
Article: M. LÜPKE (GERMANY)
Periodontal emergency treatment in the field
In 2012, 18.63 % of all dental procedures performed during tours of duty of the German Armed Foces (Bundeswehr) were caused by periodontal problems. These 819 treatment sessions represent a not unimportant factor that requires more detailed analysis. The inflammatory periodontal disorders in question were gingivitis and periodontitis. These usually chronic periodontal diseases are common and are thus also frequently encountered in the personnel of the Bundeswehr. As these are primarily chronic disorders, patients are often unaware of their development. However, acute exacerbation may occur in the event of an impaired immune system. The complications that can result, such as periodontal abscesses and necrotising ulcerative gingivitis, may lead to significant deterioration of general well-being, considerably reducing the operational capacity of the personnel affected. It is a generally held view in medicine that the biofilm formed by bacterial plaque is the main aetiological factor in the development of inflammatory periodontal disorders. Bacterial plaque contains a wide variety of microorganisms that are also present as opportunistic microbes in the oral cavity of individuals with a healthy periodontium. Under physiological conditions, the bacterial levels in the gingival sulcus are held in check by the individual immune response of the host but when the immune response is debilitated, this counterbalancing effect is removed. When on duty in the field, personnel of the Bundeswehr can be subjected to high psychological and physical stress, the level of which is determined by the theatre of operations and the nature of the mission; long term exposure to such stress can have serious consequences for the functioning of the immune system. The following article will discuss the acute inflammatory periodontopathies that can impair the operational capacity of personnel and the aetiological factors that are associated with these disorders.
Introduction
 Necrotising ulcerative periodontitis
with a close-up of the necrotic papillae
Necrotising ulcerative periodontitis
with a close-up of the necrotic papillae
Gingivitis and periodontitis are very prevalent disorders. This was again confirmed in the Fourth German Oral Health Study undertaken in 2006. For example, it was found in subjects aged 35 - 44 years that 52.7 % had gingival pockets of a depth of 4 - 5 mm while another 20.5 % had pockets of a depth of 6 mm or greater. It is thus not surprising that periodontal disease is also widespread among Bundeswehr personnel. This is demonstrated by the results of a study undertaken by Henne et al. in which 2023 military personnel were examined in the for the military particularly relevant age range of 18 - 30 years. Of these subjects, 66.4 % had gingivitis or mild to moderate periodontitis while 12 % had serious periodontal disease. These disorders are usually chronic; in other words, they develop over a longer period and the patient remains unaware of their presence because they experience no major symptoms. It should be kept in mind, however, that if periodontitis is allowed to develop unhindered, the patient will not only suffer loss of teeth but may also experience systemic effects. But not all forms of these disorders have a direct effect on operational capacity, and so this article concentrates on the periodontal diseases that are relevant to this specific aspect.
According to current medical theory, intraoral bacteria present in the supra- and subgingival plaque play a significant role in the development of gingivitis and periodontitis. These form complex biofilms on the surface of the teeth. Bacterial plaque triggers immunological and inflammatory processes that can result in the development of clinically manifest gingivitis if the periodontium is exposed to these for longer periods. The consequence can be periodontitis involving extensive destruction of the periodontium. It is now generally accepted that microbial plaque is one of the main causes of inflammatory periodontal diseases, however, increasingly focus is being placed on the immune response of the host. If the equilibrium between microorganisms and host response is
 Frontal view of necrotising ulcerative
periodontitis
Frontal view of necrotising ulcerative
periodontitis
impaired by immune system dysfunction, inflammatory periodontal diseases can develop, progress or become acutely exacerbated. There are other co-factors of relevance. These include smoking, systemic disorders and psychosocial stress. Personnel on mission regularly are exposed to increased physical and psychological stress that can have a serious impact on their immune status. Bundeswehr personnel are currently on duty around the world. This means that they need a good dental health status and thus it is the primary task of the dental services in the homeland to ensure that their dental fitness is maintained at an appropriate level. All personnel are given an annual dental check-up during which they are examined for signs of periodontal disease with the help of the periodontal screening index (PSI). It is assumed as a basic guideline that only personnel with a good oral status can be considered to have a full operational capacity. But even with this principle in place, it is still impossible to avoid cases that require emergency dental treatment. In 2012, 4392 cases required emergency dental treatment during tours of duty of the Bundeswehr. 819 of these cases (equivalent to 18.65 % of treatment sessions) were caused by periodontal disorders.
This is a not insignificant percentage in view of the fact that acute inflammatory periodontal disorders can considerably reduce the operational capacity of the affected individuals. This is particularly the case in individuals with periodontal abscesses and necrotising ulcerative gingivitis, disorders that are considered in more detail below.
Acute inflammatory periodontal diseases
In the following, I will discuss the acute periodontal diseases that are accompanied by serious symptoms and can thus have a direct influence on the operational capacity of personnel.
Periodontal abscesses
Depending on site, abscesses can take the form of gingival abscesses, periodontal abscesses and pericoronal abscesses.
 Microbial plaque shown after staining
Microbial plaque shown after staining
Periodontal abscesses are of particular periodontological relevance; here a localised infection of the gingival tissue can result in destruction of ligaments and bone. Most abscesses develop in existing periodontal pockets. As a rule of thumb, the deeper the pocket, the greater the risk of the development of a periodontal abscess. There are various possible causes of periodontal abscesses. An important aetiological factor is the prevention of clearance from the periodontal pocket (e.g. due to impaction of a foreign body). Impaired clearance results in an accumulation of host cells, sulcus fluid, inflammatory exudate and bacteria in the pocket. Smith & Davies (1986) were able to demonstrate that 55 % of periodontal abscesses are associated with a pocket depth of at least 7 mm. Other possible aetiological factors are use of systemic antibiotics, systemic disorders such as diabetes mellitus and furcation involvement. Most periodontal abscesses tend to be located near the molars. Impaired immune status can also represent an aetiological factor that can be relevant to personnel on active duty. The situations to which personnel are exposed in the field mean that they experience considerable psychological and physical stress and this, over the long term, coupled with the effects of extreme environmental conditions, can lead to weakening of the immune system. The pre-existing balance between chronic periodontal inflammation and host response is impaired, leading to acute exacerbation of the chronic inflammation. The microbial flora in a periodontal abscess is a mixture of various microorganisms, although Gram-negative anaerobic bacteria predominate. The composition of abscess flora corresponds largely to that of the microbiological flora of deep periodontal pockets. It has been shown that there is a close correlation between the presence of Porphyromonas gingivalis and abscess processes. The acute inflammation is associated with symptoms such as inflammation, pain, swelling and the loosening or extrusion of teeth. This can also be accompanied by local lymphadenitis
 Severe periodontal dental defect of
distal tooth 14
Severe periodontal dental defect of
distal tooth 14
and fever. These symptoms can seriously impact on the general status and thus the operational capacity of affected personnel who then require emergency dental treatment. In their study, McLeod et al. (1977) demonstrated that periodontal abscesses frequently lead to loss of teeth: their figures show that 45 % of teeth were lost as a consequence of a periodontal abscess. The diagnosis of a periodontal abscess mainly involves a consideration of the patient's history, a clinical examination, sensitivity testing and radiological imaging. Particularly the presence of deep periodontal pockets can be a sign that the patient may have an abscess. It is best to proceed on the basis of the aphorism "Ubi pus, ibi evacua", i.e. where there is pus, create an opening for it to drain. This is often possible by means of forced probing of the periodontal pocket although an incision may also be necessary. It is possible to use a surgical drain to remove the exudate but this is not necessary in most cases. Also required for treatment is lavage of the lesion using chlorhexidine digluconate and the prescription of an analgesic. It is advisable to avoid root surface debridement during the acute phase of a periodontal abscess. This is not only unnecessary but can also result in damage to viable sections of the periodontium. Immediate extraction is also an option for teeth that cannot be saved. As a rule, local therapy will prove to be sufficient and it will not be necessary to prescribe antibiotics. Their use should be restricted to cases in which the abscess processes exhibit a marked tendency to dissemination. In differential diagnosis in such cases, the presence of periapical processes, endo-perio lesions and abscesses in the region of root fractures need to be excluded.
Necrotising ulcerative periodontal disorders
Necrotising ulcerative periodontal disorders take the form of necrotising ulcerative gingivitis (NUG) and necrotising ulcerative periodontitis (NUP). NUG is an infection restricted to the gingiva that is characterised by gingival necrosis, gingival bleeding and pain. Untreated, NUG can result in clinical loss of attachment, bone exposure and subsequently in bone sequestration. In literature, the cited prevalence is in the region of 0.2 - 1.4 %. Various factors are involved in its aetiology, some of which are closely associated with exposure of the individual to high levels of stress.
It is not entirely coincidental that we find the first descriptions of such periodontal disorders in reports of military operations dating to 400 BC. Certain aetiological factors are particularly relevant to military personnel on active duty. Predominant among these is psychosocial stress, which is generally seen as one of the main causative factors in necrotising periodontal disease. The level of stress (such as the threat to life and limb) to which personnel are exposed is determined by theatre of operations and mission. In addition to the effects of stress on the immune system (to which I will return later), stress can also cause changes in behaviour, such as increased consumption of cigarettes and neglect of maintenance of personal oral hygiene. It is also of relevance that necrotising periodontal disorders most commonly occur in younger age groups, such as those of military personnel in the field. The predisposing factors are shown in Table 2. In microbiological terms, these disorders are associated with a mixed anaerobic flora consisting mainly of strains of Treponema and Fusobacterium with Prevotella intermedium and Porphyromonas gingivalis. The standard clinical symptoms of necrotising ulcerative gingivitis are severe pain, necrosis and ulceration of the interdental papillae with spontaneous gingival bleeding.
 Periodontal abscess with secretion of
pus − tooth 12
Periodontal abscess with secretion of
pus − tooth 12
Other often encountered symptoms are fever, poor general status, halitosis and lymphadenitis. Members of the armed forces with NUG are not fit for duty; they will require emergency dental treatment. The most likely locations are the front lower jaw and the posterior molars. The first objective of treatment is to eliminate the causative microorganisms. Because of the sensitivity to pain in acute cases, it is often not possible to provide professional cleaning of the teeth so that it is advisable to use cotton pellets to remove necrotic tissue and coatings. Also of benefit is the application of a 3 % hydrogen peroxide solution to the inflamed sections of the gingiva. This releases oxygen that is effective against the mainly anaerobic spectrum of microorganisms. Necrotising periodontal diseases can cause extensive irreversible tissue defects. The use of systemic antibiotics should thus be considered in particularly advanced cases. The administration of 750 - 1000 mg/day metronidazole for seven days has proved to be effective in view of the presence of the anaerobic microorganisms, while it is not advisable to use local antibiotics. This treatment can be accompanied by the co-administration or prescription of analgesics and the issue of a chlorhexidine digluconate solution for use as an antibacterial mouthwash by the patient at home. The patient should be given a daily appointment so that hydrogen peroxide (3 %) can continue to be applied until alleviation of symptoms and remission of the acute inflammation.
Periodontitis in association with endodontic lesions
Periodontal-endodontic lesions are pathological changes that affect both the periodontium and the endodontium. These are classified as
- primary endodontic lesions with secondary periodontal involvement
- primary periodontal lesions with secondary endodontic involvement
- genuine combined lesions
It is not always easy to distinguish between the various forms in differential diagnosis while the differential diagnosis of a periodontal abscess is itself not unproblematic. Sensitivity testing and radiological diagnosis are important in this context. There can also be acute exacerbation of periodontal-endodontic lesions, leading to the development of abscesses. For the acute therapy of these, a procedure similar to that described for periodontal abscesses can be employed. Trephination of devitalised teeth may also be necessary in cases of primary endodontic lesions. The appropriate form of subsequent therapy will be determined by whether the lesion is primarily endodontic or periodontal.
Active deployment: an aetiological factor?
 Extensive vestibular swelling in
association with a periodontal abscess at
tooth 15
Extensive vestibular swelling in
association with a periodontal abscess at
tooth 15
As stated above, bacterial plaque is the main causative factor in the development of inflammatory periodontal diseases. Bacterial plaque consists of a wide range of different microorganisms certain of which are routinely found in periodontal lesions and thus are considered to have a periodontal pathological potential. Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis and Tannerella forsythensis are considered to have a particularly marked pathogenicity. These periodontopathogenic microorganisms are also present in the oral cavities of individuals with a healthy periodontium where, however, they do not normally cause periodontal disease, apparently because the microorganisms are held in check by the immune response of the host. But this equilibrium can be disrupted. Long-term exposure to stress can result in changes to physiological parameters and the behaviour of those affected. What is designed as a short-term response by the body when threats appear can itself become a threat and a cause of illness if a stress situation persists over a longer duration. Depending on location and mission, the personnel of the Bundeswehr in the theatre of operations in Afghanistan are exposed to difficult and sometimes extreme conditions that mean that they are subjected to significantly increased psychological and physical stress. There are numerous stress factors that can generally be divided into universal and individual stress factors. The universal stress factors include sleep deficit, thirst and the extreme temperatures that can reach 50°C in summer. Examples of individual stress factors are homesickness, partnership worries, loss of comrades and the threat to own life and limb. The first
 Drainage of pus from the periodontal
pocket of tooth 15
Drainage of pus from the periodontal
pocket of tooth 15
three stress factors also impact on personnel who live in so-called 'secure' camps and who never actually leave the camp perimeters. To what extent the conditions of deployment are actually involved in acute exacerbation is still unclear; no corresponding studies of personnel in the field exposed to long-term and high levels of stress have been conducted. However, a correlation between the two seems plausible and can be assumed. This hypothesis is supported by the articles by Eger & Ferchland relating to the mission in Bosnia-Herzegovina in 2001 and a study by the same authors of the ISAF mission in 2008. Among other things, they examined changes to the microbial flora in the gingival sulcus of personnel of the German Bundeswehr serving with the ISAF. Although the changes to the investigated potentially opportunistic microorganisms registered in this study were not statistically significant, other aspects are of interest. The potentially periopathogenic microorganism Aggregatibacter actinomycetemcomitans was detected in only four subjects in the homeland; this had increased to 11 subjects in the theatre of operations. This could have been due to the proliferation of the microorganism, numbers of which were still below the detection limit while the subjects were at home. Another possibility is exogenic infection. This is an aspect that needs to be investigated in more depth in further studies.
Relevance to military medicine
A not insignificant proportion of cases of dental treatment required in the theatre of operations − 18.65 % − became necessary due to periodontal disease. However, details of the periodontal diagnoses in these cases are not available. It is important to bear in mind that not all these cases will have involved the serious acute forms of periodontal disorders discussed above. As I know from my own experience, these disorders do occur in personnel on active duty, but the exact prevalence remains uncertain. At the same time and because of the potentially serious complications associated with acute inflammatory periodontal disease, these disorders must be considered to be of major relevance in the context of military medicine. It can be assumed that the disorders dealt with during most of the treatment sessions were less serious and took the form, for example, of simple gingivitis. It would thus be desirable to have a more differentiated breakdown of the statistics. It is
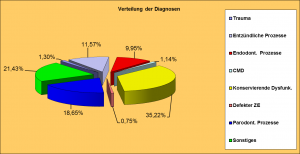 Emergency dental treatments provided during all tours of duty in 2012 by type
Emergency dental treatments provided during all tours of duty in 2012 by type
important to continue to apply the principle that only orally and periodontally healthy personnel are fit for active duty. The prophylaxis programme designed to prepare personnel for deployment that was developed and implemented by the dental service of the Bundeswehr recognises this principle and needs to be maintained. It may also appear advisable to provide professional dental cleaning services to personnel in the field. However, as long as there is no clear clinical evidence that demonstrates that this is necessary, the allocation of additional personnel and resources for this purpose cannot be justified. For the sake of completeness, I should like to briefly outline an aspect for which there is currently no relevant data. Enossal implants are increasingly being used in Bundeswehr personnel in order to provide a basis for replacement teeth. As in the case of a tooth, the tissue around such an implant can become inflamed; this is called periimplantitis. It would be interesting to find out whether conditions in a theatre of operations and the associated stress factors also play a role in the development of periimplantitis.
Author's address:
Lt. Colonel Dr. Michael Lüpke
Director of the Specialist Dental Treatment Centre
Hamburg Bundeswehr Hospital
Lesserstraße 180
Date: 01/03/2019
Source: Medical Corps International Forum (4/2014)











