
Article
Prospects of Molecular Diagnostics in Personalised Medicine
In general, precision medicine is a paradigm based on the perception, that future medical treatment should be tailored to the specific diseases of patients.
Under the keyword “Evidence Based Medicine” (EBM) we are going to have currently a better treatment for cancer, if one takes into account the genomic signature of diseases. That means the decisions about treatment should be based on a combination of well designed and preferably replicated research as well the clinical skills of health care professionals.
In the next time we’ll have globally to answer the question, where the way is going on!
This editorial is based on the state of knowledge of precision medicine as a feasable approach for Military Medicine too.
It is every doctor’s duty to cure, alleviate or prevent disease.
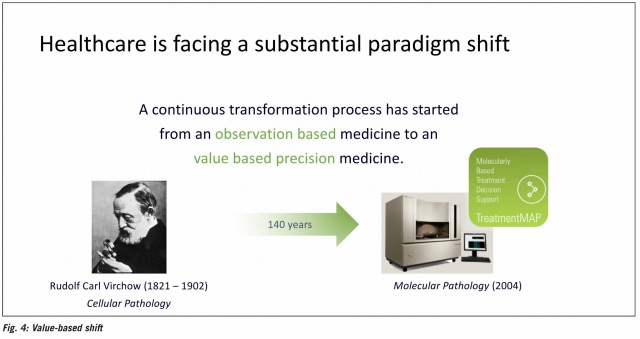
At the start of the 21st century, biomedical research and clinical medicine are in a state of flux that many are even calling a paradigm shift.
New approaches based on genome analyses and biomedical technologies make it possible to analyse vital processes more accurately and comprehensively than ever before. The hope associated with this is that causes of disease will be better understood, exact diagnoses will be made and not least highly effective, targeted and low-side-effect treatments will be developed.
The term “precision medicine” is being used commonly in international medical literature. The number of publications on this subject is growing exponentially, and Internet searches are increasing too.
On this background, it is certainly opportune to also take up this subject in international military medicine.
Personalised Treatment
Faster computers and more intelligent data links are facilitating a completely new approach in medicine. Precision medicine, the long-held dream of personalised therapy, could actually become reality as a result and therefore fundamentally change our understanding of disease.
Since Hippocrates, empirical observations, recordings of findings and contemporary procedures have shaped the medical treatment of the sick. Ground-breaking advances have occurred with the development of natural sciences. The principle of cause and effect has determined the pathway of modern diagnostics and treatment.
The decoding of the human genome now represents a milestone on the latest path towards the diagnosis and treatment of disease based on the comprehensive, personalised characteristics of patients.
The aim of precision medicine is to use targeted prevention, systematic diagnostic tools and tailored treatment methods geared towards the needs of individual patients or patient groups in order to improve the effectiveness and quality of treatment. Unwanted side effects will be reduced and the “non-responder rate” will be diminished over the long term.
It is primarily molecular technologies for the targeted determination of biological variables, known as bio-markers, that are included in the assessment of the treatment process.
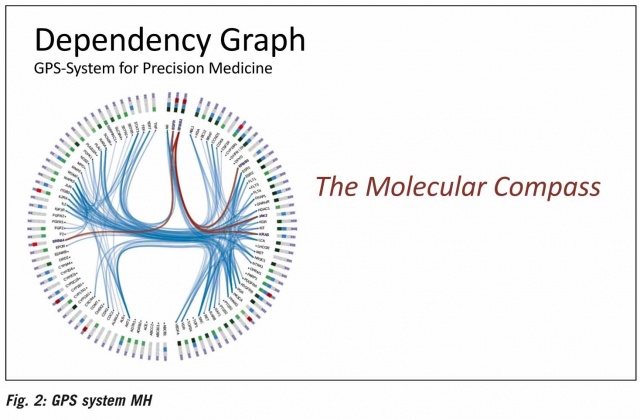
Analysing the vast array of data gathered and correlating this data with certain disease patterns or the levels of effectiveness of medical treatment represents an enormous interdisciplinary challenge.
Treatment Methods on Trial
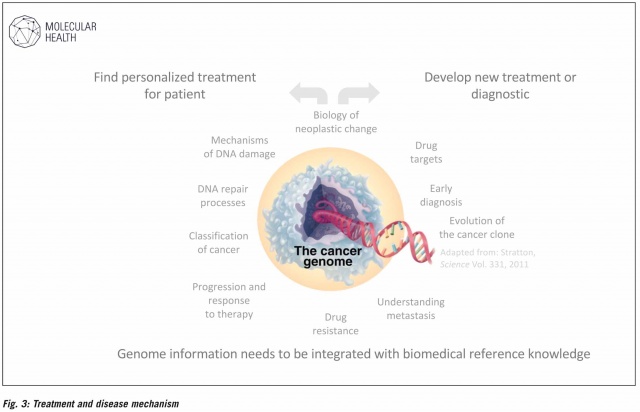
Tumour therapy is currently undergoing fundamental change. Tumours are primarily the consequence of genetic changes in body cells. Most tumour cells contain numerous (50 – 30,000) mutations that cause complex changes. The deeper understanding of the molecular mechanisms involved with the development of various types of tumour is leading to a reclassification of tumour-based disease and enabling the development of molecular tumour diagnostics and targeted therapeutic agents derived from these. It appears that the use of these treatments is associated with fewer side-effects than conventional treatment methods. As a result, traditional forms of treatment are being put on trial.
Every year, worldwide, many millions of patients with cancer are treated with chemotherapy. Conventional chemo-therapy agents generally also work on metaplastic tissue with rapidly-dividing cells (bone marrow, epithelium in the gastro-intestinal tract).
Cancer cells divide relatively frequently, which causes the tumour to grow quickly, displacing and destroying neighbouring tissue. So chemotherapy is used to attack all cells that divide quickly. However, as well as cancer cells, other cells in the hair roots, in the digestive tract and in the immune system do the same. Chemotherapy kills great swathes of tumour cells, but also even more of the body’s other cells. This leads to the patient feeling unwell, losing hair, suffering nausea and vomiting and being extremely susceptible to infections. Effectively, we are attacking everything in the body that multiplies quickly just to destroy a certain group of cells that usually only measures a few millimetres in size.
The vast majority of tumours are caused by genetic changes in body cells. The availability of tissue biopsies that are taken for diagnostic purposes makes molecular analysis possible. The resulting genetic profile provides an in-depth understanding of what is happening inside the tumour. It also provides a precise means of allocating tumours to molecular sub-groups. With many malignant tumours, treatment decisions are already being made dependent not just on the morphological findings, but also on the molecular biology findings that have also been obtained. Similar procedures are also being used in the diagnosis and treatment of infectious diseases. In neurology, molecular biology analyses are promising to open up pathways towards the early diagnosis and differentiation of various forms of dementia. Early and precise diagnosis of the molecular causes of a disease that progresses slowly, such as Parkinson’s or Alzheimer's disease, is the first vital step in the development of treatment or a preventative measure.
A large proportion of the most common chronic illnesses that occur especially in later life are multi-factorial in origin. Alongside genetic diseases, these factors include environmental influences and unhealthy lifestyles. The conditions caused include cardiovascular diseases and diabetes mellitus, as well as neuro-degenerative conditions. Treatment of the causes of chronic diseases has so far been only limited.
Molecular Diagnostics with IT
Doctors have always taken a history from the patient based on patient data, carried out a physical examination and combined the symptoms with their clinical knowledge and skill - with and without adjuvant diagnostic tools - and physiological data and laboratory parameters to obtain findings. These findings are then used to establish a diagnosis and carry out treatment, whatever it may be.
This well-used toolkit of medicine is now being extended with the targeted, methodical use of primarily molecular technologies. Biological variables, especially molecular bio-markers, are to be included in the treatment process too. The use of these bio-markers is expected to allow the increasingly accurate determination of individual biological characteristics, which will serve as the basis for suitable diagnosis and treatment. Looking long-term, it will be possible to objectivise medicine by precisely measuring and curing relevant changes in patients. Also, over the long term, an informative, more detailed classification of diseases into taxonomic groups is hoped for that will form the starting point for the development of coordinated diagnostic tools and treatments. It can be assumed that the volume of disease-related patient data available will increase. The challenge for personalised medicine lies also in storing this complex personal data in a standardised manner and deriving outcomes and treatment options from it. These must be transparent for the doctors treating the patients, the scientists involved with medical research and for the patients themselves. The management of new challenges in personalised medicine can only take place as part of a multi-disciplinary team.
The consequences of personalised
medicine are hard to predict. It requires the integration of new organisational processes into existing healthcare structures. This will also affect the military medical corps if itcontinues to follow the maxim of ultimately providing soldiers with the same medical care that can be expected from the civilian sector.
Although the general impacts on patient care associated with “personalised medicine” have not yet fully made their presence felt, it can be assumed that, despite the difficulties with acceptance that were expected initially, there will be greater transparency of treatment through evidence-based medicine in the future. Bio-informatics data processing will achieve greater prominence.
Bio-informatics forms the methodical basis of the combination and filtering, correlation and evaluation of patient data. This data, of wildly varying quality, must be medically redundant and reliable
Next-generation DNA sequencing especially is of considerable significance for the development of genomic bio-markers. Per machine and per investigative process, it allows hundreds of millions of DNA fragments to be sequenced in parallel, which means that this high-performance method now allows the genome of individual people to be fully decoded in just a few days for prices that will soon be less than 400 dollars. NGS (Next-Generation Sequencing) is already state of the art today and is being used as standard in oncology (for the sequencing of tumour tissue).
The complete or partial as a panel (20–50 genes) documentation of DNA is an important keystone of precision medicine. In future, bio-markers may also be able to make an key contribution towards the planning and delivery of clinical studies for trialling new drug treatments. Bio-markers can also contribute to drug safety by revealing pharmacological pathways. Since the occurrence and nature of bio-markers precedes a patient’s clinical response to treatment in terms of time, they may also serve as alternative end points in clinical studies and significantly accelerate and simplify them.
Summary and Outlook
While at the start of the 20th century, doctors had to rely on their five senses, experience and intuition to establish a diagnosis, they can now turn to an array of diagnostic tools. From computer-assisted history charts and imaging technology visualisation methods such as ultrasound and MRI scanning to 3D surgical procedures, new high-tech methods are constantly being added. The aims are the best possible treatment success, time savings and cost savings.
Differentiation instead of standardisation are the key words of precision medicine worldwide.
The foundations of the great advantages and benefits in drug treatment will in future be those drugs whose effectiveness has already been confirmed using reliable bio-marker tests.
Advancing molecular differentiation, especially in oncology, neurology and immunology diseases, is the trailblazer for these trends.
When US President Richard Nixon declared “war on cancer” in 1971, the aim of beating the disease within 25 years as part of a national show of strength seemed no more utopian than John F. Kennedy’s pledge in 1961 of putting a man on the moon before the end of the decade. However cancer has proved to be a tougher opponent.
In January 2015, US President Obama put 215 million dollars for research into precision medicine onto the national agenda. His initiative has helped to establish the fight against cancer based on molecular medicine. Studies are initially being funded to evaluate genome data. Precision medicine is also hoped to custom-adapt genetic profiles to modern drug therapies.
The global departure towards a new age of medicine has begun. All over the world, we are in the midst of a transformation that offers great hope!
References: [email protected]
Date: 07/21/2016
Source: MCIF 3/16










