing hardware and software issues, network connectivity, and ensuring the smooth operation of VR training sessions.
Successful VR integration into existing curricula depends on carefully mapping learning objectives to the VR system’s features. This demands either sourcing new VR-specific training modules and immersive scenarios or further developing current solutions to meet educational goals for programs like TCCC, PCC, DCR, DCS, ARSC, and CRM. Creating effective VR content – high-quality, medically accurate, and engaging – requires collaboration among medical experts, instructional designers, and VR developers. The significant technological tools, staffing, and time investments for VR scenario creation, implementation, and testing necessitate private-sector partnerships for financial viability. To shorten development timelines and reduce costs, a common approach is to collaborate with experienced private companies that already have the infrastructure for complex scenario creation. The military can then contribute subject matter expertise on training goals and objectives and conduct testing and evaluation to ensure desired outcomes. Finally, evaluating trainee performance within VR may require adapting existing assessment methods, often by incorporating standardized tools directly into the VR system to streamline AAR debriefing in alignment with current training structures

Figure 5. Examples of patients in a PCC VR scenario. (source: SimX, Inc.)
A phased and strategic approach is recommended for integrating VR/MR into the curriculum. Starting with pilot programs focused on specific training objectives can help evaluate effectiveness and identify potential challenges. Engaging early adopters among instructors and learners can foster enthusiasm and provide valuable feedback. Collaborating with experienced VR providers can streamline content development and provide essential technical support. Prioritizing the integration of VR in high-impact areas, such as scalable TCCC training or high-risk CRM scenarios, can demonstrate early value. Finally, establishing a process for ongoing evaluation and iterative improvement based on data and user feedback will ensure the long-term success of the VR training program.
Cost Considerations
Adopting VR technology involves initial investments in headsets, supporting hardware, software licenses, and content development. However, this approach offers significant long-term cost advantages over traditional manikin-based simulation. The expenses of purchasing, storing, transporting, and maintaining manikins, coupled with recurring travel, extensive man-hours, and continuous expendable supplies, are often substantially higher. Furthermore, many commercially available VR solutions offer customizable pricing options, allowing organizations to control spending according to their budgetary goals – a flexibility often lacking in the relatively static, one-size-fits-all pricing model of traditional manikins. This ability to tailor costs, combined with reducing or eliminating traditional expenses, presents VR as a more sustainable and potentially less expensive solution for scalable, high-fidelity medical training.
Conclusion – Way ahead
The mainstream adoption of affordable VR technology marks a pivotal moment for military medical simulation. Its integration promises not only reduced logistical burdens and enhanced accessibility for scalable, high-fidelity training in fundamental TCCC, PCC, DCR, and DCS but also offers a powerful platform for critical CRM and other collaborative training while foregoing the need for geographical colocation. VR’s place within a blended learning model is a versatile tool that complements existing methods, offering immersive practice and decision-making opportunities across all training backgrounds ranging from all service members treating injuries at the point of injury to medical and surgical providers. Realizing this potential will require thoughtful curriculum integration and infrastructure investment. However, the long-term gains in preparedness for LSCO in denied environments, coupled with the inherent cost-efficiencies compared to traditional methods, make further development and adoption of these platforms an imperative path ahead.
References available on request from the author.
Authors:
Lieutenant Commander (US Army MC)(OF-3) (sep) Michael Poppe, MD, Colonel (US Army MC)(OF-5) (ret.) John Dorsch, MD, Michael Barrie, MD, Martijn Boosman, MSc, Roy Schoonwater, MSc and Karthik Sarma, MD, SimX, Inc., USABrigadier general (BEL MC)(OF-6) (ret.) Erwin Dhondt, MD, MSc, SFS, MHA, DO Consultancy, Belgium
Contact: Lieutenant Commander (US Army MC)(OF-3) (sep) Michael Poppe, MD
Email: [email protected]
Figure 1: Comparison between full immersive VR and AR. (source: Martijn Boosman, SimX, Inc. (left); AI generated by the authors with Imagen 3 (right))
Figure 2: Example of a MR training system. (source: Christian Vogel, SimTCCC-XR, HENSOLDT)
Figure 3: Full immersive VR training setup consisting of (1) moderator control screen, (2) VR headset(s) with full immersive view of the scene and (3) hand controllers. (source: SimX, Inc.
Figure 4. Example of multi-person VR training in the field. (source: Marjolijn Lamme, SimX, Inc.
Figure 5. Examples of patients in a PCC VR scenario. (source: SimX, Inc.)
Date: 07/16/2025
Source: EMMS Magazine 2025











