
Article: Kashta, Almir, Thierbach, Rene, Mueller, Sabine, Eger, Thomas
Short-time effect of systemic adjunctive Metronidazole and Azithromycin in non-surgical periodontal treatment in refractory chronic periodontitis patients
Untreated advanced periodontal disease is a main reason for the development of dental emergencies and sick call during deployments. Periodontal pathogens can not be removed through mechanical treatment only. Black Pigment Producing Rods (BPRs) have an important role in the pathogenesis of the periodontal disease. Metronidazole (MET) has been for a long time the antibiotic of choice in the treatment of BPRs-related refractory severe periodontitis. However the use of MET relates to many side effects, requires a relative long time of medication (7-10 days) and it interacts with alcohol. Azithromycin (AZM) has been suggested since 2007 in the treatment of refractory periodontitis associated with BPR infections. It can be administrated for 3 days, what possibly improves the patient’s compliance. The purpose of this study was to compare the clinical results of the periodontal therapy in combination with systemic perioperative AZM and MET. Both treatment regimes resulted in a significant reduction of probing pocket depth (PD) in nonsmokers and smokers, compliant and partly-compliant patients. Our findings propagate the adjunctive use of narrow spectrum systemic antibiotics for periodontal therapy. Based on this concept microbiological screening would be useful before using antibiotics in the therapy of periodontal disease to achieve dental fitness.
Introduction
Periodontitis is a multifactorial disease with basically entity as a bacterial infection. The imbalance between bacterial infection and host response can be affected by many environmental, life style and genetic factors. Socransky et al. 1998 classified the subgingival bacterial flora in complexes according to the time of colonization of the biofilm and their role in the pathogenetic mechanism of the periodontal disease. Black Pigment Producing Rods (BPRs) belonging to the Red Complex (Porphyromonas gingivalis, Tannerella forsythia) are of an important role in starting and developing of advanced periodontal disease.
Patients that do not respond adequately to the mechanical treatment of periodontitis are prime candidates for adjunctive antimicrobial therapy (Fig.1, 2).


Periodontal pathogens can not be removed through mechanical treatment only (Mombelli et al 2000, van Winkelhof & Winkel 2009). A combination of Metronidazole and Amoxicillin has shown to be effective to combat Aggregatibacter actinomycetemcomitans (Aa). The beneficial effect of adjunctive antibiotic therapy combined with FMDSRP is reported by several authors (van Winkelhof & Winkel 2009, Herrera et al. 2002, 2008, Haffajee et al 2003).Metronidazole has been for a long time the antibiotic of choice in the treatment of the periodontal patients who had a BPRs related periodontal disease (Mombelli & Lang 1992). However the use of Metronidazol has been related to many adverse drug reactions either neurological or concerning the gastrointestinal system (metallic taste, diarrhea and other), urine changes and other urinary tract dysfunctions. Other affected organs are skin, eyes, liver, blood and immune system. But most important in the treatment of periodontal disease is the interaction of Metronidazole with alcohol. Except of the possible limited drug effect, the interaction can provoke skin redness, nausea, vomit and headaches. The relative long medication time of 10-14 days may also lead to non-compliance of the patient (Greenberg 1984, Loesche et al. 1993) and eventually to an unsuccessful treatment of the periodontal disease.
Azithromycin has been suggested since the middle 90s in the treatment of periodontitis (Sefton et al. 1996). It can be administrated orally. The prescrition for a short time (3 days) probably improves the patient’s compliance. The side-effects of AZM can be pronounced with alcohol consume (Mombelli 2008).
Gomi et al (2007) showed that AZM was very effective in the treatment of periodontal disease and that the concentration of AZM remained high till 14 days in GCF.
Finding the right antibiotic with the less adverse drug reactions is of great clinical relevance, especially for those patients who do not respond adequately to mechanical therapy. The aim of our study was to examine and compare the clinical effect of a systemic medication with Metronidazole and Azithromycin in combination with nonsurgical periodontal therapy in full-mouth deep scaling and root planing (FMDSRP) for teeth with BPRs infections.
Material and method
Retrospectively each patient was assigned a baseline diagnosis (e.g. generalised severe chronic periodontitis) according to the actual classification of periodontal diseases (Armitage 1999) with attachment loss ≥ 3mm and/or radiographic bone loss ≥ 30% of root length at ≥ 30% of sites. Periodontal examination included messurement of probing pocket depths (PPD) and recession to the nearest 1 mm using a manual periodontal probe (PCPUNC 15; Hu Friedy, Chicago, IL, USA) at 6 sites per tooth.
The study was planned as a retrospective one in which 55 at least for 5 years full or partial compliant patients with refractory chronic periodontitis between 2005 and 2009 and an infection with BPRs were selected and divided in two groups. Exclusion criteria were aggressive periodontitis, infection with Aggregatibacter actinomycetemcomitans, taking of antibiotics or bisphosphonate in the last 6 months. Diabetes mellitus and obesive patients with a Body Mass Index>30 were also excluded.
Microbiological analysis
A microbial screening was performed to identify BPRs patients. Microbiological testing was performed with 4 paperpoints to the 4 deepest periodontal pockets of different teeth in each patient (Gomi et al. 2007) 6 weeks before nonsurgical periodontal treatment (IAI-Padotest, Zuchwil, Switzerland).
Patients with BPRs lower than 10 % of the total bacterial counts got no additional systemic antibiotics and were also excluded from analysis (Weyer et al. 2007).
Evaluation of radiographs
Prior to periodontal therapy and 1 year later complete sets of periapical radiographs (Ultraspeed; Kodac, Rochester, NY, USA) in XCP technique using film holders (XCP, Kentzler & Kaschner Dental, Ellwangen/Jagst, Germany) or panoramic radiographs were obtained of each patient. Intraoral size 0 (maxillary canines and mandibular anteriors) and 2 (all other regions) dental films or panoramic films were exposed to an x-ray source (periapical: Heliodent 70Ò, 70 kV, 7 mA, Sirona, Bensheim, Germany/panoramic: OrthophosÒplus D 3200, Siemens, Bensheim, Germany) and developed under standardized conditions (XR 24 NOVA, Dürr Dental, Bietigheim-Bissingen, Germany).
All radiographs were viewed in a darkened room using a radiograph screen (DSK, Maier, Garmisch-Patenkirchen, Germany). Relative bone loss in percent was assessed at the periodontally most affected site of each tooth using a Schei ruler (Schei et al. 1959) and teeth were assigned to one of 5 groups of periodontal bone loss (< 20%, 20/< 40%, 40/< 60%, 60/< 80%, 80%and more) (Kim et al. 2007, Pretzl et al. 2008). All radiographic assessments were performed by one examiner (AK).
Evaluation of patients’ charts
The following information was retrieved from the patients’ charts:
- The main outcome variable of this study (tooth loss after therapy) was assessed by comparison of the first and last suportive periodontal therapy (SPT) examination.
- Medical history: Patients were categorized according to self-reported hypertension, cardiovascular disease (CVD), artritis, osteoporosis and diabetes mellitus.
- Dental status
- All patients who had lost teeth were asked for the reasons (e.g. caries, endodontic, periodontal, orthodontic, prosthetic, trauma etc.)
Retrospectively each patient was assigned a baseline diagnosis (e.g. generalised severe chronic periodontitis) according to the actual classification of periodontal diseases (Armitage 1999). If the information on PAL-V was missing at baseline this parameter was replaced by interproximal bone loss.
According to self-reported smoking history patients were categorized as current or nonsmokers. Non smokers were either patients who had never smoked in their lives or former smokers who had quit smoking for at least 5 years. All other patients were classified as current smokers (Lang & Tonetti 2003).
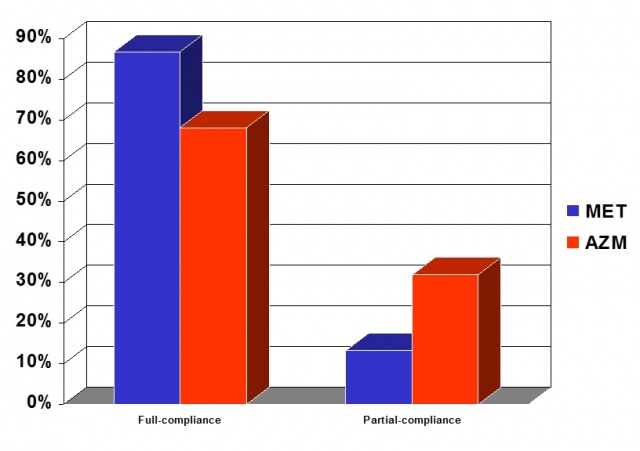
It was documented for each patient whether he or she had attended SPT at the Department VIIA (Periodontal Specialist Centre), Central Hospital of the German Armed Forces Koblenz regularly complying with the intervals that had been recommended.Compliance measures the agreement of patients’ behavior with medical recommendations (Wilson 1996). Patients attending ≥80% of all SPT visits within the recommended time ± 1 month were accounted for as full compliant (Demetriou et al. 1995). If a patient had extended the recommended SPT interval at least once over 100% he or she was accounted for as non-compliant (e.g. the recommended SPT interval was 3 months and the patient returned for SPT after 7 months) (Eickholz et al. 2008). Patients attending 50 to 80% of all SPT visits and extending the recommended intervals by ≥ 1 months but not more than 100% were accounted for as partial compliant.
Non surgical periodontal treatment and adjunctive systemic antibiotic regime
The first group (30 patients) used Metronidazole 3 x 400 mg/ day for 10 days (Mombelli & Lang 1992) starting 24 hours before FMDSRP in the years 2005-2007. The second group (25 patients) used Azithromycine 500 mg/day for 3 days perioperative (starting 2 day before SRP) in combination with FMDSRP (Gomi et al. 2007) in the years 2008-2009. Clinical parameters periodontal pocket depth (PPD), bleeding on probing (BoP), clinical attachment level (CAL) were evaluated at baseline and 6 weeks after FMDSRP. Radiologic Bone Loss (RAL) was measured at baseline and 1 year post-op. No additional surgical periodontal therapy followed during this time period. In five cases additional endodontic and seven cases necessary prosthetic treatment was performed. Compliance with individual SPT was measured one year after FMDSRP. All patients were treated from the same periodontist (TE), the clinical data were sampled from the same clinician (AK) and all statistical analysis were performed by another author (RT).
Results
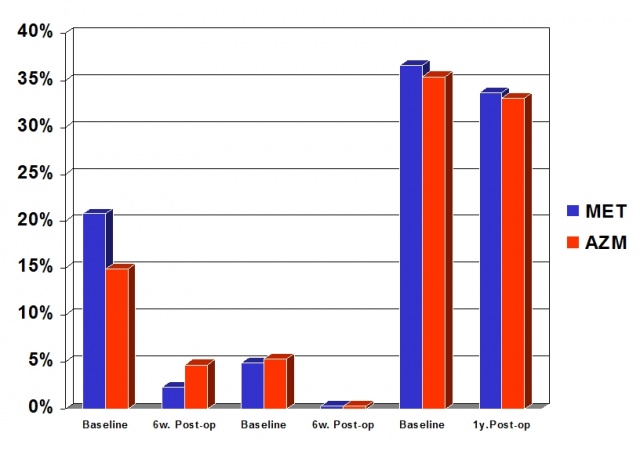
The MET group patients were on average 53.9 years old (SD 10.0 years), had 22.4 teeth (SD 4.5) and an overall average radiological bone loss (RAL) of 36.6% (SD 9.4) at baseline. Three (10 %) of them were female and 40 % smokers. The patients of the AZM group were on average 58.4 years old (SD 6.9 years), had 21.5 teeth (SD 5,0) and RAL of 35.4 % (SD 8.4). Five (25%) of the patients were female and 28% smokers. The two groups were similar and comparable with respect to the age, number of teeth RAL, smoking and other risk factors at baseline (Tab.1). Most of the patients were full compliant with the treatment and did not miss a single treatment apointment during the study period of one year (Fig.3). No patients were non-compliant during the first post-op treatment year.
Both treatment-groups resulted in a reduction of PD and RAL (Fig.4). The number of lost teeth during the first post-op year was less than 0.4 per patient in both groups. Adjunctive systemic AZM reduced 5-6 mm pockets by 9.5%, deeper pockets by 5.5%.8 teeth (out of 538 in total) were lost in 7 patients during the first post-op year. The respective reductions in the MET group were 18.5% for 5-6 mm pockets and 4.6% for deeper pockets. During the following year 11 teeth (out of 672 alltogether) were lost in 8 patients. Gain of radiological attachment in the residual dentition one year after FMDSRP was 2.3% (AZM) and 2.9% (MET) (Fig.2). Smokers in the MET-group had a non significant greater reduction of the PD in the deeper pockets compared to non-smokers. Deeper pockets (> 7 mm) were reduced to 0.1-0.4% for smokers and nonsmokers in both groups (Tab.2).
Discussion
Quirrynen et al. 1995 suggested a Full Mouth Disinfection (FMD) concept in order to avoid intra-oral transmission of the periodontal pathogens from periodontal pockets to recently instrumented sites. This concept included the disinfection of the entire oral cavity within 24 hours (Lang et al. 2008). The results in the literature are not homogenous about the real clinical effect of FMD or its modified version FM-Deep Scaling Root Planing. Lang et al. 2008 found differences in the clinical parameters between FMD or FM-DSRP and the conventional staged debridement that are hardly relevant from clinical point of view. In our clinic we have been treating patients through FMSRP because of the long distances that most of them have to travel (on average >2 hours). Our unpublished data show that patients compliance with respect to the number of visits is strongly correlated to the distance they have to travel to our clinic.
Red complex bacteria could have an important role in the refractory chronic periodontitis (Socranscy et al. 1998). In accordance with the results of other studies we showed that a recurrence or persistence of Porphyromonas gingivalis is noticed 6 months after treatment (Xajigeorgiou et al. 2006, Fleming et al. 1998). A preliminary study showed that recurrence of BPRs occurs in 30% of treated periodontal patients after the first year of periodontal maintenance and more than 70% after 5 years (Weyer J, Eger Th 2007) even after treatment with amoxycillin and metronidazole after FMDSRP.
Both of our treatment groups showed a reduction of the residual PPD, which might not be controlled in the first phase only by FMDSRP. The beneficial effect of the adjunctive antibiotic therapy combined with FMDSRP is reported by several authors. (Van Winkelhof & Winkel 2009, Herrera et al. 2002, 2008, Haffajee et al. 2003).
MET is a bactericide antibiotic, belonging to the imidazole group. It is very effective against gram negative periopathogenic bacteria (Loesche et al. 1984, 1991, Feres et al. 200). AZM is a bacteriostatic antibiotic and also effective against some Gram negative rods. Although some authors suggest that bacteriostatic drugs may not be suitable for treating biofilm infections (van Winkelhof et al. 2000 ), since the middle 90´s more studies showed positive effect for the adjunctive use of systemic AZM in periodontal non-surgical treatment (Sefton et al 1996). Administrated for only 3 days, it has been shown to have higher concentration in gingival crevicular fluid than in blood serum up to 14 days after oral administration. AZM is preferentially taken up by phagocytes and therefore its level in infected tissues is higher than in non infected sites(Gomi 2007, Pin-Chuan Lai 2011).
The role of adjunctive systemic administration of both antibiotics was compared in the treatment of gingival hyperplasia in renal transplanted patients and both antibiotics were shown to be effective in reducing the amount of gingival overgrowth. However AZM had a more consistent impact (Chand DH et al. 2004)
Haffajee et al. 2007 compared the effect of four antibiotics including MET and AZM. PPD and clinical attachment level were measured including shallow pockets. They found greater reduction of CAL for MET than for AZM. In our results we found a greater reduction of PD of 5-6 mm pockets and a gain of overall RAL for MET. AZM had a better result in the > 7 mm pockets. The role of adjunctive antibiotics becomes more important for the reduction of deeper pockets in the treatment of refractory periodontitis, while shallow pockets (< 6 mm) can be relatively good controlled by DSRP (Mongardini et al 1999). By providing an additional treatment benefit especially in deep pockets, systemic antibiotics can reduce the need for further, surgical therapy (Mombelli A. 2008).
Dastoor et al. 2007 found a significant gain of clinical attachment in smokers using AZM as adjunctive therapy to the SRP compared to the control (placebo) group - SRP only. Mascarehnas et al. 2005 found that adjunctive AZM in combination with SRP enhances the efficacy of non surgical periodontal therapy in reducing PD and improving AL in smokers. With both adjunctive systemic antibiotics in our treatment the > 7 mm pockets in smokers were impressively reduced to 0.1-0.3%.We found no significant differences in the clinical and radiological outcome for smokers, nonsmokers, partly or fully compliant patients in both antibiotic treatment groups.
Study limitations
The short time of clinical evaluation, small number of patients with full compliant refractory periodontitis (n: 43) and a missing non-antibiotic (placebo) control-group are important for the interpretation of our results. Further research on diabetic and obesive patients and aggressive periodontitis patients is necessary.
Conclusions
The use of adjunctive AZM or MET in combination with FMDSRP has almost the same clinical effect on the reduction of deep periodontal pockets in refractory, localized severe chronic periodontitis. The disadvantages of MET (neurological and gastrointestinal adverse drug reactions, long time of intake which could possibly lead to bad compliance and its interaction with alcohol) and the advantages of AZM (a better result in the reduction of deeper pockets, its short time of use, no alcohol interaction) make the combination of AZM with FMDSRP a short time, easy to administer, sure and attractive alternative to the adjunctive antibiotic treatment of refractory chronic periodontitis.
Practical implication: The presence of beneficial bacterial species may suppress the activity of pathogens especially for soldiers in combat situations. It may be advantageous to eliminate specific target bacteria only. Our findings propagate the adjunctive use of narrow spectrum systemic antibiotics for periodontal therapy (Mombelli 2008). Based on this concept microbiological screening would be useful before using antibiotics in the therapy of periodontal disease to achieve dental fitness.
Corresponding adress:
First Lieutenant (DC) Almir Kashta, MD
German Armed Forces Central Hospital,
Center for Dental Specialties
Dept. VII A - Periodontology
Ruebenacherstr. 170,
D- 56072 Koblenz
Kashta, Almir 1, 2, Thierbach, Rene. 2, Mueller, Sabine 2, Eger, Thomas2
1.Albanian Armed Forces, Medical Service
2.German Armed Forces Central Hospital, Dept. VII A Periodontology, Ruebenacherstr. 170, D- 56072 Koblenz
The authors declare that they have no conflict of interests. This study was funded by the authors and their institutions. The opinions expressed in this article are those of the authors and cannot be construed as reflecting the views of the German Armed Forces’ Medical Service, the German Armed Forces at large nor the German Ministery of Defence.
 Curriculum Vitae Lieutenant Almir Kashta. Medical Service of the Albanian Armed Forces
Curriculum Vitae Lieutenant Almir Kashta. Medical Service of the Albanian Armed Forces
1997 Medical Academy of Thessaloniki -Greece , 1998 “Aristotle” University of Thessaloniki- Medical Faculty/Dental School,2004 2ndLieutenant Albanian Armed Forces Medical Service, 2004 Training Oral Surgery 401 General Army Hospital Athens Greece, 2005 Logistic Command- Medical Branch Tirana Albania, 2006 Central Military University Hospital Tirana Albania, 2007 Promotion to 1st Lieutenant,2010 Training in Periodontology, Center for Dental Specialties, German Armed Forces Central Hospital Koblenz Germany.
Date: 12/08/2011
Source: MCIF 4/11










