
Article: W. H. GAN (SINGAPORE)
Dermatological Presentations in Military Conscripts
Current published studies in Military Dermatology are limited mainly to cross-sectional studies from data collated during clinical encounters in war campaigns and military training units. This retrospective cohort study presents another epidemiological perspective by examining the incidence of new onset dermatological conditions in a cohort of young, otherwise healthy military conscripts.
Introduction
Cutaneous skin disorders in military troops have long been recognised as a significant cause of morbidity that will weaken combat effectiveness, either from days lost to service or from degraded performance. Most dermatoses are not life-threatening or incapacitating, but persistent symptoms such as itch and pain may severely undermine a soldier’s combat performance. Furthermore, the propensity for mechanical skin trauma due to combat activities, combined with suboptimal field hygiene conditions, often prolong the time to full recovery from highly treatable dermatoses such as fungal skin infections. The consequent effect on troop morale may wilt fighting spirit, which can prove to be the decisive factor in the campaign outcome.
During the First World War, 126,365 U.S. Army soldiers were hospitalised for skin diseases between 1 April 1917 and 31 December 1919 [1]. Dermatoses alone accounted for over 2 million days of service lost by U.S. troops over the period of the war [2]. In terms of geographical variation in skin disease affliction among military personnel, statistics from the Second World War showed that dermatological conditions accounted for 15%-25% of outpatient consultations in temperate theatres of war, but up to 75% in the tropics [3]. This is not surprising as hot and humid environments predispose to skin disorders such as miliaria rubra and cholinergic urticaria. The tropical climate also encourages the thriving of arthropods, leading to arthropod-bite reactions, vector-borne tropical infections with dermatological manifestations, parasitic skin infections as well as various forms of tinea in soldiers. The operational impact of these seemingly innocuous cutaneous conditions should not be underestimated.
Much of what is known of military dermatology is derived from cross-sectional studies centred in war campaigns, peacekeeping operations and military training frames [3-7]. Few, if any studies, have followed up a cohort of soldiers to examine the likelihood and spectrum of new dermatological presentations while undergoing training.
This formed the basis for such a study within the context of the military population in Singapore. Singapore is a small country with a population of approximately 5.3 million people in 2012 [8]. It therefore needs to reply on conscription to build a defence force to deter external threats. One of the underpinning principles of military service in Singapore is universality, whereby all young Singaporean males who are fit to serve are conscripted. The duration of full-time military service is 2 years. Females are not conscripted for military service.
The primary objective of the study was to review the incidence and spectrum of dermatological conditions within a cohort of military conscripts. The secondary objective was to characterise a subgroup of conscripts diagnosed with contact dermatitis.
Methods
The study is a retrospective cohort study, which followed a group of conscripts enlisted for military service in the year 2007. Notwithstanding the fact that conscripts were enlisted in batches throughout the year, the study period for all were the same – starting from the day of enlistment and ending 2 years later, when the conscripts completed their full-time military service. Due to the principle of universal conscription, the cohort would be representative of male Singaporeans in the enlistment age group.
In Singapore, the military provides primary healthcare services for conscripts. Conscripts reporting sick are seen by primary care military doctors. All clinical encounters are documented in the military’s electronic medical records (EMR) system.
In this study, subjects are defined as conscripts with a first clinical encounter (classified as “Initial Consultation” under the visit category in the EMR) for a new medical complaint with the primary healthcare services. The primary diagnosis must be a dermatological condition listed in the International Classification of Diseases, Ninth Revision (ICD-9).
Subjects are identified through review of the military’s EMR system. Inclusion criteria included the military service group “Full-time National Serviceman” (i.e. military conscripts) and clinical consultations registered as “Initial Consultation”. Exclusion criteria included all other military service groups (such as regulars and reservists), follow-up medical reviews and consultations for the purpose of medical screening prior to specific military courses or activities.
Among the subjects, a subgroup of conscripts with a primary dermatological diagnosis of “Contact Dermatitis” diagnosed by primary care military doctors was identified. The EMR of all contact dermatitis cases were reviewed for body area involvement, possible occupational and/or environmental contactant and issuance of medical excuses, which served as a measure for the operational impact of disease burden.
The study was approved by the Institutional Review Board of the Singapore Armed Forces.
Results
The cohort comprised 18,749 military conscripts. Within this cohort, 5,922 (32%) subjects had one or more initial consultations resulting in a primary dermatological diagnosis. The subjects recorded 9,176 initial clinical consultations for new dermatological complaints over their 2-year period of military service. This constituted 5% of all initial consultations to the military’s primary healthcare services by the cohort for all causes. The incidence of reporting sick for new dermatological complaints was 24.5 per 100 military conscripts / year.
The mean age for the 5,922 subjects was 20.5 ± 1.4 years. The breakdown by ethnic groups was: Chinese – 4,942 (83%), Malays – 482 (8%), Indians – 313 (5%) and other ethnicities – 185 (4%).
The spectrum of dermatological presentations revealed that fungal skin infection was the commonest cause for seeking medical consultations by military conscripts, accounting for 2,526 (28%) of the 9,176 initial visits (see Figure 1). This was followed by 1,832 (20%) initial consultations for non-specific dermatitis, 657 (7%) consultations for insect bite reaction, 578 (6%) consultations for bacterial skin infection and 550 (6%) consultations for friction-related skin injury. Contact dermatitis contributed 176 (2%) initial consultations to the load of new dermatological disease presentations.
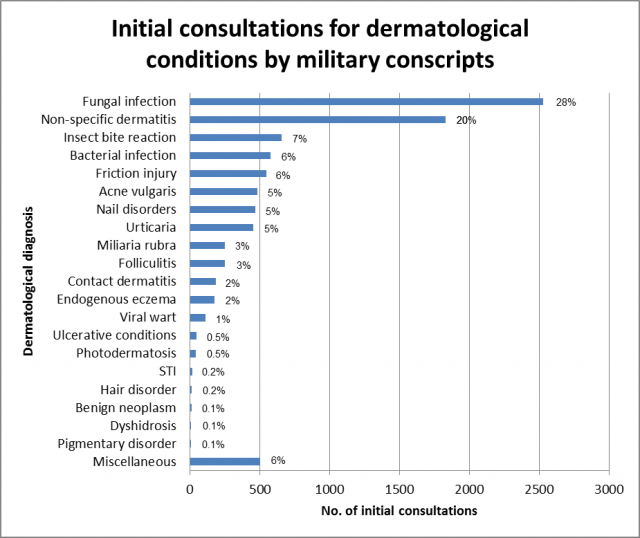 Fig. 1: The spectrum of dermatological conditions in military conscripts diagnosed by primary care military doctors (n = 9,176 initial consultations).
Fig. 1: The spectrum of dermatological conditions in military conscripts diagnosed by primary care military doctors (n = 9,176 initial consultations).
Of the top 5 causes of dermatological presentations, the incidence of conscripts reporting sick for these conditions over the 2-year period of military service ranged from 2.9 per 100 military conscripts for friction-related skin injury to 13.5 per 100 military conscripts for fungal skin infection (see Table 1).
| Diagnosis | No. of initial consultations | Incidence over 2-year military service period (per 100 military conscripts) |
| Fungal skin infection E.g. tinea pedis, tinea cruris, tinea corporis | 2,526 (28%) | 13.5 |
| Non-specific dermatitis | 1,832 (20%) | 9.8 |
| Insect bite reaction | 657 (7%) | 3.5 |
| Bacterial skin infection E.g. abscess, cellulitis, pitted keratolysis | 578 (6%) | 3.1 |
| Friction-related skin injury E.g. skin abrasions, friction bullae | 550 (6%) | 2.9 |
Table 1: Top 5 causes of dermatological presentations with the highest incidence in military conscripts
All 176 initial consultations with the diagnosis of “Contact Dermatitis” were from different subjects. Of these, 34 were excluded from the series after a comprehensive review of the medical records as these cases were deemed to be more clinically compatible with other dermatological conditions. They include miliaria rubra (22 cases), urticaria (4 cases), endogenous eczema (2 cases), tinea pedis (2 cases), insect bite reaction (2 cases), xeroderma (1 case) and keloid (1 case).
Of the series of 142 cases of contact dermatitis from the cohort included in the analysis, the breakdown by ethnic groups was: Chinese – 123 (87%), Malays – 10 (7%), Indians – 5 (3%) and other ethnicities – 4 (3%). The incidence of reporting sick for contact dermatitis was 0.8 per 100 military conscripts over the 2-year period of military service.
In contact dermatitis, the hands and feet are known to be commonly affected. Our case series showed that while there was a high proportion of cases with hands involvement (25%), the lower limbs (27%), upper limbs (21%), back (19%) and trunk (11%) were all more commonly affected than the feet (9%) in the population of military conscripts (see Figure 2).
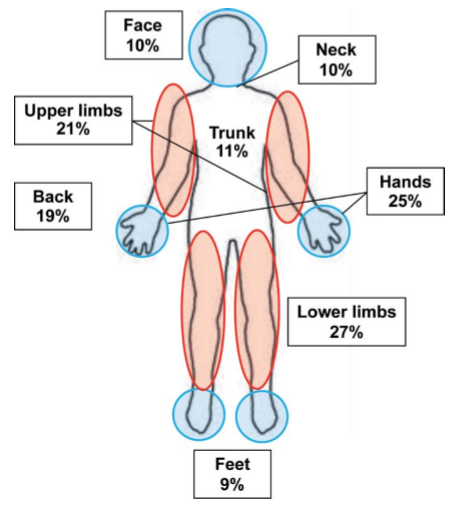 Fig. 2: Schematic diagram of the human body showing areas of involvement in military conscripts with contact dermatitis. (NB: The total body surface area involvement adds up to more than 100% as more than one area can be involved in individual cases.)
Fig. 2: Schematic diagram of the human body showing areas of involvement in military conscripts with contact dermatitis. (NB: The total body surface area involvement adds up to more than 100% as more than one area can be involved in individual cases.)
From the clinical notes, the occupational and/or environmental contactants attributed in the development of contact dermatitis included combat fatigues (8%), camouflage cream (6%), topical medicaments (6%), grass (5%) and dust (4%) (see Figure 3). Of note, no identifiable contactant was elicited in nearly half of the cases (48%).
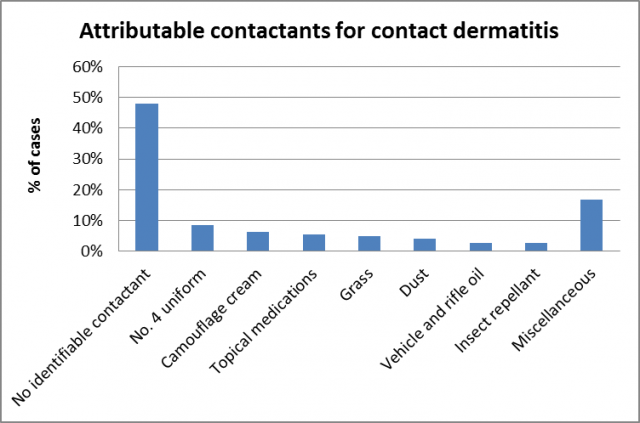 Fig. 3: Occupational and environmental contactants attributed in the development of contact dermatitis in military conscripts (n = 142 cases).
Fig. 3: Occupational and environmental contactants attributed in the development of contact dermatitis in military conscripts (n = 142 cases).
The case series of 142 cases resulted in 3 cases of permanent medical reassignment to non-combat status (2 cases of irritant contact dermatitis to grass and 1 case of irritant contact dermatitis to combat fatigues). Operational downtime in terms of temporary medical excuses included excuses from camouflage cream (104 man-days/year), combat fatigues (102 man-days/year), boots (25.5 man-days/year) and outfield training (19.5 man-days/year). In addition, the medical issuance of restriction to light duties accounted for 57.5 man-days/year. Overall, there were only 2 days of sick leave granted in the case series.
Discussion
During the period of their 2-year military service, conscripts in Singapore are provided with free primary healthcare services. As such, the vast majority will opt to seek medical consultation within the military for any ailments as this avoids out-of-pocket payment for medical services. As with the national healthcare system, access to specialist healthcare is through referral by primary care doctors. These factors gave confidence that the study would give a representative incidence and spectrum of new dermatological conditions in the military conscript population in Singapore.
Overall, new dermatological presentations constituted a fair proportion of workload for the military healthcare system. They accounted for 5% of all initial consultations by the cohort, with the incidence of reporting sick for new dermatological complaints by conscripts at 24.5% per year.
The spectrum of dermatological conditions in this study highlights 3 important points. First, fungal skin infections, insect bite reactions and friction-related skin injuries, which were among the top 5 conditions with the highest incidence in conscripts in Singapore, were also high on the list in cross-sectional studies of soldiers deployed in Timor Leste and Panama [6,7]. In contrast, prevalence surveys of dermatological cases seen in troops based out of the Middle East (Iraq and Saudi Arabia) during the Gulf War indicated a different disease pattern, with eczema and benign neoplasms dominating the burden of skin diseases [3-5]. Notwithstanding the difference in study design, it can be commented that Singapore’s conscripts have a more similar profile of common skin diseases with troops based in Timor Leste and Panama than those deployed to the Middle East. Singapore, Timor Leste and Panama have in common tropical and humid environmental conditions. The Middle East, while also hot, has an arid climate. The dissimilarity in the dermatological conditions between these regions is likely contributed by differences in climatic conditions in the areas of operation, among other factors. This knowledge serves as an important planning guidance for military medical authorities as it helps to predict the dermatological disease patterns likely to be encountered by troops deployed outside of their usual training base. This will allow appropriate medical supplies to be stockpiled and the type of diagnostic capability to be made available in field medical facilities.
Second, fungal skin infections made up the largest group of skin diseases with an incidence of 13.5% in conscripts over the 2-year military service period. Studies from other military populations lend support to the generally high prevalence of fungal skin infections, specifically tinea pedis, in this occupational group [9-12]. Length of military service [10] and the setting of military training [12] were factors which had been shown to be associated with tinea pedis in soldiers. However, one study found no association with hygiene measures [12]. Nevertheless, the high incidence of fungal skin infection in our study and its preventable nature with consistent and rigorous hygiene measures underscore the condition as one which is amenable to intervention. It will be worthwhile considering the implementation of a programme, targeted at commanders and soldiers, to raise awareness and impart the importance of creating opportunities for the regular practice of field hygiene in disease prevention.
Third, 20% of all new encounters for dermatological complaints were given a diagnosis of “non-specific dermatitis”. This reflects the level of diagnostic uncertainty faced by primary care military doctors and is a surrogate of their knowledge and practice of dermatological science. While there is no comparable study, which examines diagnostic competency of dermatological conditions in general practitioners in Singapore, Wang E et al found that only 3.6% of dermatological cases seen at one of Singapore’s largest emergency departments were referred to the dermatology clinic without a diagnosis [13]. This disparity suggests the relative difficulty in the clinical recognition of dermatological conditions by primary care military doctors. As in many other countries’ medical education systems, the coverage of dermatology for Singapore’s medical undergraduates is restricted to the introductory level. The relevant experience in recognising and managing dermatological conditions is gained from postgraduate training and clinical rotations through dermatology units. The finding in this study suggests the need to regularly update primary care military doctors in military dermatology, thereby enabling them to appreciate the onset of dermatological symptoms and signs in the occupational context of soldiers. This will enhance the diagnosis and management of dermatological conditions in our soldiers.
The incidence of contact dermatitis over the 2-year military service period was 0.8 per 100 military conscripts, indicating that the development of this condition was not common in the cohort of military conscripts. The operational impact of this disease for the military was correspondingly small, as seen from the types and period of issued medical excuses.
Causative agents in contact dermatitis can be broadly classified as occupational or environmental contactants. In many aspects, the military can be perceived as a microcosm of the wider society, and many of the industrial sectors are also found, albeit on a smaller scale, within the military. As a result, soldiers in specific vocations may be exposed to oils, fuels and solvents (vehicle and aircraft mechanics); paints (sailors involved in ship repair and painting); and detergents (military cooks). These are in addition to the potential for the development of contact dermatitis to military-specific contactants such as explosives, munitions, fuses and combat gases [14]. Plants and insects form the largest groups of environmental contactants, with the specific flora and fauna dependent on the climate and indigenous species of the geographical locations of operation.
No contactant could be identified in 48% of cases. The reasons might include the difficult in pinpointing the culpable agent among the myriad of new occupational and environmental exposures that conscripts were simultaneously exposed to during military training, or the inadequate training of primary care military doctors in performing an occupational medical surveillance.
An earlier study of occupational skin diseases in military personnel seen at Singapore’s largest dermatology unit between 1989 and 1999 found irritant contact dermatitis (ICD) to be more common than allergic contact dermatitis by a factor of 4.4 to 1 [15]. The most common irritants were oil/grease, wet work and solvents, and the most common allergens were food and chromates. Grass is a potential environmental contactant, which is very common in the tropical island-state of Singapore and soldiers will almost always be exposed to grass in military training areas around the country. Approximately 150 cases of grass intolerance are referred to the dermatology unit annually, with the majority of them being young men who are undergoing military training or about to be enlisted into military service [16]. Two studies published in the 1990s which evaluated Singaporean soldiers presenting with grass intolerance indicated that the majority were due to ICD rather than true grass allergy [16,17].
With this background in contact dermatitis in Singapore’s military population, our study suggests that there may be a shift in the type of contactants after more than a decade. Combat fatigues, camouflage cream and topical medicaments such as muscle relaxant spray appear to have replaced the “traditional” industrial-related contactants. This is also reflected in the preponderance for more diffuse body surface involvement. A plausible explanation for the shift in the type of exposures is the outsourcing of selected functions by the military within the last decade, including vehicular and aircraft maintenance, and military-wide catering services. These functions are now undertaken by commercial contractors. Another contributing factor could be the increased awareness and improvement in occupational safety and health standards and practices within the military.
Pertaining to environmental contactants, there were only 7 cases of grass intolerance reported in our series. It is possible that with an increasingly educated and informed society over time, young men (and their parents) have become more aware of medical issues that may potentially cause them problems during military service. They are therefore more ready to report them for medical evaluation before enlistment. This may occur during pre-enlistment medical screening, which takes place 6 to 9 months prior to military service enlistment and are not data included for the purpose of this study. Overall, the study results should be interpreted taking cognisance that the case series represents a primary care perspective of contact dermatitis without the benefit of specialist opinion nor clinical investigations, whereas previous studies referenced earlier analysed confirmed cases diagnosed by dermatologists.
Our study has several limitations. Firstly, using medical records as a research tool is suboptimal due to the variable quality of clinical entries by doctors. This makes data interpretation challenging and may skew results in some instances, such as the reported high proportion of contact dermatitis cases with no identifiable contactants. Clinical and occupational history might be sought but not entered. Secondly, excluding 34 (19%) out of 176 cases of contact dermatitis from analysis due to diagnostic error may call the overall validity of the other diagnoses into question. A point in mitigation is the recognition that the accurate diagnosis of contact dermatitis requires dermatological experience whereas other more common conditions in our study, such as fungal skin infections and insect bite reactions, would generally be much less diagnostically perplexing even for junior doctors. Thirdly, the analysis of contact dermatitis cases was performed without the benefit of patch tests. While positive test results are to be expected in only a minority of cases as most contact dermatitis are irritant in nature, it would nonetheless be useful in more accurately defining the types of (allergic) contactants.
In conclusion, this study has been able to present the incidence and spectrum of dermatological conditions in a cohort of military conscripts in Singapore. As far as the authors are aware, this is the first study of its kind in the region. The results of this study offer a unique opportunity to understand the development and impact of dermatological diseases in a military population training in a tropical environment. This will also set the stage for future epidemiological studies to understand the impact of the operating or training environment on a soldier’s risk of the development of skin diseases.
Key points
- Previous studies on military dermatology are cross-sectional studies, whereas this retrospective cohort study examines the incidence of dermatological conditions in a cohort of young, otherwise healthy military conscripts.
- Fungal skin infection has the highest incidence among new dermatological presentations in military conscripts, a condition amenable to primary prevention with rigorous practice of field hygiene.
- The list of contactants attributable for the onset of contact dermatitis have shifted away from “traditional” industrial-related agents like grease, solvents and chromates, reflecting the occupational evolution in the type of military duties undertaken by military personnel over the years.
Author:
GAN Wee Hoe
MBBS(S’pore), MPH, DAvMed(UK), MRCP(UK), FRCP(Edin), FAMS
Chief Air Force Medical Officer, Republic of Singapore Air Force
Concurrently Assistant Chief of Medical Corps, Singapore Armed Forces
RSAF Aeromedical Centre, 492 Airport Road, Singapore 539945
Email address:[email protected]
Tel (Office): (65) 6210 0501
Tel (Mobile):(65) 9698 0702
Fax:(65) 6285 3032
Acknowledgements
The author would like to acknowledge the Singapore Armed Forces Medical Corps for granting permission to access the data for this study. I also want to thank Ms Janet Lim from HQ Medical Corps for her assistance in data-mining. The opinions and recommendations expressed in this paper are those of the author and do not represent official policy of the Ministry of Defence, Singapore or the Singapore Armed Forces.
References: [email protected]
Date: 10/15/2015
Source: MCIF 4/15











