

Article: T.F. MONAR, L. FAZEKAS, S. RENDEKI (HUNGARY)
Interaction between Medicin, Military and Technology
Do they need each other: Mars, Vulcanus and Aesculapius ?
The aim of the present review article is to provide a representative list of some of the main turning points where medicine, military and technology met each other. It has a non-clandestine function, that the examples presented impress political and economical decision makers.
The triad of ancient mythology characters, gods of war, technology and that of medicine respectively, they are grouped here to illustrate the potential interoperability among three different cultural phenomenons. Search for more efficient methods, techniques when military force is applied to achieve certain political goals and minimalise their mortal effects on human beings at the same time, it seems to be two antagonistically opponent goals. However, history teaches (another god comes into mind, she is Clio) that medicine in general and surgery in particular always gets an impetus when need arouses for care of wounded and sick - inevitable results of armed conflicts.1 Mars and Aesculap are equally heavily dependent on technology and it is even more true as we approach present day practice. This interdisciplinary observation is underlined by the fact, that the human factor is an extremely strong but not sole determinant of the final outcome in both terrains. The aim of the present review article is to provide a representative list of some of the main turning points where medicine, military and technology met each other. It has a non-clandestine function, that the examples presented impress political and economical decision makers.
A landslide industrialization of medicine in general and of surgery in special at the end of 19th century have mirrored and profited at the same time from the deep changes in society and other cultural spheres, like technology. Repetition and mass production became the magic words in industry. The concept of (automatic) endless repetition of certain movements/actions went hand in hand of need for permanent cycles of mass production of same quality products. The emerging market and consequently industry of healing, caring for sick and wounded: hospitals, sanatoria and rehabilitation centres („Kurorte”) demanded mass production of medicines and purpose built surgical tools. Surgery as a standardized procedure was made available by aether and chlorophorm anaesthesia in the last third of the 19th century, became safe by detergents and rubber gloves a little bit later and was born as a mass procedure due to huge demand in the First World War, a level of organized carnage never seen before.
Mechanization of modern war challenged
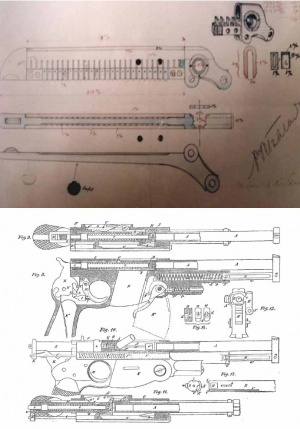 Fig. 1: Maxim gun and Singer sewing machine
Fig. 1: Maxim gun and Singer sewing machine
mechanization of surgery, as manpower limitations on one hand and quality-demand on another pressed hard for resource optimization. The core of main military inventions on the approach of the 20th century consisted of rolling, reloading mechanisms (revolvers, guns, turrets) which features were typified in their civilian counterparts in tools like sewing machine, typewriter and washing machine. The same steps and actions were repeated in the same quality resulting in a theoretically endless performance. (Fig. 1) Consistency of action, reproducibility (standardization), relative simplicity, durability and reliability were the key requirements, while relatively uncomplicated mechanisms using high quality metals were the shared features aimed at to fulfill independently for the particular purpose of the given mechanisms. On the receiving end, availability (potential for mass production) combined with easy understandability played important roles. Automatization ment a single operator or at least a minimal crew. The same concept was followed when the task was optimizing to treat, to kill or to provide proper clothing large populations.
Surgery, a „per se” craftmanship was prone to accept what technology offered while demand was high due to war related injuries. It is not surprising, that returning from the dressing stations of WW1, a young Hungarian surgeon stepped forward with the first usable surgical stapler. (Fig. 2) Standardization of surgical sutures, key element in closure of tissue and success of (bowel, stomach) anastomosis was an old dream. The first surgical suturing instrument was designed at the turn of the 19th century by Florian Hahn from Nuremberg. It was a miniature sewing machine applied to an intestinal clamp and worked on the principle of the domestic sewing machine. It applied automatically fine silk strings, the main stitching material of the day. The idea was great, the construction failed. Hümér Hültl, a Hungarian professor of surgery from Budapest replaced the running silk and catgut by fine wire hooks in his machine presented in 1905. It clipped stomach tissue in four parallel lines. Size, weight and complicated mechanism prevented its popularity, altogether 50 were produced.
 Fig. 2: Aladar von Petz (1914–1918)
Fig. 2: Aladar von Petz (1914–1918)
Aladár Petz entered the Motor Ambulance Column No 1 of the Austrian-Hungarian Army (K.u.K) as a medical officer in 1914. Returning from the Italian Front in 1918, he joined Hültl’s Clinic in Budapest and by 1920 the design of his own stapler was ready. There is no need for extra effort to imagine, that his recent mass surgical experiences in the trenches, feeling of demand combined with his affection to technology urged him to solve the problem he identified. Artistic gobeline-style stitching of the surgeon-magician had to be replaced by a more standard technique. There was a need, a concept, while the office staplers offered the solution (Fig. 3). The „gastric and intestinal suturing instrument” Petz invented applied a double- row of nickel silver inverted tip clips. instead of wires. The eccentric arms with a loading wheel at it ends made the machine lighter and easier to handle2. The Petz’s machine and its concept is the archetype of all staplers. H. Friedrich (Ulm, 1934) used replaceable staple cartridges for repeated firings while Nakayama developed his own models.
 Fig. 3: Office Stapler and cross section of loading mouth of a Maxim machine gu
Fig. 3: Office Stapler and cross section of loading mouth of a Maxim machine gu
In 1923 Petz made an agreement with Jetter Scheerer Medical Equipment Manufacturing Company in Germany, and they distributed the instrument under the trade mark „Aesculap”. The author’s name had become a verb: „durchpetzen” (to staple it throught) in the German speaking world3. The world of gastrointestinal surgery was occupied by the machine by the 1930s and 1940s4. The end of World War Two divided Europe into two halves. And Hungary had fallen into the Soviet sphere of influence. The full horizon of public life, medicine included was put under control of Soviet advisers. B. V. Petrovsky, an eminent surgeon and WW2 veteran surgeon, an exceptionally gifted and humble professor was appointed to Budapest. During his tenure in Hungary, he became acquainted with local surgical customs, of which extensive usage of the Petz stapler was an important element. Returning to the Soviet Union in 1951 Petrovsky recognized the urgent need of promoting the further development of the just recognized Petz type stapling device.5 During the Korean war, under the shadow of an imminent Third World War, scarcity of properly trained (military) surgeons available, industrialized surgical closure technique was highly demanded. B.V. Petrovsky was appointed head of Ministry of Health of the Soviet Union and he was able to realize his vision. The Kiev Scientific Institute for Surgical Devices and Instruments developed a series of mechanical staplers following Petz’s principle, but they were significantly modified and tailored to the task of the closure of both bronchi and lung parenchyma and other viscera. The American surgeon, M. M. Ravitch visited the Kiev Institute in 1958 and met N.M Amosov, his equally brilliant Russian counterpart, who presented his stapled lung cases6. G. Astafiev made also important contributions. Ravitch, (Illustration) one of the most innovative surgeons of his time also had served as a surgeon in WW2. It is said, that he operated on for 72 hours during the Battle of Bulge. No question, his own military surgical past helped him in recognizing the importance of mechanical suturing. The gun-like appearence and the triggering function of the staplers are reflecting their conceptional subliminal roots. (Illustration – a stapler and a gun) Ravitch obtained some models and shipped them to the USA. It took a decade while the concept of mechanical suturing conquered the USA.7 The entrepreneur LC Hirsch founded the United States Surgical Corporation in 1964 and further developed the „Russian staplers” as they were known by that time. The Auto Suture brand and its all metal tools became well known and only a few remembered Petz, the inventor. 1976 saw the first disposable, single-patient use mechanical staplers. In the late 1970s the first clinical trials confirmed the superiority of stapled bronchial stumps in safety. Johnson and Johnson’s Ethicon brand entered the staplers’ race in 1977. Pre-loaded magazines and extensive usage of plastics at the end of 1980s changed the world of staplers, while anastomosis machines became widely available. The 1990s brought the new concept of minimally invasive surgery which is unthinkable without automatic suturing. Technology supervened art of surgery, at least, for a while. At the same time, stapling technology opened the door for the concept of a new emergency surgical concept, introduced by military medicine demand. Forward surgical teams since the Vietnam War applied key elements of Damage Control Concept (DCC). Quick and efficient control of bleeding and infection within the thoraco-abdominal compartment, cornerstone of damage control surgery, found its tools in the quick firing, reloadable and disposable staplers8. Universality of the application was expressed in acronym: TA (thoracoabdominal).
One hundred years have passed since the birth of the conception to the daily reality of DCS supported by mechanical suturing and stapling: a result of combined efforts of surgeons in war and peace, and experts in technology.
There are at least two surgical specialties, which were born in the Great War9. Neurosurgery had two great forefathers in uniform: Cushing and Barany (Illustration: photo). Huge number of cases seen in his specialized center in France helped Cushing to lay down the foundation of brain surgery10. Barany went to serve in Przemysl (equivalent of Verdun on the Eastern Front) in the centre of the Austro-Hungarian – Russian front to practice head surgery. He won his 1916 Nobel Prize for his research on the inner-ear as a Russian POW. (Tzar Nicolaus set him free on that occasion…)
Lockwood wrote in 1940, citing Lundy, the Senior Anesthetist at the Mayo Clinic, "Out the last war came chest surgery"11. Without anesthesia it would not happen: Ivan W Magill, who is commemorated by his forceps, is not the only one to be mentioned here. Sauerbruch, father of the specialty of thoracic surgery laid down the basic principles for chest trauma as did many on the other side of the frontlines dividing the Antante and the Central Powers12. Forceps and sternum chisel carries the name of the French P Duval and the German Lebsche respectively, just two surgeons to mention.13 A rib spreader was constructed by the Argentinian Finochietto, the only thoracic surgeon to whom a tango was dedicated14 and who served in the Portuguese Military Hospital in Nelly. These eponyms are proves of what Wilkins noted: “When surgeon cuts, the past cuts with him”15. Major thoracic surgery became standard as the Great War proceeded.16 Senior surgeons in khaki such as G Gask, B Moynihan refined methods17. TP Dunhill, one of the pioneers of sternotomy referred to the wartime experience in the region of GE Gask and P Duval. The same can be said about the thoraco-abdominal (transdiaphragmatic) complex injuries18
Wound treatment was developed further 19utilizing hydrogen peroxide or sodium hypochlorite, a solution prepared by Dakin20 and popularized by Carrel. The tetanus question was raised, but only typhus and cholera vaccination reached acceptable results. The Spanish Flu (1918-9) killed as many as WW1, giving a test field how to cope with thoracic empyema. Von Bülau’s method won against the Anglo-Saxon open window policy, but the modern, evidence based21approach was laid down by US Army Empyema Commission headed by E Graham.
While there was only one X-ray in Manchuria during the Russo-Japan war (1904-5), the mobile RTG machine, not rarely on a truck, became a commonplace in both sides of the First World War. Radiographers made themselves indispensable (Foto. WW1 RTG Automobile )
The Spanish Civil War saw men of fame like Bethune22 and Trueta23, treating the wounded on the Republican side, while the brilliant Scottish Macintosh24 anesthetized the maxillofacial injured of Gen. Franco’s army. Norman Bethune, the extravagant Canadian surgeon and sociopath organized the blood banks on the Barcelona front and operated during the siege of Madrid. Large scale collection of blood, storage, distribution were the main tasks to solve he fulfilled: challenges of a military medicine environment. Similarily, Trueta, an inventive trauma surgeon made his main contribution in the concept of mass casualty evacuation/care, a Spanish experience he transplanted to London which benefited from it during the London Blitz. Fractured bones intrigued Petz also, who constructed a cast-like metal structure, called the „distractor”, as early as 1933. This unorthodox treatment of open fractures of the lower arm and leg could be considered a prototype of the „fixateur extern”: a military surgical method saw its rebirth in Iraq and Afghanistan.
The invention of Penicillin in 1928 „needed” WW2 to achieve an industrial volume production25. The sulpha-penicillin competition concluded in one of the very first drug trials, lying down the basics of medical research of our days.
Chemical warfare, poisonous gases of WW1 battlefields unintentionally led to the birth of cancer treatment. Counting on the well-known lymphocytekilling effect of the mustard nitrogen (yperite), GE Lindskog was the first to give mustin to his otherwise untreatable non-Hodgkin lymphoma patient with mediastinal mass26.
The story goes on, we could carry on with the examples, and one day we might do that. Space limitation and time at our hand prevent us from detailing further items to put on the list. Our aim was to answer the question: do we need each other? The answer is a clear cut yes.
To sum up, the above detailed turning points example the symbiotic, catalytic effect between medicine, military and technology. Looking back at the past 100 years, some of the interactions are obvious, others need further exploration, even excavative research. The aim is not better understanding alone, but direct support of decision makers of the present by exposed past experiences and even failings. Some of the concepts slept for a long time, while a need aroused – to wake up them from a sleeping beauty dream. How many other useful concepts and inventions to help save lives, or just limbs and souls (PTSD!) are still in narcolepsy? Wartime mass production and testing of existing but underused, undertested drugs like penicillin, need for machines like surgical staplers and anesthesia machines helped them to revolutionize civilian practice. Concepts of triage and damage control surgery, evacuation (scoop and run vs. stay and play), complex logistics of blood and homeostasis born in war permeated into the daily medical care in peaceful town and countryside. Obviously not all upfront technology is applicable and affordable in our routine healthcare systems. Remote controlled robotic surgery comes into mind, especially when one has social level responsibilities and faces the challenges of mass casualty care. There are many sad experiences, tested reflexes, proven decision making patterns paid dearly in the past in the „cultural memory” of the military medical mind. These are on offer for their civilian counterparts, while extremely highly specialized, evidence based, scientifically controlled knowledge can be received in return. Shortly saying, a bidirectional knowledge translation for mutual benefit is a realistic expectation from the cooperation of the military and the civilian siede. Exploring the limits and defining the futile attempts are also common responsibility and in shared interest.
Authors:
Prof Tamas F Molnar MD DSci,
First and corresponding author
9022 Győr, Batthyanyi ter 13, Hungary
e-mail: [email protected]
Co-Authors:
Col. Laszlo Fazekas MD MC(Hun),
Maj(Ret) Szilard Rendeki MD
Date: 11/12/2014
Source: MCIF 4/14











