
Almanac
Netherlands, Kingdom of the



Surgeon General
Jelle A.H. Bos, MD, PhD
Surgeon Commodore
Source: Ministry of Defence Netherlands
NLD Military Health Service Directorate
P.O. BOX 20701
MPC 58B
2500 ES, The Hague
THE NETHERLANDS
Contact Details for Public Affairs:
Phone: +31 (0)70 318 8188
Email: [email protected]
Pictures and Graphics: Wikimedia Commons
History
The history of military healthcare in the Dutch armed forces traces back to 1815 when King William I appointed Professor S.J. Brugmans to organize medical supply depots and establish training schools for military doctors. By 1869, the Regiment Geneeskundige Troepen was founded within the Army, providing medical support in key conflicts like the Franco-Prussian War (1870-1871) and later during both World Wars.
The Navy, by the mid-19th century, had its own medical corps, focusing on the unique health challenges of sailors on long sea voyages and in distant colonies, including vaccination programs against smallpox. The Air Force established its medical services after its creation in 1913, with a focus on aviation medicine, addressing issues like altitude sickness and hypoxia.
Throughout the 20th century, especially during the Korean War (1950-1953) and various UN peacekeeping missions in the Balkans and Afghanistan, military medical services became more coordinated. In 1991, the Military Health Care (MHC) was created to unify medical efforts across all branches.
Today, military healthcare includes field hospitals, medical evacuation capabilities, and specialized trauma care, playing a vital role in both national defense and international peacekeeping.
NATIONAL CONTEXT AND SUMMARY
Netherlands: Overview and Geostrategic Position
Geographically, the Netherlands covers an area of approximately 41,500 square kilometers, making it one of the smaller countries in Europe. Bordered by the North Sea to the northwest, Germany to the east, and Belgium to the south, it is strategically located within the heart of Western Europe.
The country has a population of about 18 million, with the majority living in urban areas, particularly in the western provinces known as the Randstad, which includes major cities such as Amsterdam, Rotterdam, The Hague, and Utrecht. The Netherlands has a long history of peaceful relations with neighboring countries and is a founding member of several international organizations, including NATO and the European Union.
Organization of the Ministry of Defence and Armed Forces
The King of the Netherlands serves in a ceremonial role for the Dutch Armed Forces, unlike most other Monarchies the King does not serve as a Commander-in Chief. The Ministry of Defence is led by the Minister of Defence, a member of the Cabinet. The Chief of Defence is the highest-ranking military officer and oversees the operational command of the armed forces. Each position has distinct responsibilities:
The Minister of Defence manages all aspects of national defense policy, resource allocation, and military operations.
The Chief of Defence is responsible for military strategy, command structure, and advising the government on defence matters.
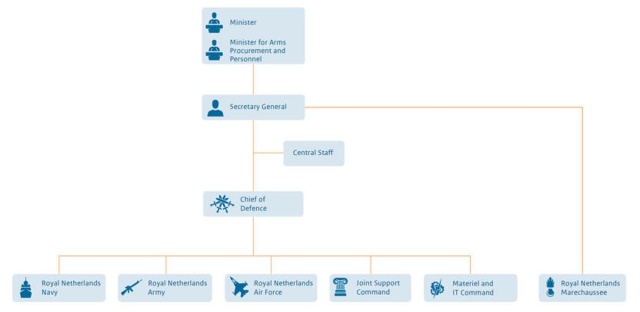
Figure 1: organization chart of the Ministry of Defence source: Ministry of Defence Netherlands
National Health System
The organization of the Dutch healthcare system is primarily governed by the Dutch Constitution, which delineates responsibilities among the national government, municipalities, and regional health authorities. The national government oversees public health policy, while municipalities are responsible for local health services. The Dutch Health Insurance Act mandates basic health coverage for all residents, ensuring access to a wide range of medical services, including primary care, specialist treatment, and hospital care.
Public health responsibilities, which encompass areas such as disease prevention, health education, and sanitation, are shared among various levels of government. Municipalities typically manage local public health initiatives, while regional health authorities coordinate healthcare delivery and services.
Dutch Military Health Service
The Surgeon-General of the Armed Forces is the responsible military health authority and oversees the military healthcare organization as the Director of the NLD Military Health Service Directorate. The military healthcare organization is providing comprehensive healthcare to military personnel, including medical, dental, and mental health services. Members of the armed forces are primarily covered by the dedicated military healthcare framework and do only use the national healthcare system in extremis.
The military healthcare organization operates medical facilities staffed by military healthcare providers, ensuring that active service members receive the necessary care. In cases where care cannot be provided within military facilities, service members may be referred to civilian healthcare providers.
Organizational Structure
Centrally Positioned Healthcare Elements
The Defence Healthcare Organisation (DHO) is responsible for providing healthcare services across all branches of the Netherlands Armed Forces, both domestically and internationally. With approximately 1,350 personnel, the DHO delivers a wide range of services, including first-line healthcare, dental care, hospital capabilities, rehabilitation, blood provision, clinical specialist teams for deployment, medical logistics, and initial medical education. The organisation is led by the Commander of the Defence Healthcare Organisation.
Operational Role 1 and Role 2 medical assets are decentralized and fall under the command of the individual domains: the Navy, Army and Air & Space Force.
Operational Military Healthcare
The Royal Netherlands Navy is equipped with maritime medical capabilities for Role 1 and Role 2 care on its vessels. The Navy’s Role 2 facilities, particularly for the three Joint Support Ships, are staffed and equipped by the dedicated Single Service Management unit 400 Medical Battalion (MedBn) and the surgical teams from the Defence Healthcare Organisation. The Royal Marine Corps has Role 1 capabilities for amphibious operations, supported by land-based Role 2 support from 400 MedBn. The Navy’s medical branch is led by the Navy Surgeon General, and the Navy medical services employ approximately 120 personnel.
The Royal Netherlands Army integrates medical personnel into its three brigades (11 AirMobile Bde, 43 Mechanized Bde, and 13 Light Bde), each of which has its own medical company with Role 1 assets. Role 2 assets, however, are centralized within the 400 MedBn under the Land Operations Support Command. The 400 MedBn is capable of deploying Role 2 facilities to support sustained operations or high-threat missions for any of the armed forces branches, including Role 2 afloat support for the Navy. This battalion can also provide personnel to augment medical task forces, Medcells, and Patient Evacuation Coordination Cells. The Medical Command is a staff unit under the Land Operations Support Command, responsible for the readiness of all land medical forces. The Army Surgeon General at Army Headquarters oversees the medical branch with a total personnel strength of approximately 1,100.

Figure 2: Role 2 hospital of the 400 Medical Battalion source: Ministry of Defence Netherlands
The Royal Netherlands Air & Space Force maintains aviation medical capabilities focused on AEROMEDEVAC, supporting deployable units with casualty station capacity at their Casualty Staging Units. The Air Force’s medical branch is headed by the Air Force Surgeon General, with approximately 140 medical personnel in total.
The Royal Netherlands Marechaussee (Military Police) has a dedicated medical branch headed by the Marechaussee Surgeon General. While some medical personnel support military police operations directly, the Marechaussee is largely supported by the medical services of other domains with which they are deployed.
Military Hospital
The Central Military Hospital (CMH) in Utrecht is the primary facility for military inpatient and outpatient care, with a capacity of 30 beds. The CMH works closely with the neighboring University Hospital Utrecht, and is able to expand its capabilities to manage major incidents through a 200-bed (sheltered) facility that can be operational within 30 minutes, including quarantine capabilities. This setup provides a unique and rapid-response medical facility for major incidents and disaster relief in the Netherlands.

Figure 3: Exercise National Disaster Hospital source: Ministry of Defence Netherlands
The Military Rehabilitation Centre in Doorn provides rehabilitation services with a capacity of 80 inpatient beds, plus outpatient care. This facility also serves civilian patients and has advanced training and orthopedic workshop capabilities.
Institutes
The Coordination Centre for Expertise on Working Conditions & Health provides expert guidance on occupational health, safety, and environment, supporting the Surgeon General and military healthcare with a focus on operational readiness and deployment. This includes occupational health services and training for occupational health physicians.
The Centre for Human and Aviation is responsible for aeromedical and psychological evaluations, testing, training of aircrew, and research in human factors.
The Diving Medical Centre conducts medical assessments, training, and treatment for diving personnel, including decompression sickness treatment and hyperbaric medicine research.
The Sports and Training Medical Centre offers physical examinations and applied research on exercise and field physical demands, advising on physical stress management for soldiers.
The Defence Healthcare Education and Training Centre provides foundational and specialized military medical education and training. This institute focuses on military-specific healthcare applications and serves as a medical center of excellence.
The Institute for Defence and Partnership Hospitals is a unique component, collaborating with civilian hospitals to enhance surgical capacity. This program ensures that civilian medical personnel with reserve military status can support military needs through pre-planned deployments, training, and contracting.
Military Medical Research and Innovation
The Netherlands Defence Healthcare Organisation (DHO) conducts vital research to address the health and operational needs of military personnel through collaboration with research entities such as the Netherlands Organisation for Applied Scientific Research (TNO), Dutch universities, industry, Hospitals, allied military health organizations, and various government bodies. The research focuses on military-relevant topics that support the development of evidence-based practices, improve health care for personnel, and enhance operational decision-making.
The DHO actively participates in international research initiatives, which ensures the Dutch Armed Forces benefit from the latest medical innovations and healthcare practices. These collaborations include engagement with NATO’s Science and Technology Organization, where Dutch representatives contribute to committees and Research Task Groups related to health, medicine, and protection. The Netherlands also participates in technical panels within The Technical Cooperation Program on Military Medicine.
Research priorities for the DHO include:
These research priorities help the DHO proactively address both ongoing and emerging health challenges, contributing to the overall resilience and operational readiness of Dutch Armed Forces personnel.
The research priorities are included in the following core themes:
- Force health protection and enhancement for the purpose of preparing the individual soldier
- Increasing deployability under operational conditions
- Trauma care under operational conditions
- Data-driven health interventions
- Moral-ethical frameworks of human performance optimization and enhancement
- autonomous operational medical (logistics) chain
Does the military have any standing domestic and international tasks or operations? (last 20 years)
| 2004-2005 | SFIR Iraq: Role 1 and Role 2 deployment; North Afghanistan Pol-E-Khomri: Role 2 deployment; |
| 2006 | NRF 5 Pakistan: Role 2 for humanitarian assistance; |
| 2006 | Exercise RECAMP Cameroon Africa: medical assistance programme; |
| 2006-2010 | ISAF South Afghanistan Uruzgan: Role 1 and Role 2 deployment; |
| 2006-2010 | ISAF South Afghanistan: Aeromedevac and holding capabilities; |
| 2006-2011 | ISAF South Afghanistan Kandahar: Role 3 specialist team; |
| 2007-2011 | KFOR: Role 3 specialist team; |
| 2012 | Kunduz: Role 1 and contribution with a Role 2 medical team; |
| 2012-2014 | Afghanistan Kunduz: Role 1 and contributions with a Role 2 medical team; |
| 2013-2014 | BMDTF (Patriot) Turkey: Role 1 MTF; |
| 2014-2019 | MINUSMA Mali: Role 1 MTF and Aero Medevac; |
| 2014 | MH-17 (UKR): deployment of Role 1 MTF, Role 2 MTF and identification teams; |
| 2015-2021 | Resolute Support Afghanistan, Role 1 MTF and Role 2 medical team; |
| 2016 | Ocean Shield, European border patrol: integrated Role 1 assets; |
| 2016- 2025 | CBMI: training support mission IRAQ mission, R1 MTF; |
| 2016- ongoing | Enhanced Forward Presence (eFP) Baltic States: integrated Role 1 assets; |
| 2024 | ASPIDES: Role2E Afloat in Red Sea |
| Ongoing | Numerous ongoing missions with a small tailor-made medical footprint |
Source: Ministry of Defence Netherlands
In addition, medical services support various exercises throughout the world.
How are new medical equipment or capabilities procured?
The procurement of new medical equipment in the Dutch military healthcare system involves a collaborative process among several key organizations. It begins with the Medical Service, which assesses medical needs and identifies gaps in capabilities. The Command Materiel and IT then allocates the budget based on these requirements and issues a request for proposal to potential suppliers.
The Military Health Logistics Center (MGLC) manages logistics, ensuring timely delivery. The Defence Healthcare Training and Education Centre takes care of implementing the new materials in the training of personnel.
How are medical logistics organized and managed during operations?
The MGLC supports the Military Medical Care in taking care of a well-functioning and ready military. It supports the different operational commands in the buy in, delivery, storage, transport and control of the supplies.
Describe innovations or lessons from the experience of providing military medical support on operations.
The use of deep-frozen blood products, particularly platelets stored at -80°C, has proven both safe and effective in managing trauma-related hemorrhage, especially within military contexts. The Netherlands Armed Forces have utilized these deep-frozen thrombocyte concentrates since 2001 to treat massive bleeding in combat and austere settings, where logistical constraints make it difficult to rely on conventional room temperature-stored platelets (RSPs). The deep-freeze approach enables extended storage times of up to 4 years, significantly reducing waste from product expiration and allowing for transport over long distances without compromising product quality. Retrospective analyses and preclinical studies have shown that deep-frozen platelets are effective in supporting haemostasias. For instance, trauma-induced hemorrhage models suggest that these frozen products can be as effective as RSPs in stabilizing patients, without increasing the risk of adverse reactions. Additionally, the deep-freezing process may activate platelets in ways that could enhance their clot-forming abilities in specific situations, despite showing some differences in in vitro tests compared to fresh platelets.
However, this storage method could be logistically transformative, as it reduces reliance on freshly collected products and "walking blood banks" in remote or emergency settings.
MILITARY MEDICAL PERSONNEL
In the Netherlands, military medical recruitment and training for the Dutch Armed Forces are managed through a structured process led by the Defense Health Organisation and supported by the Defense Healthcare Education and Training Centre.
Recruitment Process
Recruitment is coordinated with the broader Dutch military recruiting system, ‘WerkenbijDefensie.nl’ which advertises positions and provides information to candidates.
Education and Training
Most initial medical education is obtained through civilian universities and colleges, offering foundational degrees and specialized programs, such as nursing and physician training. Once recruited, all personnel undergo additional training at the Defense Healthcare Education and Training Centre, where they complete military-specific medical training, including field medicine and emergency trauma care.
After medical education, skills and knowledge are kept current at each medical officers personal brigade and they gain experience in a hospital.
Institute for cooperation between Defence and Relational Hospitals (IDR)
A unique collaboration exists between the Dutch military and civilian hospitals, in which 14 hospitals participate. Under this arrangement, military healthcare personnel are placed in these partner hospitals as full-time medical staff but continue to be paid by the government. In exchange, medical specialists from these civilian hospitals voluntarily register as reservists, committing their expertise to support the military when needed. This system strengthens the skill sets of military healthcare providers through daily civilian practice while ensuring that the military has access to a broader range of specialized care and expertise in times of crisis or deployment.

Figure 4: The participating hospitals of IDR source: Ministry of Defence Netherlands
CIVIL-MILITARY RELATIONS
The NLD Military Health Service highly depend on support by the civilian healthcare organizations. Specialist teams are recruited and deployed by a specific military agency and specialist medical personnel support military medical education and training as reserve officers and reserve noncommissioned officers. The interaction with the civilian sector will increase even more as we strive to ensure the required medical quality. This will be achieved by embedding military medical personnel in civilian healthcare organizations for periodical training.
CBRN
The Defence CBRN Expertise Centre is the hub for all knowledge, education, training, and deployment related to chemical, biological, radiological, and nuclear materials. Approximately 110 employees (both military and civilian) work there. The centre is located in Vught and is part of the Army's Engineer Training and Education Centre and has a dedicated medical staff of 3 Subject Matter Experts.
(status: 12th September 2025)











