
Article: P.Bärtsch
Who gets mountain sickness?
Altitude, ascent rate and individual susceptibility are the most significant determinants for High Altitude Cerebral Edema (HACE) and High Altitude Pulmonary Edema (HAPE) . In general, susceptible individuals can avoid an HAPE at altitudes of up to 7000 m without medication if they ascend slowly.
1. Acute Mountain Sickness
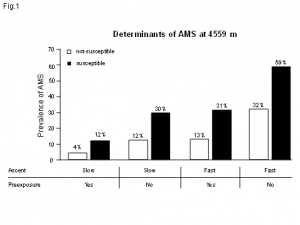 Prevalence of AMS at 4559 m in altitude, dependent on the ascent rate, preexposure
and the susceptibility to AMS for 827 climbers. A slow ascent was defined as > 3 days
as of a height of 2000 m and preexposure as > 4 days above 3000 m in the previous
2 months. Climbers who rarely or never experienced headaches during climbs over
3000 m who had a case-history score of < 4 were classified as not susceptible to AMS.
(As per reference (1)).
Prevalence of AMS at 4559 m in altitude, dependent on the ascent rate, preexposure
and the susceptibility to AMS for 827 climbers. A slow ascent was defined as > 3 days
as of a height of 2000 m and preexposure as > 4 days above 3000 m in the previous
2 months. Climbers who rarely or never experienced headaches during climbs over
3000 m who had a case-history score of < 4 were classified as not susceptible to AMS.
(As per reference (1)).
A large epidemiological study of 827 mountain climbers at the Capanna Margherita (4559 m) (1) established three independent determinants for acute mountain sickness (AMS). All three had comparable significance: preexposure, ascent rate and individual susceptibility (Figure 1).
Prevalence of AMS at 4559 m in altitude, dependent on the ascent rate, preexposure and the susceptibility to AMS for 827 climbers. A slow ascent was defined as > 3 days as of a height of 2000 m and preexposure as > 4 days above 3000 m in the previous 2 months. Climbers who rarely or never experienced headaches during climbs over 3000 m who had a case-history score of < 4 were classified as not susceptible to AMS. (As per reference (1)).
Other factors, including age, gender, level of training (self-estimated), alcohol and nicotine consumption and body weight, had no significant association with the prevalence of AMS at 4559 m in altitude. The results correspond to data collected from 3158 tourists in various health resorts in the Rocky Mountains (altitudes between 1920 and 2956 m) (2), if one disregards the significant influence of body weight on AMS among the tourists. This discrepancy can be explained by the fact that a study on mountain climbers at 4559 m is inevitably a selection of the study population vis-à-vis physical fitness and thus body weight as well.
Since preexposure and ascent rate are generally covered in consultations related to a high-altitude expedition, the evaluation of altitude tolerance depends on the degree of individual susceptibility. Information on the state of health during earlier expeditions at comparable altitudes, periods of preexposure and ascent rate enable one to assess the risk. Since such information is not always available, several experts recommend tests for assessing altitude tolerance. The most significant methods for the characterization of altitude tolerance are based on the following findings:
- Individuals with altitude sickness have lower arterial oxygen saturation (SaO2) than control subjects without illness. There is considerable overlap among the individual values, however. (3)
- A low hypoxic respiratory drive is considered as a cause for the high level of hypoxemia associated with AMS. However, studies on this have produced contradictory results.(4)
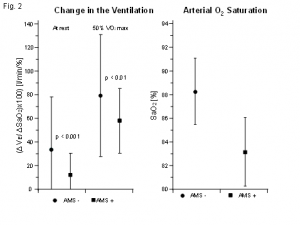 The left half shows the ventilation (mean value ± standard deviation) in normobaric
hypoxia (FIO2 0.115), presented as the increase in the ventilation in L/min per decrease
of one percent saturation, at rest and under exertion with 50 %VO2max, n = 128. (As
per reference (5)). The right half shows the oxygen saturation (mean value ± standard
deviation) measured with pulse oximetry 20-30 min after exposure to normobaric
hypoxia (FIO2 0.10 – 0.15) or 20-30 min after arriving at 2000 - 4500 m in altitude
after passive, rapid transport. 63 individuals with poor and 83 individuals with good
altitude tolerance. (As per reference (6)).
The left half shows the ventilation (mean value ± standard deviation) in normobaric
hypoxia (FIO2 0.115), presented as the increase in the ventilation in L/min per decrease
of one percent saturation, at rest and under exertion with 50 %VO2max, n = 128. (As
per reference (5)). The right half shows the oxygen saturation (mean value ± standard
deviation) measured with pulse oximetry 20-30 min after exposure to normobaric
hypoxia (FIO2 0.10 – 0.15) or 20-30 min after arriving at 2000 - 4500 m in altitude
after passive, rapid transport. 63 individuals with poor and 83 individuals with good
altitude tolerance. (As per reference (6)).
Many groups have studied the connection between hypoxic ventilatory response (HVR) and AMS. While studies with up to 30 subjects did not establish a significant association for the two parameters (4), a prospective study of 128 mountain climbers by Richalet et al. (5) demonstrated that AMS is associated with a significantly lower ventilatory response to normobaric hypoxia (FIO2 = 0.115) in the lab (at rest and under exertion). The results of this study are presented in Figure 2 (left half); there is such a high degree of overlap in the individual values that the test is not suited to providing a reliable prognosis in individual cases. While there is a statistical significance, these differences in the HVR have no clinical relevance vis-à-vis consultation.
Unfortunately, the same applies to measuring arterial oxygen saturation with a pulse oximeter during hypoxic exposure in the lab or in field studies. Burtscher et al. (6) carried out such measurements on 150 subjects with known altitude tolerance and found significantly lower values in individuals with poor altitude tolerance compared to those with good altitude tolerance. The large overlap in the individual vales originates from the results presented in Table 2 (right half). Consequently, one must distinguish between statistical significance and clinical relevance for this study, as well.
The left half shows the ventilation (mean value ± standard deviation) in normobaric hypoxia (FIO2 0.115), presented as the increase in the ventilation in L/min per decrease of one percent saturation, at rest and under exertion with 50%VO2max, n = 128. (As per reference (5)). The right half shows the oxygen saturation (mean value ± standard deviation) measured with pulse oximetry 20-30 min after exposure to normobaric hypoxia (FIO2 0.10 – 0.15) or 20-30 min after arriving at 2000 - 4500 m in altitude after passive, rapid transport. 63 individuals with poor and 83 individuals with good altitude tolerance. (As per reference (6)).
In summary, one can state that preexposure, ascent rate and individual susceptibility are the most important predictors of AMS. Susceptibility is best assessed from anamnestic specifications. Tests for determining susceptibility to AMS do not make much sense due to insufficient selectivity. Since high altitude cerebral edema (HACE) generally results from progressive AMS, the same applies to HACE, as well. If there is a suspicion of HACE from the medical history, this suspicion can be confirmed with MRT evidence of haematosis in the brain, in particular in the corpus callosum. (7)
2. High Altitude Pulmonary Edema
The numbers in Table 1 on the prevalence of high altitude pulmonary edema (HAPE) make clear that HAPE is dependant on altitude, the ascent rate and individual susceptibility.
Table 1
Prevalence of High Altitude Pulmonary Edema (HAPE)
Altitude Ascent Prevalence
Alps 4559 m 2-4 days 0.2 %
Himalaya Trekking 5450 m 6 days 2 %
Alps (without history of HAPE) 4559 m 22 hrs. 6 %
Himalayas (soldiers) 5500 m Flight/auto. 16 %
Alps (with history of HAPE) 4559 m 22 hrs. 62 %
Influence of the ascent rate, altitude and susceptibility on the prevalence of HAPE. (Data from references (14;15;16)).
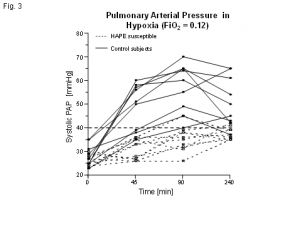 Systolic pulmonary arterial pressure for
10 HAPE-susceptible (solid line) and 10
non-HAPE-susceptible (broken line)
persons during a four-hour exposure to
normobaric hypoxia (FIO2 = 0.12, PO2
corresponds to an altitude of 4500 m).
(As per reference (12)).
Systolic pulmonary arterial pressure for
10 HAPE-susceptible (solid line) and 10
non-HAPE-susceptible (broken line)
persons during a four-hour exposure to
normobaric hypoxia (FIO2 = 0.12, PO2
corresponds to an altitude of 4500 m).
(As per reference (12)).
The HAPE increases the faster and higher the ascent. As of yet, the influence of preexposure has not been studied systematically. Anecdotal reports from Mt. McKinley on climbers who descended to base camp after a HAPE at 4400 m and later climbed to the top (6195 m) successfully suggest the importance of preexposure. A number of observations demonstrate that (8) climbers who suffered a HAPE multiple times during a fast ascent in the Alps were able to reach altitudes of up to 7000 m without medical problems when they climbed an average of only 300 – 350 m/ day after the 2000 m mark or when they were pre-exposed in advance at altitudes between 3000 and 5000 m. These observations suggest that ascent rate and preexposure are significant determinants for HAPE as well as AMS.
Studies on the treatment of HAPE with medications that reduce pulmonary arterial pressure (9;10) demonstrate that the excessive pressure increase in the pulmonary arteries is a decisive pathopysiological factor in HAPE. Many studies have shown that climbers with a history of HAPE in the event of short-term hypoxic exposure experience an excessive pulmonary arterial pressure increase (11). This can be proven non-invasively for normobaric hypoxia via Doppler echocardiography (Figure 3) (12) and can thus be used for the identification of individuals susceptible to HAPE.
Systolic pulmonary arterial pressure for 10 HAPE-susceptible (solid line) and 10 non-HAPE-susceptible (broken line) persons during a four-hour exposure to normobaric hypoxia (FIO2 = 0.12, PO2 corresponds to an altitude of 4500 m). (As per reference (12)).
One retrospective study showed that the systolic pulmonary arterial pressure in 32 of 37 subjects (86 %) can be measured with Doppler echocardiography and that a cut-off value of 41mmHg exhibits a sensitivity of 77 % and a specificity of 93 % (13). General screening is not recommendable, however, due to the low prevalence of HAPE susceptibility (0.2 to 2 %) for conventional climbing or trekking (Table 1). With a prevalence of 0.2% (which can be assumed for climbing to the 4000 m mark in the Alps), it would take 500 studies to identify one person susceptible to HAPE. In the process, however, 36 other people would be incorrectly assessed as positive. With a prevalence of 1.5 - 2 %, which has been described for the trek to the Mount Everest base camp (14), 50 studies would result in one correct positive and 4 incorrect positive identifications. Furthermore, it must be noted that these calculations are based on the results of retrospective studies. It is to be expected that a prospective study - like the one ongoing in our department - will produce even less favourable numbers, so that a general screening for HAPE susceptibility using pulmonary arterial pressure measurement in hypoxia cannot be recommended. In view of a negative predictive value of 97 % (13), the measurement of the pulmonary arterial pressure in hypoxia for climbers with a history of doubtful HAPE makes sense, since a normal pressure increase in hypoxia largely precludes HAPE susceptibility.
In summary, it can be stated that altitude, ascent rate and individual susceptibility are the most significant determinants for an HAPE. In general, susceptible individuals can avoid an HAPE at altitudes of up to 7000 m without medication if they ascend slowly (300 - 250 m/day as of 2000 m). Although the excessive pulmonary arterial pressure increase in hypoxia is the decisive pathopysiological factor for HAPE and can also be used as a marker for susceptibility in the lowlands, general screening (despite a high degree of sensitivity and specificity) is not recommendable due to the low prevalence of HAPE among Alpine climbing and trekking.
Date: 04/18/2018
Source: MCIF 2/2011











