
Almanac
Germany, Federal Republic



Surgeon General
Lieutenant General Ralf Hoffmann, MD
Deputy of the Inspector General:
Lieutenant General Andreas Hoppe / Source: Ministry of Defence
Von-Kuhl-Strasse 50
56070 Koblenz
GERMANY
Pictures and Graphics: Wikimedia Commons
*The entry will be updated in September*
CONTENT
- Joint Medical Service
- Air Force
- Army
- Joint Support and Enabling Service
- Navy
Context
The medical services of the Bundeswehr were centralized into the Bundeswehr Joint Medical Service in 2002. The responsibility for the medical support of the vast majority of the military was transferred to this major organisational element. However, because of the specialised needs of military aviation, an Aeromedical Service was retained within the aeronautical units maintained by the Air Force, Army and Navy of the Bundeswehr, and a centralised aeromedical institution under the leadership of the Surgeon General of the Air Force was established to provide specific support in the entire field of Aerospace Medicine.
JOINT MEDICAL SERVICE
Basic Task of the Military Medical Service
The core task of the Bundeswehr Joint Medical Service (BwJMS) is to protect, sustain and restore the health of service personnel.
The spectrum of health care services in the Bundeswehr is tailored to the requirements of operations abroad and is the product of all capabilities and capacities needed for protecting, maintaining, promoting and restoring the physical and mental health, social well-being and operational readiness of the soldiers in accordance with current scientific and technological standards. These services include tasks of preventive medical care, free health services, military medicine, dental medicine, veterinary medicine, military pharmacy (including food chemistry), CBRN medical defence and other tasks under public law.
From this spectrum, specific services will be provided for soldiers in the fields of health care, medical training and medical support. The guiding principle for the quality of medical care during deployments abroad is to guarantee a treatment outcome that, in terms of quality, corresponds to medical standards in Germany. For that purpose, the medical service engages in specific projects of cooperation with national military and civilian partners also under the aspect of burden-sharing.
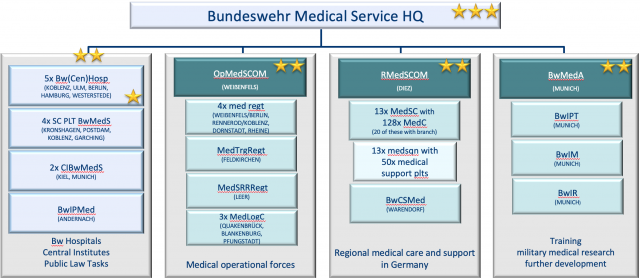
Structure
Consistent orientation towards mission-related tasks, the streamlining of command and control structures and the continued focus on tasks that require a medical licence are essential determinants of the Bundeswehr Joint Medical Service.
In order to achieve these goals and maintain personnel sustainability, the Bundeswehr Joint Medical Service comprises a total of approximately 18.000 military and 3.000 civilian posts.
Source: Ministry of Defence
The Surgeon General is the commanding general of the German Joint Medical Service and, in medical matters, exercises control over the medical services of all other services and branches of the Bundeswehr.
He also commands the Bundeswehr Medical Service Headquarters (BwMS HQ) located in Koblenz, which at field army level is the highest military medical command in Germany. It is under the direct control of the Federal Ministry of Defence (FMoD).
All command and control structures of the Bundeswehr Medical Service are organized at the Bundeswehr Medical Service Headquarters, focusing on a process-oriented organisation rather than on customary staff branches. In the training branch, for example, staff from personnel management works alongside with staff from operations and readiness.
The Bundeswehr Medical Service Headquarters (BwMedSHQ) is directly subordinated to the Federal Ministry of Defence and supports the Surgeon General of the Bundeswehr in carrying out his duties. Therefore all processes for the Bundeswehr Joint Medical Service, such as planning, leadership, control and steering, are coordinated on one tier. That also applies to the professional leadership of the medical services in the branches of military services and military organization sector. The planning conceptually anticipates potential future military operations and evaluates the capabilities and resources required to fulfill the mission. Thereby all activities will be considered, which are aligned to the future composition of the medical service as an enabler in combination with all armed forces. Primarily the fulfillment of the commitments made to the NATO and EU as well as the national functional guidelines and timelines for the medical care pursuant to NATO standards are directive for the planning. The national implementation of these framework specifications takes place via the system networks of the capability profile of the Bundeswehr. The scope, capabilities and the material equipment are determined by the planning variables of the essential users (especially the army, air force and navy) with regard to the strength of the personnel approach and the requirements for protections and mobility.
At the same time BwMedSHQ assumes the function of a monitoring authority for the Bundeswehr in the field of public law supervision, insofar as this has been transferred to the BwMedSHQ by statutory regulations.
The large number of challenging tasks and the presence of high-ranking representatives of the Bundeswehr Joint Medical Service clearly shows the complexity of the task as well as the importance of the BwMedSHQ.
Good health care is based, among other things, on high-quality equipment and facilities. The rapid development cycles in medical technology must also be met in the Bundeswehr Joint Medical Service. This is the only way to achieve appropriate treatment results based on state-of-the-art science and technology. Current procedures in the procurement of commercially available medical equipment cannot keep pace with this at present. In order to accelerate the procurement of medical material by the Federal Office for Infrastructure, Environmental Protection and Services of Bundeswehr, a functional element was set up in the Bundeswehr Medical Service Headquarters. Another goal is to relieve the Federal Office of Bundeswehr Equipment, Information Technology and In-Service Support. By transferring the procurement of non-weapon system-related products (including commercially available medical material) to the Federal Office for Infrastructure, Environmental Protection and Services of Bundeswehr, the aim is to focus the Federal Office of Bundeswehr Equipment, Information Technology and In-Service Support on its core task. It was possible to achieve an initial capability with own forces and resources. Full establishment will only be possible in the medium term.
The task spectrum covered ranges from cross-border crisis management to collective and national defence. A particular focus is on CBRN (chemical, biological, radiological, nuclear) medical defence and on the coordination of strategic, supra-national medical evacuation.
The Medical Service Command maintains an Operations Center dealing with special challenges. The COVID 19 pandemic required the bundling of information, preparations and central support decisions in the course of administrative assistance. The medical support for the reinforcement of NATO's eastern flank in connection with the war in Ukraine and the management of war casualties are currently being coordinated in the Operations Center.
A feature unique to the Medical Service is its responsibility for the organisation and management of Strategic Aeromedical Evacuation (StratAirMedEvac) operations. The responsibility includes stationing, military security, alerts and mobilisation.
Its responsibility for the organisation and management of Strategic Aeromedical Evacuation (StratAirMedEvac) operations is a unique feature of the Medical Service. The responsibility includes stationing, military security, alerts and mobilisation.
As regards equipment, medical materiel logistics and protective tasks, Bundeswehr Medical Service Headquarters in particular takes charge on a centralised basis, of the following tasks for Bundeswehr routine duty at home and on deployment:
- conducting of duties to be carried out by the person in charge of operational and supply responsibility in order to maintain deployment capability and readiness for operations;
- development of basic requirements and principles for the equipment of the Bundeswehr Joint Medical Service;
- conceptualization of technical requirements in relation to medical materiel logistics to support the provision of medical care;
- estimation of the situation, planning and issuance of orders in relation to logistics;
- management of logistics personnel in the Bundeswehr Joint Medical Service; and
- execution of protection duties for CRBN defence and self-protection in the Bundeswehr Joint Medical Service.
In 2019 the Multinational Medical Coordination Centre / European Medical Command (MMCC/EMC) was established in Koblenz. Task of the MMCC/EMC is to provide coordinating support to the medical services of NATO and EU. The experience made in the management of large-scale medical emergencies or the Ebola crisis has shown that the interdependencies between public health protection and external and internal security are increasing. A future core task of MMCC/EMC will be civil-military cooperation, in particular with the organisations and institutions of the EU nations and establishments. MMCC/EMC supports in the provision and assessment of the medical situation picture for NATO and EU, which is jointly developed with the nations and NATO/EU organisations.
The five Bundeswehr Hospitals are commanded directly by the BwMSHQ. Therefore, a division of hospital management is integrated into the command structure of the BwMSHQ under the direct control of the Deputy Commanding General of the BwMSHQ.
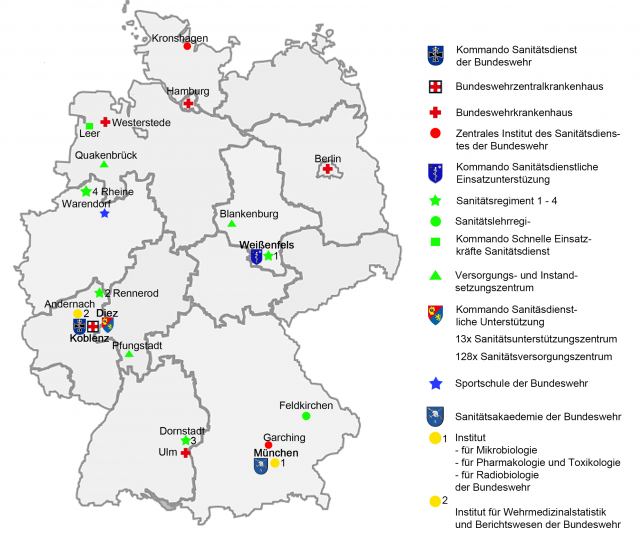
Five Bundeswehr Hospitals located in Koblenz, Ulm, Berlin, Hamburg and Westerstede are directly subordinated to the Bundeswehr Medical Service Headquarters as well as the Central Institutes of the Bundeswehr Medical Service at Kiel and Munich and Supervisory Centers for Public Law Tasks of the Bundeswehr Medical Service North (Kiel), West (Koblenz), East (Potsdam) and South (Munich).
The military hospitals take care of a multitude of tasks, which are all necessary to maintain the basic operation of the hospitals. As part of the findings from our participation in missions, since 2007 the military hospitals consistently have been aligned to the requirements for the provision of medical care in use. Without the execution of all these tasks, an adequate treatment of the personnel on missions would be impossible.
Therefore, military hospitals treat military personnel as well as civilian patients. To acquire the requested spectrum of patients, the military hospitals are involved in the civilian land-based and airborne emergency service in the respective region. The military hospitals include a capacity of 1811 beds to serve as training centres for our medical personnel, to have a suitable range of diseases and injuries and to have special skills to treat patients with (poly)trauma, patients with mission-related mental and psycho-traumatic disorders and patients with infectious diseases. Of their total of 1811 beds, 787 are approved for civilian inpatient care and thus serve as a contribution to the overall German healthcare system. Without this integration in the civilian health care system, the military hospitals would not be able to fulfil their task to qualify the physicians for missions. Thus a relevant spectrum of patients and a relevant mix of medical cases or injuries is needed, in order to prepare the physicians for their duties.
The military hospitals thus form the central part of the commitment to ensure the effectivity of the medical service. In addition to the provision of their own staff for missions abroad, they are primarily responsible for the medical education of members of the Medical Corps, pre-deployment training, continuing education and training of our medical specialists.
At the division level, two commands and the Bundeswehr Medical Service Academy are subordinate to the Bundeswehr Medical Service Headquarters.
The leadership mission "medical support on operations" is executed at Operational Medical Support Command (OMSCOM) in WEISSENFELS. Subordinate to this capability coordination command are four medical regiments, Medical Training Regiment, and Medical Service Rapid Reaction Regiment, as well as three Medical Logistics Centres. Operational Medical Support Command in WEISSENFELS – as kind of "permanent lead command" – is thus responsible for providing medical operational forces and for coordinating and steering their pre-deployment training.
The Bundeswehr Joint Medical Service has four Medical Regiments, elements of which will be stationed at or close to Bundeswehr hospitals in order to strengthen the training and exercise system and to increase options for the mutual support between field units and Bundeswehr hospitals. Three Medical Regiments are located in Weißenfels/Berlin, Rennerod/Koblenz and Dornstadt/Ulm. The main task of the medical regiments is to provide personnel and material to maintain a hospital on deployment, augmented by medical specialists from the military hospitals and the regional medical facilities.
Related to collective defence and as a consequence of the latest NATO Summits, future medical units will be also stationed in the vicinity of the potential beneficiaries. That was one of the reasons the fourth Medical Regiment was recently stationed in Rheine.
In addition, the Medical Service Rapid Reaction Regiment in Leer combines all airmobile and airborne medical capabilities of the Bundeswehr Joint Medical Service to ensure that medical care and support are made available to troops on deployments abroad within a very short period of time. During longer deployments, rapid response forces are relieved by stabilization forces.
Basic training of medical trainee soldiers and pre-deployment training of medical personnel is provided by the Medical Training Regiment in Feldkirchen.
Regional Medical Support Command (RMSCOM) in Diez exercises command and control over all regional medical facilities in Germany. In numbers, there are 13 Medical Support Centres, 128 Medical Clinics, 15 Medical Clinics with Speciality Services and the Bundeswehr Centre of Sports Medicine. The aim is to ensure that military personnel never is more than 30 kilometres or 30 minutes away from the nearest regional medical treatment facility.
The spectrum of the Medical Support Centres includes Medical care by General Practitioners, dental care, medical care by specialists (out-patient clinics) and occupational health care. The Bundeswehr Centre of Sports Medicine provides advice to military sports teams, works in research on the topic of sports and preventive medicine, develops concepts (individual personal fitness training et alia) and has a significant part in the rehabilitation of personnel injured during missions abroad.
In addition, the Medical Support Centres are also in command of the 13 Medical Squadrons whose task it is to provide medical support to the troops.
The Bundeswehr Medical Service Academy in MUNICH constitutes the fourth capability pillar. It is the central research, capability development and teaching facility of the Bundeswehr Medical Service. In addition, there are three available departmental research facilities within the FMoD area of responsibility for the field of CBRN medical defence.
Institutes, Research and Public Health
Veterinary and pharmaceutical laboratory diagnostics including potable water and food examination are provided by Central Institutes of the Bundeswehr Medical Service at Kiel and Munich.
Medical research in the field of detecting and preventing CBRN-Threats is conducted in the laboratories of the institutes affiliated with the Medical Service Academy in Munich. The Bundeswehr Institutes of Microbiology, of Pharmacology and Toxicology, and of Radiobiology are also stationed in Munich. The Bundeswehr Institute of Preventive Medicine in Andernach and provides research and operational assets for injury protection, health protection and surveillance capabilities.
Source: Ministry of Defence
Medical Logistics
Medical logistics is provided by three Medical Logistics Centres located in Quakenbrück, Blankenburg and Pfungstadt.
The main task of a Medical Logistics Centre is to supply military missions and regional medical facilities with pharmaceuticals and medical devices. Pharmacists and pharmacy staff assure storing and shipment in accordance with national and international regulations.
Training and provision of personnel for military missions is another important aspect. The regional medical facilities are provided with advice on drug selection and proper usage of medicines. In addition, the centres provide repair and maintenance of medical equipment.
Thus, the Medical Logistics Centres cover a variety of logistical and pharmaceutical capabilities to ensure sufficient health care to the soldiers of the Deutsche Bundeswehr.
Field Deployments
Medical care for personnel who become ill, injured or wounded during deployment is provided through the medical evacuation chain. This chain of closely interlocking phases ranges from self and buddy aid through medical care in field medical treatment facilities to final clinical treatment and rehabilitation in Germany. The medical evacuation chain consists of four medical service treatment levels. Depending on the severity of the illness or injury, the patient will pass through some or all of these levels. Well-trained specialist personnel and efficient, mobile equipment are available for the benefit of personnel at all times.
First aid through self and buddy aid forms the start of the medical evacuation chain. Initial emergency medical care is rendered at Mobile Aid Stations (Role 1). Trained medical specialists perform on-site triage, shock and pain management as well as haemostatic measures. They also ensure the clearance of the respiratory tract and artificial ventilation.
Complimentary emergency diagnostic services and treatment are provided at Mobile Surgical Hospitals (Role 2). These are able to deal with acute injuries and disorders and the relevant surgeons and anaesthetists. A Mobile Surgical Hospital consists of mobile containers. Tents are used in some cases. The size and facilities of a centre are adapted to the requirements of each deployment.
Field Hospitals (Role 3) provide in-patient and out-patient specialist medical care. They have extended surgical, intensive care and specialist diagnostic and treatment facilities and, if necessary, can stabilise casualties for direct evacuation back to Germany.
In relation to the type and severity of their injuries, casualties are generally transported back to Germany in specially equipped Bundeswehr aircraft within the framework of StratAirMedEvac. Special equipment includes Patient Transport Units (PTU) for the movement of intensive care patients. Six PTU can be installed in Airbus A-310 aircraft operated by the Deutsche Luftwaffe (German Air Force, see Luftwaffe).
The main elements at Role 4 level are the Bundeswehr Hospitals in Germany. If necessary, civilian hospitals and rehabilitation centres are also used. These facilities provide the further treatment of patients who have been evacuated from the area of deployment. As a rule, strategic air medical evacuation aircraft land in the reserved military zone of Cologne-Bonn airport. From there, patients are transferred to the Bundeswehr hospitals.
Protected Casualty Transport Vehicles used (examples)
Current missions:
1999 – KFOR / Kosovo
2015 – CD / CBI Jordan / Iraq
2006 – UNIFIL / Lebanon
2008 – ATALANTA / Horn of Africa
2013 – MINUSMA / Mali
2013 – EUTM / Mali
2013 – MINURSO / West Sahara
2017 – eFP BG LTU / Lithuania
2019 – UNMHA / Yemen
Civil-Military Cooperation
The Bundeswehr cooperates with its civilian counterparts in terms of measures, personnel and resources. The purpose of the cooperation is to promote a closer relationship between Bundeswehr units on the one hand and civilian authorities and the civilian population on the other.
The Bundeswehr Joint Medical Service has established seven centres for civil-military cooperation across Germany for subsidiary medical support.
These centres have the following capabilities:
- Conducting triage and providing medical treatment within the scope of available capacities, operating facilities in the following medical support roles:
- Role 1 – mobile aid station. (All-terrain) patient evacuation capacity and casualty decontamination capability required planning and allocation of the necessary medical personnel as determined by the Bundeswehr Medical Service Headquarters.
- Role 2 – mobile surgical hospital. Requires at least one week of planning (including reconnaissance, transportation and setup) and allocation of the necessary medical personnel as determined by the Bundeswehr Medical Service Headquarters.
The above capabilities can only be provided with the involvement of medical personnel from the Bundeswehr hospitals and the Central Institute of the Bundeswehr Medical Service and, where applicable, only with the (involvement, kein guter Ausdruck) of materiel resources from the command area, since it may not be possible for one centre alone to provide these capabilities.
Medical Services of the Army, Navy, Airforce and Joint Support and Enabling Service
In the year 2000, the personnel of all medical corps of the branches of the armed forces were combined into the Bundeswehr Joint Medical Service. Only smaller subunits in every branch of the armed forces were left, led by their own surgeon generals. The surgeon generals are responsible for health and medical related aspects in view of their branches’ specialties.
The Army Medical Corps
The Surgeon General of the Army commands the Army Medical Corps on behalf of the Army Chief of Staff and the Surgeon General of the Bundeswehr as a specialized service. At the same time, he represents the interests of the Army with respect to the Surgeon General of the Bundeswehr and vice versa.
The Surgeon General of the Army is located in the German Army Headquarters and advises the Army Commanders directly on medical service matters and those relating to the Medical Services of the Army. All Corps and Division Surgeons, the Flight Surgeon of the Army, and the Senior Medical Officer in the Army Training Command work under his command.
Medical Service of the Rapid Response Forces Division
The Medical Service of the RRFD works under the command of the Division Surgeon. The Special Operations and Air Maneuver Forces of the Army are located in this division. The potential deployments of the RRFD are characterized in particular by a high degree of mobility, air mobility, a high level of threat, the bridging of large distances with an appropriate distance to their own troops, surprise, speed and secrecy.
The specific characteristics of Army Special Operations and Air Maneuver Forces training, exercise and deployment are considered in medical services support, so that in the two paratrooper regiments of the Airborne Brigade and in the SOF their own medical personnel are organically deployed to support the troops.
Airborne mobile aid station and rescue vehicle BV 206 - optimized for the deployment of the airborne troops
The two independent Airborne Medical Companies of the Paratrooper Regiments are commanded by Medical Staff Officers. They each have an airborne patient treatment platoon, two airborne rescue platoons and their own Patient Evacuation Coordination Cell (PECC). The ability to parachute jump is an essential precondition in order to be able to follow without restriction the parachute regiments, which are to be supported in all deployment types/options. For this reason, both Airborne Medical Companies are fully capable of parachute jumping.
Deployments of the Special Operations Forces (SOF) of the Army receive medical support from air-mobile emergency physician teams and air-mobile medical teams, as well as air-transportable Role 1 facilities. An Air-Mobile Emergency Physician Team of the SOF consists of two Special Forces Senior NCO paramedics, a SOF emergency physician, and a driver. The Special Forces Senior NCO paramedics are fully trained as both commandos and paramedics. The SOF emergency physician is a Medical (Staff) Officer who is specialized in emergency medicine and SOF-specific infantry and other medical service training.
Wiesel 2 San – patient care optimized in terms of size and weight reduction
The option of being ready for deployment in special operations can only be guaranteedby the broad and in-depth training of everyone involved. The forces providing medical care must be aware of the effects of excessive heat in the desert, tropical conditions or extremely low temperatures in Arctic latitudes in the same way as they are acquainted with the clinical pictures? and specific features of the respective climate zones.
The Medical Service of the German Navy
The Medical Service of the German Navy ensures medical care for all seagoing and flying units of the fleet, deployed or in port, including the Navy´s special and specialized forces, using the very latest in medical technology and procedures. The Navy Medical Service provides health support for Navy operations and training ashore and afloat. It works closely together with the Bundeswehr Joint Medical Service to provide primary surgery and dental care during Navy operations and training afloat.
The Naval Medical Institute
The Naval Medical Institute covers the field of maritime medicine and the entire range of scientific, research, care-providing, preventive and teaching facilities. Due to the increasing importance of departmental research, it was divided into the three sections Maritime Medicine, Diving and Hyperbaric Medicine and Research and Education.
Deployments Afloat
The medical capabilities of deployed Navy units vary strongly and depend on the platform and the embarked personnel. All levels of medical care can be provided, ranging from two Role 2 naval rescue centres (NRC) in which several medical teams perform primary surgery within clinical timelines on a combat support ship, to surgeons and anaesthesiologists embarked on frigates, to shipboard physicians or highly trained ship´s paramedics performing pre-hospital emergency care.
German Air Force Centre for Aerospace Medicine (AFCAM)
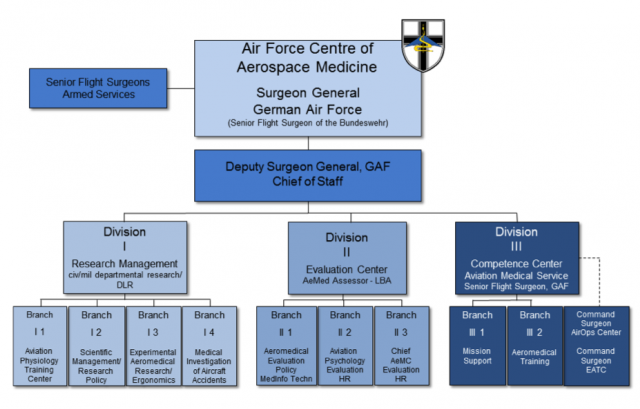
By fusion of the former office of the Surgeon General German Air Force and the Air Force Institute of Aviation Medicine, a new institution was established in October 2013: the German Air Force Centre for Aerospace Medicine (Zentrum für Luft- und Raumfahrtmedizin der Luftwaffe (ZentrLuRMedLw). This centre covers all responsibilities for the “Aerospace Medicine” sector on behalf of the Bundeswehr including the Flight Medical Service of all flying units. While the Surgeon General of the Air Force is the highest-ranking Flight Surgeon of the Bundeswehr, the Chief Flight Surgeons of the Army and the Navy are assigned to AFCAM, and the head of one of the three divisions of AFCAM is the Chief Flight Surgeon of the Air Force.
The Flight Medical Service of the German Air Force
The Flight Medical Service of the German Air Force is responsible for providing flight medicine in all operational air wings, global mission support, health support administration, aeromedical training and medical equipment for our flight surgeon clinics as well as AE (aeromedical evacuation) onboard our various aircraft. The air wing’s flight surgeon clinics comprise of flight surgeons, flight surgeon assistants, physiotherapists and sports trainers. They provide medical support as family practitioners of our aviators and air traffic controllers as family practitioners and function as aeromedical examiners (AME), as well. Additionally, they support the German AE system as medical directors (MD) onboard our AE-aircraft. Command, support and guidance are provided by Division III, the Competence Centre for Flight Medical Service and the Chief Flight Surgeon of the Air Force.
Flight surgeons in the field / Aeromedical Evacuation
Appropriate and continuous aeromedical support is also an essential factor in successfully maintaining military flight operations at a deployed operating base. Special requirements thus apply with regard to the training, motivation and proficiency of flight surgeons stationed in the field. A deployed flight surgeon must also be capable of acting as an Aeromedical Evacuation Coordinating Officer (AECO), providing the aeromedical expertise required by the casualty evacuation chain.
A flight surgeon must have the abilities required to perform the duties of the Medical Director (MD) in all Tactical Aeromedical Evacuation (TacAE) and Strategic Aeromedical Evacuation (StratAE) missions and, like the civilian senior emergency physician, to coordinate the civilian emergency medical services during airborne evacuation. A Medical Crew Chief (MCC) is at hand to assist the flight surgeon. The Aeromedical Evacuation (AE) flight crew also includes the Medical Device Technician, whose job it is to ensure that onboard medical equipment and material are both functional and safe. The direct medical treatment and monitoring of wounded, injured and sick personnel being transported by aircraft are provided by the specialists of the Bundeswehr Joint Medical Service.
The Medical Service in the Joint Support and Enabling Service
The Medical Service in the JSES provides specialist advice for force commanders, performs military pharmaceutical tasks for the Bundeswehr, and fulfils specific specialist tasks. The JSES further ensures the provision of medical care at Bundeswehr agencies abroad (outside of military operations).
Senior Medical Officers (SMOs) in capability coordination commands serve as medical advisors to force commanders. In addition, they analyse physical and ergonomic requirement profiles for various specialist tasks and contribute medical expertise to the further development of technology and procedures. These tasks are especially important with respect to future personnel development.
The Surgeon General of the Joint Support and Enabling Service, the Bundeswehr Logistics Centre, and medical materiel depots perform military pharmaceutical tasks. Military pharmacy elements have in-service, maintenance and supply responsibility for medical materiel in the JSES. They furthermore represent the interests and technical issues of medical materiel management in the further development of logistic systems at the interface to the main logistics process.
A broad range of specific specialist tasks are performed in national and international HQs, authorities, commands and agencies and are carried out by medical advisors, special instructors at schools, veterinarians for working dogs, and toxicologists in the CBRN corps.
The Subdivision of the Surgeon General of the Joint Support and Enabling Service controls and coordinates health support and medical materiel logistics in the JSES.
The responsibilities of the Surgeon General include:
- assessing medical operational readiness in his area of responsibility,
- providing expert advice to the Chief of Staff of the Joint Support and Enabling Service and the Surgeon General of the Bundeswehr in all medical matters of the JSES,
- assuming in-service and supply responsibility for medical materiel in his area of responsibility,
- exercising functional control over subordinate medical elements and providing intermediary or final reports for decision-making processes.
AIR FORCE


| Surgeon General | Address: | Armed Forces Personnel: |
| Dr Bernhard Groß Brigadier General MC | Flughafenstraße 1 | 27.535 |
Source: Ministry of Defence
German Air Force Centre for Aerospace Medicine (AFCAM)
By fusion of the former office of the Surgeon General German Air Force and the Air Force Institute of Aviation Medicine, a new institution was established in October 2013: the German Air Force Centre for Aerospace Medicine (Zentrum für Luft- und Raumfahrtmedizin der Luftwaffe (ZentrLuRMedLw). This centre covers all responsibilities for the “Aerospace Medicine” sector on behalf of the Bundeswehr including the Flight Medical Service of all flying units.
While the Surgeon General of the Air Force is the highest-ranking Flight Surgeon of the Bundeswehr, the Chief Flight Surgeons of the Army and the Navy are assigned to AFCAM, and the head of one of the three divisions of AFCAM is the Chief Flight Surgeon of the Air Force.
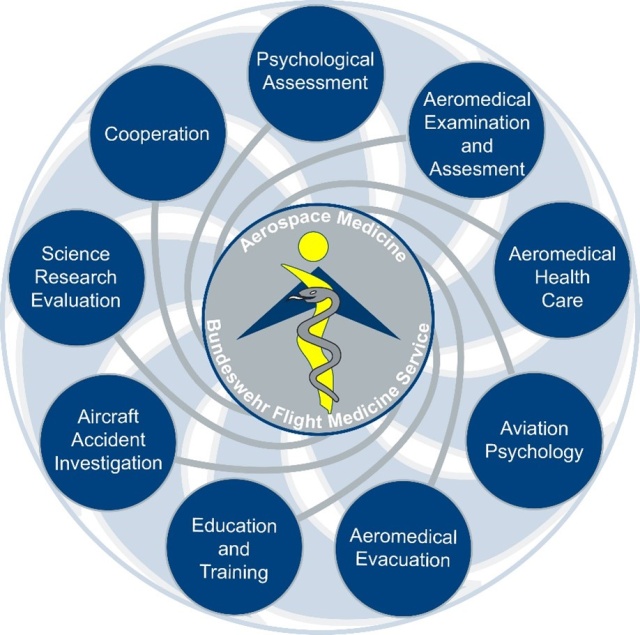
Source: Ministry of Defence
The duties of the Flight Medical Services include not only the medical examination, evaluation and support of military flight personnel but also the evaluation of pilots on behalf of civilian aviation authorities. The Centre for Aerospace Medicine has different fields of competence which are shown above. The selection of candidates for flying duties by means of computer and simulator-based testing of aptitude and trainability, the provision of national and international training courses in aerospace physiology and aviation medicine, as well as the testing of aircraft, aircraft equipment, flight clothing and aviation life support equipment with regard to their suitability for use by the flying crews. Further tasks include the forensic investigation of aircraft accidents, including toxicological and DNA analysis, the processing of all aspects of flight physiology, and intervention in crisis situations. As a science-based service provider, the AFCAM has to assure the quality of its services by conducting its own scientific research. All tasks relating to scientific aspects, research, testing and development in the Centre for Aerospace Medicine of the German Air Force are carried in one division.
The Surgeon General of the German Air Force is in command of the AFCAM, which comprises the personnel and facilities of the units of the former Institute of Aviation Medicine currently based in Fürstenfeldbruck, Manching and Bückeburg together with those of the previous Office of the Surgeon General of the German Air Force and the majority of those of the previous advisory services within the command units based at Köln-Wahn. The Flight Physiology Training Centre with its large-scale equipment typical for aerospace physiology, such as human centrifuge, high altitude simulation chamber and disorientation trainer, is currently located in Königsbrück, close to Dresden in Saxony. Based on the cooperation agreement between the Federal Minister of Defence and the German Aerospace Centre (DLR) in May 2014, parts of the AFCAM will move in a new building on the DLR compound in Cologne in October 2022. The AFCAM will become part of the aerospace medicine campus in order to develop a European competence center in future.
Close cooperation with the DLR will include the implementation and supervision of specific research projects, the mutual use of largescale equipment as a cost-saving measure, and the exchange of personnel for training purposes and to promote young researchers.
The AFCAM also issues medical guidance and direction to the flight surgeon units in the wings of the German Air Force and is additionally responsible for deployment support, healthcare, logistics, administration and training. In the areas of international and national joint projects, research orientation and quality management, the Surgeon General of the German Air Force has the support of a Scientific Coordinator.
Source: Ministry of Defence
The Flight Medical Service of the German Air Force
The Flight Medical Service of the German Air Force is responsible for providing flight medicine in all operational air wings, global mission support, health support administration, aeromedical training and medical equipment for our flight surgeon clinics as well as AE (aeromedical evacuation) onboard our various aircraft. The air wing’s flight surgeon clinics comprise of flight surgeons, flight surgeon assistants, physiotherapists and sports trainers. They provide medical support as family practitioners of our aviators and air traffic controllers as family practitioners and function as aeromedical examiners (AME), as well. Additionally, they support the German AE system as medical directors (MD) onboard our AE-aircraft. Command, support and guidance are provided by Division III, the Competence Centre for Flight Medical Service and the Chief Flight Surgeon of the Air Force.
The GAF operates Eurofighter and Tornado fighter jet aircraft, CH53, AS532 and H145M helicopter, A400M, C130J, A310 MRTT (Multirole Tanker Transport) as well as A319/A321/A340/A350 and Global 5000 aircraft and the Remotely Piloted Air System (RPAS) Heron1.
The Eurofighter wings are stationed at the airfields in Laage, Nörvenich, Wittmund and Neuburg a.d. Donau. In order to provide optimum coverage of German airspace, particularly over coastal and border areas, QRA (Quick reaction alert) units are permanently based at Neuburg a.d. Donau and Wittmund. The wings have been renamed as ‘tactical air force wings’ (TaktLwG) to reflect their multi-role capability, as opposed to the former “fighter” and “fighter bomber” wings.
The reconnaissance units of the Air Force, including its TORNADO aircraft and HALE/MALE UAVs, are concentrated at the Kropp/Jagel airfield in the TaktLwG 51 “Immelmann”. The Tactical Air Force Wing 33 stationed in Büchel retains its previous assignment, equipped with TORNADO aircraft.
The main objective of future air transport involves the fusion of strategic and tactical air transport capacities. The German Air Force will operate up to 53 multi-role A400M Airbus transport aircraft and up to 66 medium-lift CH53 transport helicopters. Because of its central location in Germany and the current framework situation, the main operating base of the A400M is Transport Airwing 62 in Wunstorf, just west bound of Hannover. The CH53 helicopters are combined in a helicopter squadron based at Laupheim and Schönewalde (Holzdorf airfield). Special flight services for the federal government and parliament are provided from Berlin Brandenburg International Airport and Cologne Airport by the Special Air Mission Wing MoD (Flugbereitschaft BMVg).
The aeromedical care of personnel who require a pilot license is provided by the flight surgeons within the wings of the individual military formations. Flight surgeons support flight operations, provide flight safety services and flight physiology training, and are responsible for the aeromedical health of flight crews. They advise their wing commanders and all their superior Air Force officers on matters relating to aviation medicine and general healthcare, and with their specialist medical skills, they contribute to the success of training, exercises and missions of airborne military formations. The Flight Medical Service of the Bundeswehr ensures that the health of flight crews is such that they retain their operational capabilities. Extensive aeromedical support, regular examinations and evaluations of the aptitude, suitability and ability of personnel with regard to their assignments help reduce health-related risk factors among flight crews to a minimum.
The aeromedical support provided also includes preventive inoculation, advice on travel medicine, help in the preparation for and follow-up of missions, rehabilitation measures, the promotion of a healthy lifestyle, and encouragement to participate in sporting activities.
The aim of all aeromedical measures is to establish and maintain the best possible level of operational capacity, flight safety, morale and health among aircrews. They improve individual resistance to stress and optimise performance capacity, enhancing the ability of aircrews to act appropriately in threshold situations and thus providing for sustainable efficiency and in particular safety during flight operations. Flight medicine, as provided by flight surgeons in operational flight units, combines aspects of clinical aeromedicine, flight physiology, flight psychology, physiotherapy, sports, nutritional and occupational medicine with direct experience of flight operations to form an integrated sub-process of health provision within the overall healthcare requirement.
Field Deployments
Flight surgeons in the field / Aeromedical Evacuation
Appropriate and continuous aeromedical support is also an essential factor in successfully maintaining military flight operations at a deployed operating base. Special requirements thus apply with regard to the training, motivation and proficiency of flight surgeons stationed in the field. A deployed flight surgeon must also be capable of acting as an Aeromedical Evacuation Coordinating Officer (AECO), providing the aeromedical expertise required by the casualty evacuation chain.
A flight surgeon must have the abilities required to perform the duties of the Medical Director (MD) in all Tactical Aeromedical Evacuation (TacAE) and Strategic Aeromedical Evacuation (StratAE) missions and, like the civilian senior emergency physician, to coordinate the civilian emergency medical services during airborne evacuation. A Medical Crew Chief (MCC) is at hand to assist the flight surgeon. The Aeromedical Evacuation (AE) flight crew also includes the Medical Device Technician, whose job it is to ensure that onboard medical equipment and material are both functional and safe. The direct medical treatment and monitoring of wounded, injured and sick personnel being transported by aircraft are provided by the specialists of the Bundeswehr Joint Medical Service.
In order to ensure the best possible medical results for the patients in accordance with the fundamental guideline of the Bundeswehr Joint Medical Service, a particular focus is placed on Aeromedical Evacuation as a significant component of the evacuation chain. For this purpose, the German Air Force has a proved and tested system in place, which consists of various kinds of aircraft with different medical equipment, an aeromedical transport command system, and established standard operating procedures. The introduction of the A400M with its enhanced capacity and operational potential represents a significant extension of the spectrum of aircraft that can be used in StratAE and TacAE missions. To provide StratAE worldwide, the German Air Force maintains an A400M with full medical configuration and the corresponding personnel in rapid response status at all times. In 2022 the Airbus A310MRTT will be decommissioned. The multirole transport capacity (passenger and cargo transport, air-to-air refuelling and Aeromedical Evacuation) will be transferred to a multinational unit (Multinational Multirole Transport Tanker Unit (MMU)) operating up to 9 A330MRTT out of Eindhoven, NLD and Cologne, DEU airfield. One of the MMU´s aircraft in AE-configuration uses Cologne as home base. The fleet of the MMU is tasked by the EATC (European Air Transport Command). In its maximum configuration, the A330MRTT is able to carry up to 6 intensive care and 16 intermediate and low care patients.
ARMY


| Surgeon General | Address: | Armed Forces Personnel: |
| Dr med Kai Schlolaut Colonel MC | Army Command Surgeon General of the Army Prötzeler Chaussee 25 15344 Strausberg GERMANY | 60.000 |
Source: Ministry of Defence
The Army Medical Corps
In the year 2000, the personnel of all medical corps of the branches of the armed forces were combined into the Bundeswehr Joint Medical Service. Only smaller subunits in every branch of the armed forces were left, led by their own surgeon generals. The surgeon generals are responsible for health and medical related aspects in view of their branches’ specialties.
Accordingly, the mechanized forces of the Army in the form of two divisions with three brigades each receive medical care on all levels during basic operations and when on assignment by forces of the Joint Medical Service. The mechanized divisions are supplemented by forces of the Rapid Response Forces Division (RRFD). This division controls an Airborne Brigade (Bde) with two parachute assault regiments, one Army Aviation Bde equivalent with two transport helicopter and one attack helicopter Regiment and the Army Special Forces. With the integration of the 11 Airmobile Brigade (11 LMB) NLD into the RRFD as part of the DEU/NLD cooperation, the Division brings together the skills of the German Army and the Royal Netherlands Army (RNA), which are required for a rapid response, air mobility and for the execution of Special and Air Maneuver Operations. Owing to this special requirement profile, the RRFD has its own DEU/NLD airborne and air-mobile medical forces on medical Role 1 level which ensures qualified initial general and emergency medical care during training, exercises and when on assignment. The Division Surgeon RRFD for this purpose is tasked with the responsibility as Medical Advisor for the common DEU/NLD medical support to RRFD operations. The RNA has one Medical Planning Officer within the Division Surgeon’s Office for this purpose.
Army Medical Corps Command Structure
The Surgeon General of the Army commands the Army Medical Corps on behalf of the Army Chief of Staff and the Surgeon General of the Bundeswehr as a specialized service. At the same time, he represents the interests of the Army with respect to the Surgeon General of the Bundeswehr and vice versa.
The Surgeon General of the Army is located in the German Army Headquarters and advises the Army Commanders directly on medical service matters and those relating to the Medical Services of the Army. All Corps and Division Surgeons, the Flight Surgeon of the Army, and the Senior Medical Officer in the Army Training Command work under his command.
Medical Service in Headquarter Staffs
Medical service command and advisory elements (corps, division, brigade surgeons as well as Senior Medical Officers) are provided in the subordinate command authorities, as well as at the division and brigade level. They advise the respective commanders on all medical support matters and are responsible for the planning, control, coordination and monitoring of the measures for ensuring the deployment readiness and support services of the Medical Corps. As Senior Medical Officers, they lead the medical service of the unit, which is technically assigned, to them during deployment. The Division and Brigade Surgeons have an important interface function with the points of contact at the Bundeswehr Joint Medical Service. This ensures that the specific interest and needs of the Army and the Bundeswehr Joint Medical Service are mutually agreed and coordinated.
Medical Service of the Rapid Response Forces Division
The Medical Service of the RRFD works under the command of the Division Surgeon. The Special Operations and Air Maneuver Forces of the Army are located in this division. The potential deployments of the RRFD are characterized in particular by a high degree of mobility, air mobility, a high level of threat, the bridging of large distances with an appropriate distance to their own troops, surprise, speed and secrecy.
The specific characteristics of Army Special Operations and Air Maneuver Forces training, exercise and deployment are considered in medical services support, so that in the two paratrooper regiments of the Airborne Brigade and in the SOF their own medical personnel are organically deployed to support the troops.
The two independent Airborne Medical Companies of the Paratrooper Regiments are commanded by Medical Staff Officers. They each have an airborne patient treatment platoon, two airborne rescue platoons and their own Patient Evacuation Coordination Cell (PECC). The ability to parachute jump is an essential precondition in order to be able to follow without restriction the parachute regiments, which are to be supported in all deployment types/options. For this reason, both Airborne Medical Companies are fully capable of parachute jumping.
The SOF provides personnel to carry out special operations such as hostage release operations (HRO). As a rule, such operations are carried out under conditions where it is not possible to rely on the existing medical infrastructure of the country in which the deployment is performed. The structure of medical service support in the SOF considers these framework conditions. In the SOF staff unit, there is a Medical Services Branch under the command of the SOF Command Surgeon. This branch ensures not only the provision of advice to the leadership of the unit but also the detailed planning of medical service support for special operations and the technical management of the organic medical personnel of the SOF. The SOF has a medical clinic, which ensures not only medical care during peacetime operations, but also the provision of medical support for a wide range of deployment options up to Role 1 level during training and exercises.
Deployments of the Special Operations Forces (SOF) of the Army receive medical support from air-mobile emergency physician teams and air-mobile medical teams, as well as air-transportable Role 1 facilities. An Air-Mobile Emergency Physician Team of the SOF consists of two Special Forces Senior NCO paramedics, a SOF emergency physician, and a driver. The Special Forces Senior NCO paramedics are fully trained as both commandos and paramedics. The SOF emergency physician is a Medical (Staff) Officer who is specialized in emergency medicine and SOF-specific infantry and other medical service training.
The option of being ready for deployment in special operations is only made possible by the broad and in-depth training of everyone involved. The forces providing medical care must be aware of the effects of excessive heat in the desert, tropical conditions or extremely low temperatures in Arctic latitudes in the same way as they are acquainted with the clinical pictures and specific features of the respective climate zones.
The Aeromedical Service of the Army
The Aeromedical Service of the Army Aviation is under the command of the Flight Surgeon of the Army, who is integrated into the Army Aviation Command within the Rapid Reaction Forces Deployment (RRFD).
His main tasks include the aeromedical care for Flight Operations and Army Aviation Training Facilities at their home bases, during training missions and deployments, the aeromedical advice to the Army Aviation Commanders and the planning and organization of the Flight Accident Emergency Medical Services during Flight Operations.
To fulfil these main tasks, Flight Surgeon Groups are integrated into the three Army Aviation Regiments of the RRFD, the International Helicopter Training Centre and the Air Mobile Training Centre.
To guarantee the continuous qualified medical rescue measures in case of Flight Accidents and Incidents, the three Army Aviation Regiments have their own integrated Flight Accident Emergency Medical Groups, trained in special rescue measures relating to their aircraft type.
Army Training Facilities
The Army Training Command leads the training facilities of the Army. The Command Surgeon of the Army Training Command is responsible for the continuing advanced and further training of the medical services as well as the medical personnel at the Army training facilities.
At the training facilities, the next generation of commanders receives extensive theoretical and practical training in the integration of medical service personnel and resources into the conduct of operations – from the group to brigade level. Furthermore, defined personnel receive special medical and paramedical training. Here, mutual understanding and knowledge of one another are particularly important. Medical service training by qualified instructors is therefore integrated into all training facilities. The priorities in medical service training are set at the Army Officers' Academy, the NCO School of the Army and the Army Combat Training Centre. The Specialized Operations Training Centre represents the training facility of the Special Operations and Specialized Forces of the Army. Against the background of the particular tactical framework conditions in Special Operations, the ability of the deployed soldiers to provide extended self-and buddy-aid at a highly specific level is indispensable. Therefore, the forces of the Army used in Special and Specialized Operations are trained as “Combat First Responders (CFR)” on qualification levels A to C. The defining feature of this special training is the embedding of emergency medicine aspects in the deployment principles and methods of the Special Operations and Specialized Forces.
Military Experts on Mission, OSCE observers and UN observers, civilian specialists (NGOs), as well as journalists or chemical weapons inspectors, also receive training in advanced self-aid and buddy care at the Training Centre of the Bundeswehr for the United Nations.
The Pack Animal Centre belongs to the 23rd Mountain Infantry Brigade and is commanded by a Veterinarian Staff Officer. It supports the Mountain Infantry Brigade and other military units in all conflict scenarios in difficult to extreme or difficult to access terrain, including high altitudes and extreme climatic and weather conditions, with its mountain pack and riding animals, which are capable of carrying out transport and delivery tasks. During deployments and basic operations, it ensures the veterinary care of the animals and their correct shoeing.
Summary
The concentration of the medical services in one Bundeswehr Joint Medical Service has brought with it a significant improvement in the quality of medical service care and made it possible to guarantee such medical support during operations over the last few years. At the same time, it has provided the Army with room to develop a highly specialized Role 1 medical support for the Special Operations and Specialized Forces.
In addition to the further improvement of the quality of care, the focus in the future will be in medical support within the Collective Defense. The increasing demands placed on mobility with simultaneous protection during the assignments of Airborne/SOF and regular Army Ground Forces with the view towards NATO defense planning has to be considered in order to continue the high-quality medical care for the Special Operations, Specialized Forces and regular Army Ground Force wherever their assignment takes them.
JOINT SUPPORT AND ENABLING SERVICE

| Surgeon General | Address: | Armed Forces Personnel: |
| Dr med Johannes A. Grohmann Colonel MC | Kommando Streitkraeftebasis Fontainengraben 150 53123 Bonn Germany | 31.100 |
Source: Ministry of Defence
The Medical Service in the Joint Support and Enabling Service
The Joint Support and Enabling Service
The most important factor behind the development of the new structured Joint Support and Enabling Service (JSES) was the orientation towards providing a wide range of capabilities for operations. The previous structure with its broad spectrum of capabilities was thus converted into capability coordination commands:
Logistics Command of the Bundeswehr
Military Police Command of the Bundeswehr
CBRN Defence Command of the Bundeswehr
Territorial Tasks Command of the Bundeswehr
MN Joint Headquarters Ulm
Joint Support and Enabling Command (JSEC) and the
Armed Forces Office
with their respective subordinated commands and agencies.
Technical and administrative responsibility as well as training authority are brought together.
The following diagram of the JSES can only provide a rough outline of the tasks and responsibilities of the Service. A detailed illustration would exceed the scope of a compendium such as this. This is why the tasks of the medical elements within the JSES are not specifically outlined.
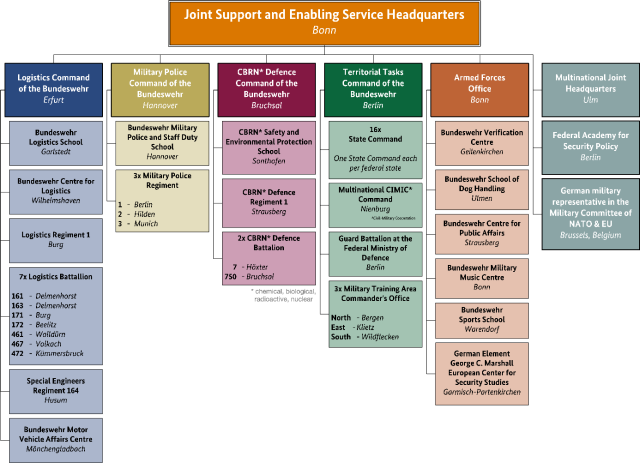
Fig. 1: Structure of the Joint Support and Enabling Service Source: Ministry of Defence
The Medical Service in the Joint Support and Enabling Service
The Medical Service in the JSES provides specialist advice for force commanders, performs military pharmaceutical tasks for the Bundeswehr, and fulfills specific specialist tasks. The JSES further ensures the provision of medical care at Bundeswehr agencies abroad (outside of military operations).
Senior Medical Officers (SMOs) in capability coordination commands serve as medical advisors to force commanders. In addition, they analyse physical and ergonomic requirement profiles for various specialist tasks and contribute medical expertise to the further development of technology and procedures. These tasks are especially important with respect to future personnel development.
The Surgeon General of the Joint Support and Enabling Service, the Bundeswehr Logistics Centre, and medical materiel depots perform military pharmaceutical tasks. Military pharmacy elements have in-service, maintenance and supply responsibility for medical materiel in the JSES. They furthermore represent the interests and technical issues of medical materiel management in the further development of logistic systems at the interface to the main logistics process.
A broad range of specific specialist tasks are performed in national and international HQs, authorities, commands and agencies and are carried out by medical advisors, special instructors at schools, veterinarians for working dogs, and toxicologists in the CBRN corps.
Surgeon General of the Joint Support and Enabling Service / Senior Medical Officer of the Joint Support and Enabling Service
The Subdivision of the Surgeon General of the Joint Support and Enabling Service controls and coordinates health support and medical materiel logistics in the JSES.
The responsibilities of the Surgeon General include:
- assessing medical operational readiness in his area of responsibility,
- providing expert advice to the Chief of Staff of the Joint Support and Enabling Service and the Surgeon General of the Bundeswehr in all medical matters of the JSES,
- assuming in-service and supply responsibility for medical materiel in his area of responsibility,
- exercising functional control over subordinate medical elements and
- providing intermediary or final reports for decision-making processes.
The Chief of the Division of the Surgeon General of the Joint Support and Enabling Service is the technical superior of the Medical Service and in charge of the subdivision of the same name in the Command and Control Directorate of the JSES HQ. He also acts as Senior Medical Officer of the JSES and represents the respective interests in matters of health support and medical materiel logistics. The Surgeon General of the Bundeswehr is his direct technical superior.
The Military Medicine and Military Pharmacy branches provide specialist medical expertise for the mission of the JSES.
Their tasks include:
- processing, reviewing and co-signing national and international documents, concepts, directives, decrees and service publications containing medical matters,
- ensuring that medical personnel of the JSES receive training and education that is appropriate to their posting,
- monitoring and ensuring medical operational readiness in the JSES,
- analysing and evaluating all guidelines and policy documents with regard to medical relevance,
- implementing requirements of the Surgeon General of the Bundeswehr for the JSES and
- representing the interests of the JSES in medical working groups, committees and study groups (e.g. CIMIC, optimization of assessment systems, organisational health management, evaluation of pre-/post-deployment activities, PTSD, integrated project teams, etc.).
Based upon a service level agreement, the Division of the Surgeon General of the JSES provides all its specialist medical expertise also to the recently established branch of the Cyber and Information Domain Service.
Military Medicine Branch
The Military Medicine Branch evaluates findings in the fields of preventive health protection, ergonomics and man-machine interaction with regard to their military medical relevance and integrates them into the further development of technologies and procedures used in health support. Furthermore, the Military Medicine Branch secures the implementation and further development of the Occupational Health Management in the JSES and the Cyber and Information Domain Service.
Military Pharmacy Branch
The Military Pharmacy Branch has in-service and supply responsibility for medical materiel as well as functional control of medical materiel management in the JSES. The main tasks cover three key areas.
As part of the in-service and supply responsibility with regard to medical materiel, military pharmacy ensures the material readiness of medical facilities in the area of responsibility of the Chief of Staff of the Joint Support and Enabling Service. By also fulfilling this task for the major organisational element Personnel, the JSES emphasizes its role as a service provider for all major organisational elements. The JSES is also the central service provider for all agencies of the Bundeswehr with regard to the provision of medical materiel. Centrally procured medical materiel is managed and kept “ready to use” in medical materiel depots. The maintenance control of Bundeswehr medical materiel also takes place in the JSES, under the responsibility of the Military Pharmacy Branch.
In addition, the Military Pharmacy Branch represents the interests of the JSES to the main process manager for logistics in matters related to the management and maintenance of medical materiel.
This branch also acts as Authorized Representative of the Chief of Staff of the Joint Support and Enabling Service for military medical projects in the Integrated Planning Process and establishes medical materiel investment and running cost requirements for the financial requirements analysis and medium-term financial planning.
The Senior Medical Officer (SMO) of the Armed Forces Office
The Senior Medical Officer of the Armed Forces Office could be considered the unit physician with the largest area of responsibility in a geographical sense. He is responsible for the medical care of all German soldiers stationed abroad outside of military operations. This includes all medical advice, especially with regard to travel medicine, the implementation of vaccination programs, the supply of pharmaceutical products, and medical assessments. Of course, he also provides advice and support if family members, for example of a military adviser in Central Africa, experience medical problems.
The Senior Medical Officer is under the administrative control of the Chief of Staff of the Armed Forces Office and under the technical control of the Surgeon General of the Joint Support Service. He organizes and leads the medical service of his command area. He advises the Commander of the Armed Forces Office, heads of agencies in his command area in Germany and abroad, German military attachés, heads of Bundeswehr agencies abroad as well as heads of the German Military Advisory Groups in Africa and Asia on all matters related to the medical service.
He has technical control over the following medical areas:
- unit physician at Supreme Headquarters Allied Powers in Europe (SHAPE) in Mons, Belgium;
- unit physician of the German element of the Joint Forces Headquarters in Brunssum, Netherlands;
- medical sergeants of German elements of NATO staffs in Fontainebleau, France; Naples, Italy; Innsworth GBR, Lisbon, Portugal; JFC HQ Brunssum, Netherlands and Izmir, Turkey, as well as at the German Armed Forces Command, United States and Canada in Reston, USA
- Commander, Bundeswehr School of Dog Handling, Ulmen.
SMO / CJMed Division of the Multinational Joint Headquarters
In 2013, the Response Forces Operations Command in Ulm was transformed into the Multinational Joint Headquarters (MN JHQ) Ulm.
This new command is a multinational joint headquarters at the operational level. Its capability to lead both EU and NATO operations is unique. It leads from the theatre of operations and must therefore be quickly deployable to any place in the world.
The headquarters comprises approximately 400 German and multinational soldiers and civilian personnel and is able to lead multinational joint operations of NATO and the EU up to an overall strength of 50,000 soldiers. It is particularly qualified to work closely together with civilian partners, such as the European External Action Service, host countries, international organisations such as the Red Cross and relief organisations (comprehensive approach).
The MN JHQ Ulm staff therefore includes elements such as Intelligence and Knowledge Development, Strategic Communications, and an Operational Competence Centre. In addition, the MN JHQ Ulm provides key personnel for a German-led EU headquarters at the military-strategic level.
The Combined Joint Medical (CJMed) Division plans and coordinates multinational medical care for each operation. Personnel of this division are closely involved in the operational planning process in all relevant bodies.
Medical support also includes force health protection, medical logistics, and medical intelligence. A key task is implementing the comprehensive approach, in other words in-theatre medical civil-military co-operation with governmental, international and non-governmental organisations.
A patient evacuation coordination centre (PECC) staffed mainly by CJMed personnel coordinates patient evacuation at the operational level.
In addition, CJMed contributes to further medical development and medical operations analysis at the multinational and national level. The CJMed Division is also extensively involved in the planning, execution and follow-up analysis of multinational pre-deployment and certification exercises.
The Chief of CJMed Division is the SMO of the command area during routine operations. At the same time, he is the medical director of each overall operation and acts as a multinational technical superior to all medical forces participating in the operation and as a medical advisor to the force commander.
Bundeswehr School of Dog Handling
The Bundeswehr School of Dog Handling in Ulmen is headed by a veterinarian and provides the Joint Support and Enabling Service with a very special capability from the wide range of Medical Service capabilities. Starting from their recruitment until the end of their service, working dogs of the Bundeswehr receive veterinary care in Ulmen to ensure their fitness for their main tasks of protection and guard duty, searching for missing persons, detecting drugs and explosives, and mine detection. This includes a reach back procedure for the treatment of illnesses and injuries the animals may suffer on operations.
The recruitment of the dogs is realized by buying young adult dogs on the European market but the main number of the working dogs is provided by the own military breeding of Belgian Shepherds and in smaller numbers German Shepherds. Following its selection and training, a working dog is handed over to its handler, who will work with this dog until it reaches approximately 8 years of age. With the help of modern technology, the training of dogs and their capabilities are continuously optimised and developed. Time and again dogs have been found to be clearly superior to other sensors.
The school's veterinary clinic is equipped with modern medical technology. This means that even major surgical procedures can be performed there. Since 2011, a documentation system for veterinary data is available at the clinic.
The school also ensures that four-legged pensioners and veterans receive lifelong care. If they cannot stay with their handlers' families or be placed with someone else, they remain in Ulmen, spending their sunset years with a pack and housed in modern kennels.
Bundeswehr Logistics Command
The Bundeswehr Logistics Command in Erfurt and the Bundeswehr Logistics Centre, which has direct authority over fixed logistic installations, follow the capability-oriented approach of the JSES. This means that joint technical and administrative control of medical materiel depots lies directly with the Bundeswehr Logistics Centre. The group for the technical supervision of military pharmacy in the Bundeswehr Logistics Centre and its military and civilian personnel are the central point of contact and control agency for ensuring the provision of medical materiel by the JSES. Medical materiel is provided by the medical materiel depots in Epe and Krugau, which also have the status of Bundeswehr pharmacies.
In addition to materiel requirements and stock management for centrally procured medical materiel, the central maintenance control point for medical materiel is also part of the Bundeswehr Logistics Centre. It is responsible for planning, controlling and coordinating the maintenance of medical equipment throughout the Bundeswehr. It also acts as an interface between different units and military and civilian maintenance facilities across all major organisational elements.
As a unique ability, the medical materiel depot in Krugau has a center of excellence for the inspection and maintenance of modular medical units containers. This has reduced the pressure on supply facilities for medical materiel of the Bundeswehr Medical Service.
Bundeswehr CBRN Defence Command and Bundeswehr Military Police Command
The Bundeswehr CBRN Defense Command and the Bundeswehr Military Police Command do not have an on-site SMO. Their medical tasks are administrated by the Military Medicine Branch within the JSES HQ.
Bundeswehr Territorial Command
The Senior Medical Officer (SMO) of The Bundeswehr Territorial Command (BwTerrCOM) advises the commander in all medical matters. The BwTerrCOM is the German OpsCommand for inner German operations. Territorial tasks mainly include:
- Host Nation Support,
- Mediator between civilian and military authorities following the civilian administration structure and according to the levels of cooperation,
- inter-agency assistance/disaster relief at home and functional leading element of military training areas.
- Responsibiliy for the territorial reserve e.g.Regional Security and Support Companies to support regional home defense capability.
Joint Support and Enabling Command
The Joint Support and Enabling Command (JSEC), being under SACEUR`s operational command, is the NATO Command and Control (C2) entity on operational level for the Rear Area and supports Host Nations (HNs) in planning, execution & coordination of Security, Force Protection and Area Damage Control. JSEC furthermore enables Training and Integration (RSOM-I) of NATO Follow-on-Forces. Last, JSEC conducts security operations and Force protection operations in support and on request of the HNs.
At 1 April 2019 JSEC was build up in ULM as a new entity and part of the NATO Force Structure. Next milestones are Initial Operating Capability (IOC) scheduled for 1 October 2019 and the Full Operating Capability (FOC) scheduled for 1 October 2021.
JSEC Medical Service
JSEC Medical Service (MedServ) is NATOs operational-level responsible entity in coordinating medical-related matters in the Rear Area (RA). MedServ identifies requirements for the whole range of upcoming tasks from Baseline Activities and Current Operations (BACO) up to Maximum Level of Effort (MLE) within the own Area of Responsibility (AoR).
The tasks are, to plan, direct, co-ordinate and assess the joint medical support for transiting and assigned forces, assigned operations and contingencies including command, control, communication and information (C3I) structures for an integrated system of treatment, medical evacuation and medical supplies, force health protection and reporting.
Furthermore, JSEC MedServ contributes in all medical and medical-related matters to the development of joint medical plans, situational awareness, procedures, policies and doctrine. A core basis for this is the establishment of a recognized medical picture already in BACO and maintained and expanded in Crisis and MLE.
Essential in the RA is a functional network and active relationship with all relevant entities in the AoR including the Host Nation (HN) to establish and provide comprehensive and high-level Medical Support. In a coordinating function, JSEC MedServ de-conflicts and harmonizes national and alliance medical support plans from a Rear Area perspective and supports bi- or multinational medical support solutions and arrangements.
MedServ is able to cover the three sectors medical planning, medical operations and medical Logistics / Force Health Protection. Staffed with national and multi-national members, the Peacetime Manning Requirements include additionally dual-hatted posts from Multinational Joint Headquarters ULM (CJMed).
Summary
Medical tasks are only one part of the support activities carried out by the JSES for the Bundeswehr. The Medical Service in the Joint Support and Enabling Service supports units of the JSES by providing advice on all medical issues and by contributing expertise to further development. The Medical Service also provides the Bundeswehr with special medical, pharmaceutical and veterinary capabilities that only exist within the JSES. The Medical Service in the JSES has been optimised in the new structure in order to fulfil its functions. It will continue to be developed based on lessons learned.
NAVY


| Surgeon General | Address: | Armed Forces Personnel: |
| Dr med Stephan Apel Rear Admiral (lh) MC | Navy HQ Kopernikusstr. 1 18057 Rostock GERMANY | 14.012 |
Source: Ministry of Defence
Basic Task of the Military Medical Service
The Medical Service of the German Navy ensures medical care for all seagoing and flying units of the fleet, deployed or in port, including the Navy´s special and specialized forces, using the very latest in medical technology and procedures. It protects, maintains and restores the health of soldiers.
Structure
The Navy medical Service is headed by the Surgeon General of the German Navy. He is head of the Navy Medical Service Directorate, is a member of the German Navy Headquarters Board, and is the Medical Advisor of the Chief of German Navy.

The Commander Operations is also the head of Operation Directorate. Same is true for the Surgeon General of the NAVY who is head of the Navy Medical Service and the Commander Support who is also head of the Logistic and CIS Directorate.
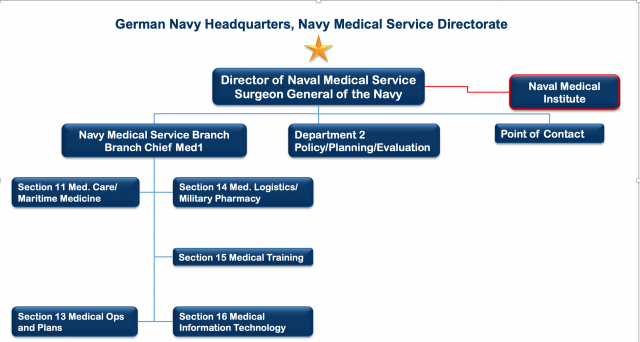
Source both graphics: Ministry of Defence
The Navy Medical Service provides health support for Navy operations and training ashore and afloat. The Navy Medical Service works closely together with the Bundeswehr Joint Medical Service to provide primary surgery and dental care during Navy operations and training afloat.
Institutes
The Naval Medical Institute covers covers the entire field of maritime medicine. This institution is located in Kiel and is directly subordinate to the Surgeon General of the German Navy. It is also collocated with other institutions of the Bundeswehr Joint Medical Service. It is the “alma mater” of all German medical officers of the Navy and directly supports the Navy through research and education. After the reorientation of the Medical Service, all Navy-related responsibilities were given to the Naval Medical Institute, which remains the land-based centre of excellence within the Navy. The Institute covers the entire range of scientific, research, care-providing, preventive and teaching facilities. Due to the increasing importance of departmental research, it was divided into three sections:
Maritime Medicine, Diving and Hyperbaric Medicine, and Research and Education.
The Institute of Naval Medicine
- provides medical care in the event of hyperbaric accidents
- provides mission-specific medical education to personnel on board
- provides threat-related medical expertise
- provides medical appraisal and research
Also pharmacists who are registered food chemists and dentists are part of the Navy Medical Service.
Deployments Afloat
The medical capabilities of deployed Navy units vary strongly and depend on the platform and the embarked personnel. All levels of medical care can be provided, ranging from two Role 2 naval rescue centres (NRC), in which several medical teams perform primary surgery within clinical timelines on a combat support ship, to surgeons and anaesthesiologists embarked on frigates, to shipboard physicians or highly trained ship’s paramedics performing pre-hospital emergency care.
Role 1 is performed at sea on every unit. At this level, a well-trained paramedic is responsible for skilled first aid and diving medical support for all divers on board. This minimum level is also provided on submarines and mine-hunting vessels. All hunting vessels have a decompression
chamber for treating diving accidents.
Different medical kits are available depending on operational needs, the number of soldiers, and the expected numbers of casualties. These kits include appropriate sets of drugs and dressing material, defibrillators, monitors, respirators as well as rescue equipment such as stretchers, transport hammocks and vacuum mattresses.
All other units have their own ship hospital. These units have shipboard physicians and two paramedics. In addition to the minimum equipment found on boats, ship hospitals also have laboratory equipment (blood count, clinical chemistry and enzymes), ultrasonic diagnostic equipment, and basic surgical equipment.
Frigates are also equipped with an anaesthetic machine, an X-ray device, and surgical material for damage control surgery. They have a limited holding capacity. On deployments, frigates receive a DCS team.
On combat support ships, a Role 2 naval rescue centre (NRC) can be activated and made operational within about one week. Activated to the highest configuration, it serves as a Role 2 Enhanced afloat. It offers 34 beds (plus 9 in the ship´s own hospital) and 5 ICU beds (plus 1). There are no Role 3 or higher facilities afloat in the German Navy.
Dental care is provided on frigates, combat support ships, and support ships (tenders). Ship hospitals can be equipped with mobile dentist material. Combat support ships have an integrated dental centre.
The Navy has MK 88A Sea Lynx and MK 41 Sea King helicopters. For some deployments, frigates embark two MK 88A, whereas combat supply ships have two MK 41. These helicopters can also be equipped with medical kits. In its current configuration, the MK 41 is able to carry 1 ICU litter patient and six patients with minor injuries. An MK 88A has space for one litter patient or 5 seated patients with minor injuries.These helicopters will be replaced soon by sea tiger and sea lion.
The German Navy cooperates closely with medical services ashore and afloat of all combined forces and relies on host nation support in all deployments and missions.
(status: 23th June 2025)











