

Article: Shreshth Dharm-Datta, J McLenaghan
Medical lessons learnt from the US and Canadian experience of Treating Combat Casualties from Afghanistan and Iraq
The Winston Churchill Memorial Trust, established in 1965, funds Travelling Fellowships and both authors visited hospitals in Germany, Canada and the USA regarded as centres of excellence with expertise in the early care, reconstruction and rehabilitation of the combat casualties of our NATO Allies, as recipients of these Fellowships. This article presents some of the lessons learnt in the field of musculoskeletal trauma and rehabilitation from the Canadian and US military medical systems. In trauma, there were significant differences in wound debridement policy, use of external fixators for fractures, primary use of circular frames for open tibial fractures and a far more liberal use of bone morphogenetic protein in fracture treatment. Differences in soft tissue reconstruction policy regarding flaps for soft tissue cover over exposed bone, near-universal usage of topical negative pressure dressings and use of Allgöwer-Donati suture pattern to close all wounds were noted. Ertl amputation osteoplasty, a modified form of transtibial amputation, had also been reintroduced. In rehabilitation, the management of heterotopic ossification, in particular with imaging techniques and excision surgery, was identified. For the upper limb, we observed the patient training required to use a myoelectric hand and the future possibility of targeted muscle re-innervation to make controlling these myoelectric prostheses more natural using innate motor patterns. For the lower limb, we found we used identical above knee prostheses. For patients who have had limb reconstruction and have poor function, an energystoring orthosis was demonstrated to compensate for the loss of range of motion and muscle power.
Introduction
The Winston Churchill Memorial Trust1 was established in 1965 on Sir Winston Churchill’s death with thousands of people paying into a public subscription as a living memorial to him. The income from this original investment has allowed the Trust to fund 100 Travelling Fellowships and 10 bursaries at Churchill College, Cambridge, every year since 1966. This Fellowship is open to all British citizens resident in the UK and allows Fellows to travel abroad and learn lessons that can be brought back to benefit future generations of British people. In 2009, the Medical and Health category title was the ‘Treatment and Rehabilitation of Traumatic Injuries’. The authors were recipients of this prestigious Fellowship and chose to follow the themes of musculoskeletal trauma and rehabilitation visiting the orthopaedic and rehabilitation departments of the main military and civilian hospitals treating combat casualties from the US and Canadian Armed Forces. Over a 10-week period, the US military hospital in Landstuhl Regional Medical Center (LRMC), Germany, the University of Alberta Hospital and Glenrose Rehabilitation Hospital in Edmonton, Alberta, Canada, the two major centres of US military care at the Walter Reed Army Medical Center/National Naval Medical Center (WRAMC/NNMC) in Washington DC/Bethesda, Maryland, and the Brooke Army Medical Center (BAMC) in San Antonio, Texas, were visited. The aim was to learn lessons from their experience of treating combat casualties and exchange ideas from our experience of the Royal Centre for Defence Medicine (RCDM) Birmingham and Defence Medical Rehabilitation Centre (DMRC) Headley Court. Our experience from this Fellowship, some of the lessons learnt and the problems faced in common with our NATO Allies are presented.
Educational points
▪ It is a US medical policy to wash out wounds every 48 h and use monolateral external fixators on all fractures. The UK has a more liberal policy on subsequent wound debridements and immobilisation for aeromedical transfer.
▪ Bone morphogenetic protein-2 is used far more liberally in the USA, without necessarily the evidence base to substantiate its use.
▪ The Ertl amputation osteoplasty has no real benefits over conventional transtibial amputation.
▪ Early heterotopic ossification (HO) excision (after CT to guide maturity) can be performed without recurrence, using appropriate prevention treatment.
▪ Myoelectric limbs with targeted muscle re-innervation may be the future of upper limb prosthetics.
▪ All three countries use the same C-leg prosthetic knee for above knee amputees.
▪ Keeping patients motivated with limb reconstruction is challenging and patients may ask for elective amputation; the development ofthe Intrepid dynamic exoskeletal orthosis (IDEO) energy-storing ankle foot orthosis may change attitudes towards persisting with reconstruction treatment.
Patient Care Infrastructure
UK combat casualty care
When UK service personnel are injured in combat in Afghanistan, they receive immediate first aid from other members of their team and are evacuated to the Role 3 British Military Field Hospital based at Camp Bastion (or Basra during the war in Iraq). Once stabilised and the immediate threat to life has abated, all casualties are aeromedically transferred to Role 4 at RCDM Birmingham for definitive surgical treatment. RCDM is established at the civilian University Hospitals Birmingham National Health Service (NHS) Trust, which comprised Selly Oak and Queen Elizabeth Hospitals, and as a university teaching hospital has all specialities available.
Selly Oak Hospital closed in 2010 and all facilities are now located at the Queen Elizabeth site. DMRC at Headley Court provides the single point of referral as the Role 4 Tri-Service Unit for neurological, musculoskeletal and amputee rehabilitation. On discharge from RCDM Birmingham, all patients are referred to DMRC for rehabilitation and the more severely injured or amputee patients are admitted directly as inpatients. All amputees are referred to the on-site Prosthetic Limb Fitting Service. To facilitate communication between the various units treating injured patients, there is a weekly ‘Joint Theatre Clinical Case Conference’ teleconference among the R3, R4 units and Aeromedical Cell for feedback and discussion.
Since 2010, Service personnel not expected to return to full duty with 6 months are moved from their combat units to one of the 11 regional Personnel Recovery Units. They are allocated a Personnel Recovery Officer who works with them to facilitate their return to duty or transition to civilian life. Personnel Recovery Centres run in partnership with the charities Help for Heroes and The Royal British Legion are based at Edinburgh, Colchester, Tidworth, Catterick, Plymouth and Sennelager, Germany, and provide additional welfare support, vocational and sporting activities for recovering personnel.
US facilities
The US military retains military hospitals to care for combat casualties. Their term ‘Echelon’ of care reflects the UK term ‘Role’, such that E1 is R1 and so on. Geographical distance from the field hospitals to the Continental United States of America (CONUS) necessitates a stop off point in mid-Europe for aircraft refuelling and the Echelon 4 facility at Landstuhl in Germany, near the United States Air Force base at Ramstein, is a Level 2 trauma facility to stabilise and treat patients prior to the long transatlantic flight to CONUS. In CONUS, there are three Echelon 5 hospitals that equate to UK Role 4 for combat casualties: WRAMC/NNMC, BAMC and the Naval Medical Center San Diego. WRAMC closed in 2010 and combined at the Bethesda site to form the tri-service Walter Reed National Military Medical Center. Patients are sent to these depending on whether they are originally stationed on the East, South or West Coast, respectively, with all burns patients sent to the military burns unit at BAMC.2 The rehabilitation facility at the WRAMC site is named the Military Advanced Training Center (MATC), at BAMC the Center for the Intrepid (CFI), and the Comprehensive Combat and Complex Casualty Care (C5) facility is at Naval Medical Center San Diego.3 4 There is also a weekly video conference among the E3, E4 and E5 units for feedback and discussion.
Warrior Transition Units (for Army) and Wounded Warrior Regiments (for Marines) were established in 2007. These aim to coordinate the rehabilitation needs of Service personnel for those out of acute care and deemed to need greater than 6 months rehabilitation within a Service ethos. Personnel are posted to these WTUs and WWRs, which are distributed throughout the country at hospitals and large bases, with polytrauma and amputee rehabilitation concentrated at the MATC, CFI and C5 WTUs/WWRs.
Canadian facilities
Canada provided the personnel for the Role 3 hospital at Kandahar Air Field from 2006 to 2011. Canadian combat casualties are repatriated via LRMC to Canada using US aeromedical assets. The Canadians have no military hospitals in their country, and all care of combat casualties is performed in civilian institutions funded through a social healthcare model, akin to the NHS. Due to geographical considerations, repatriated Service personnel do not go to one central hospital, but are distributed to major hospitals near where they are stationed or where their families are based and enter a civilian hospital system for complete casualty care from acute surgery to rehabilitation. Only when they are discharged from the civilian rehabilitation hospitals to the Base do they re-enter the conventional military primary care and physiotherapy setup. As there are no military hospitals, secondary care medical and nursing staff are placed in civilian Level 1 trauma centres to work when not deployed.
Trauma
Wound debridement
All open wounds are irrigated and debrided every 48 h in the initial phase. This frequency is reduced to every 72 h after three to four washouts of the wound and provided that the wound is clean, but continues till closure. Pulsed lavage is only used on relatively clean wounds in the initial phase or after several washouts when the wound is clean and free of visible debris and is not used in new and dirty wounds due to driving debris, dirt and bacteria further in.
Initial fracture management
Monoplanar external fixators are used on all open fractures in the field hospitals and this is a US military medical policy.8 The use of traction or plaster cast immobilisation is not used, unlike UK policy. Large bone deficits are filled with antibiotic laden cement beads acting as a spacer to control dead space and manage bacterial levels in the CONUS hospitals.
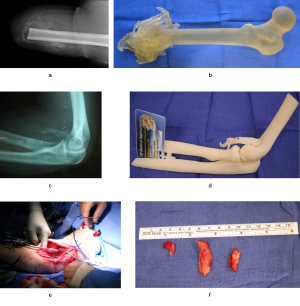
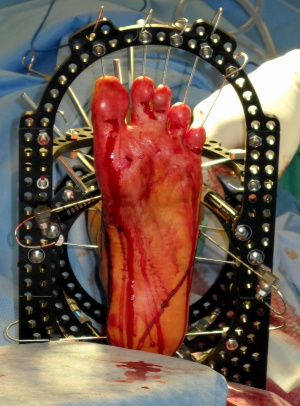
Open tibial fractures
Open tibial fractures, particularly Gustillo Anderson Grade III, present a challenge. The US military surgeons prefer conversion of the monolateral external fixators to definitive circular external fixators using Ilizarov techniques rather than internal fixation in E5 hospitals. The Taylor spatial frame (TSF) (Smith & Nephew, Inc., Memphis, Tennessee, USA) has evolved into their workhorse circular external fixator as the first-line device used. Some issues with using the TSFs have been resolved. Ankle equinus or toe clawing (the latter possibly from missed foot compartment syndrome with Volkmann ischaemic contractures) was prevented by the use of fine axial wires along the length of the toes to hold them extended and prevent ankle plantarflexion. This is coupled with the use of a foot plate to allow the patient to fully weightbear in the TSF (Figure 1C).
Bone graft and bone morphogenetic protein
In open fractures with segmental bone loss, bone graft (synthetic, allograft or autologous) was not used acutely due to the risk of this becoming infected and acting as sequestrum. In the early management of these fractures, bone morphogenetic protein-(INFUSE, Medtronic, Memphis, Tennessee, USA) soaked on collagen sponge was used at the fracture site. If bone grafting was required, this was performed as a delayed separate procedure at a later date.
Soft tissue reconstruction
The US military surgeons have found that free flaps have high failure rates in the presence of infected wounds, which the majority of combat casualties will have. Rotational (pedicled fasciocutaneous and muscle) flaps have had more success and are being used more to cover the soft tissue defects in limbs.10 We noted that US military plastic surgeons were more involved in the treatment of maxillofacial trauma, so unlike UK practice, fasciocutaneous and pedicled gastrocnemius flaps were done by the orthopaedic trauma specialist, while free flaps were performed by the orthopaedic hand surgeons experienced in microvascular surgery. If the flap was too small to cover the soft tissue defect or the vascular pedicle would not let it reach the area (eg, distal third tibial wound), the TSF could be used to reduce the distance requiring soft tissue coverage by shortening or angulating the fracture within the frame, covering the defect with the pedicle flap and progressive correction of the long bone and stretching its soft tissue cover over several months.
Wound closure
When the wound was clean and suitable for closure, the modified Allgöwer-Donati suture pattern was used. This has the least disruption to microvascular cutaneous blood flow, and hence theoretically the least likely to result in ischaemic skin flap necrosis and wound breakdown.
Topical negative pressure dressings
Vacuum assisted closure (Kinetic Concepts, Inc., San Antonio, Texas, USA) dressings are used on all open wounds at the Echelon and hospitals. These are often first applied in the field hospitals for wound exudate and management issues for aeromedical transfer and this dressing therapy will continue throughout the patient’s treatment till final wound closure. The use of an ‘incisional’ vacuum assisted closure dressing applied for delayed primary closure was common, especially on lower limb injuries. This involves placing a thin strip of the black GranuFoam polyurethane foam along the sutured wound closure line to allow wound exudate management and prevent skin maceration.
Modified Ertl procedure
Ertl developed his amputation osteoplasty in 1920, which took a corticoperiosteal flap from the tibia and secured it to the fibula to provide an osseous union between the two. In a normal below knee amputation, the limb prosthesis transfers all its load onto the proximal tibia and patella tendon. The tibio-fibular synostosis creates a more rigid, broad distal limb to allow sharing of the loadbearing with the end, similar to the end-bearing stump of a through-knee amputation. The originator also believed that loading the distal portion of the tibia could prevent disuse osteoporosis of the tibia, fibular instability and pain. A modified version has been reintroduced for selected patients at WRAMC. This uses a fibular strut graft hinged to form the bone bridge that docks into the tibia and a screw or TightRope (Arthrex, Inc., Naples, Florida, USA) to hold the synostosis. However, a review of their results disputes some of these benefits with a higher complication rate in modified Ertl versus conventional transtibial amputations.
Prosthetics and Rehabilitation
Heterotopic ossification

Potter et al and Forsberg and colleagues16 reported that around 60% of US combat amputees had heterotopic ossification (HO) present in the stump, with nearly 10% requiring surgical excision due to pain, ulceration and prosthesis fit issues in spite of conservative measures such as changing the socket and/or liner, rest and painkillers. A comparative study of UK and US combat amputees found similar prevalence, although the severity was lower in the UK group. HO excision too early has a high risk of recurrence. We observed that the US policy was for relatively early excision of the HO after a minimum of 6 months after injury. CTwas used to gauge maturity of HO; if the HO was corticated, it was gauged to be mature enough to be excised. In contrast, UK policy had been to wait a minimum of 18 months and use technetium-99 isotope bone scan to see if the HO was ‘cold’ and metabolically inactive.
Recurrence was prevented using 700cGy irradiation in a single fraction and/or a 6-week course of celecoxib (non-steroidal antiinflammatory), depending on preoperative severity (eg, both would be used in traumatic brain injury patients with HO). In the 60 excisions they had done by the time of our visit, they had no symptomatic recurrences.
CT data for computer aided design/computer aided manufacturing model
The use of CT to gauge maturity of HO also allows the production of computer aided design/computer aided manufacturing models.19 This allows the physiotherapist and prosthetist to localise symptomatic areas and take efforts to avoid irritation by modifying the socket or appropriate padding. It also aids surgical planning of the excision and avoiding neurovascular structures which may pass through the area of distorted anatomy. Figure 4 demonstrates HO arising in the cubital fossa, near the neurovascular structures that pass anterior to the elbow joint. The model allowed the surgeons to rotate the model and plan their approach to excise the HO fragments without compromising essential structures.
Upper limb prosthetics
Overall, 20% of both the US and UK military amputees have upper limb amputations.20 21 Conventional mechanically operated upper limb prosthesis have poor compliance and usage. The myoelectric prostheses i-Limb and ProDigits (Touch Bionics, Livingston, UK) provide an artificial functional hand or fingers respectively that can be controlled by myoelectric signals. Sensors pickup the transcutaneous electromyographic signal from muscles innervated by their respective motor nerves and a microprocessor-controlled system converts this into control of the myoelectric hand’s motors. For an amputee, electrodes must be placed on alternative proximal muscles such that opening the hand could be controlled by triceps contraction (proximal radial nerve), closing the hand by biceps contraction (musculocutaneous nerve) and switching to wrist rotate mode is by biceps and triceps co-contraction. A period of training is therefore required to learn to control a myoelectric hand.
Targeted muscle re-innervation
It would be more intuitive and require less retraining for the amputee to use the original nerves that provide motor control of the hand, that is, the median, ulnar and distal radial nerves to control the myoelectric prosthesis. The challenge is obtaining a transcutaneous electromyographic signal directly from these nerves as their innervated muscles were removed with the amputation. Research by Kuiken and Dumanian using targeted muscle re-innervation aims to resolve this. The amputated peripheral nerves are rerouted from the brachial plexus to a unique part of the pectoralis major and serratus muscles or biceps and lateral triceps (depending on level of humeral amputation). The new host muscle is selectively denervated from its normal motor nerve and then re-innervated with these distal nerves, with overlying subcutaneous fat also removed to improve electrical conduction. The re-innervated muscle amplifies the electrical signal of the amputated motor nerve and electrodes placed over the corresponding patch of skin supply this to the myoelectric prosthesis. This allows finer control of the prosthesis using innate motor patterns and improved dexterity.
Lower limb prosthetics
The pneumatic postamputation mobility Aid (Ortho Europe, Abingdon, UK) is used in the UK to mobilise amputee patients early before the distal wounds of the amputation have healed. It works by inflating to form a collar around the residual limb to provide support along its length, without touching the distal end. This is only a temporary ‘prosthesis’ but allows UK amputees to walk upright very early before a socket/liner could be fitted to the residual limb. The US and Canadians therapists do not use this and their amputees mobilised relatively late when the wound had healed to allow socket/liner fitting. Prostheses for above knee (transfemoral) amputees involve replicating a knee joint. The standard issue prosthetic knee is the microprocessor-controlled C-leg (Otto Bock GmBH, Duderstadt, Germany) among the UK, US and Canadian military amputees. The next generation C-leg named X-2 (commercial/civilian version is the Genium knee) by Otto Bock was being trialled in select patients at the MATC during our visits but the improvements from this more expensive prosthesis were not sufficient to change the standard issue knee.
Salvaged limbs and late amputation
Patients with a reconstructed lower limb may have deficits in strength due to muscle loss from debridement, poor range of motion from scarring or primary joint fusion for unreconstructable articular fractures, lack of stability, nerve damage or pain with attempts at higher intensity activities. The patient may be able to walk on level ground but uneven ground, inclines or running is not possible.
Some patients therefore request late elective amputations as they feel the function they would obtain from a below knee prosthesis is greater than what they achieve with their native reconstructed leg. The prevalence of late (>3 months) amputations for US combat casualties who undergo lower limb reconstruction is 15%,26 comparable with 10% for UK.25 Reasons given by these patients include neurological dysfunction, persistent or recurrent infection, neurogenic pain, non-neurogenic pain, fracture non-union or malunion, soft tissue breakdown and globally poor functional result. Furthermore, limb reconstruction patients rehabilitate in the same facilities as amputees and there is a culture of acceptance of amputation within this population. Patients in the reconstruction group become frustrated with their slow progress, prolonged rehabilitation, repeat hospitalisations and complications, comparing themselves with the early success of many amputees returning to function.
Therapy strategies include early hydrotherapy in the TSF, early normalisation of movement patterns and complex movement patterns which incorporate balance and proprioception; additionally, integrated weightbearing protocols encouraging the patient to put as much weight through the limb as possible while in the TSF help healing and compliance with reconstructive treatment.
Energy-storing ankle foot orthosis

The CFI/BAMC team have a custom-designed orthosis to fit over the reconstructed lower leg called the IDEO.24 This stores energy on the loading response, mid-stance and terminal stance phases of the gait cycle in a stiff but elastically deformable carbon fibre strut, and releases it under relative control on pre-swing (toe off ). The idea is to reduce the effort of pre-swing by storing some of the energy normally dissipated during stance phase by eccentric muscle contractions as the ankle dorsiflexes (indeed these muscles may no longer be present). In the IDEO, therapists teach running re-education to encourage mid-foot strike and lessen impact on the calcaneum.
Subjectively the patients report improved functional abilities on variable walking speeds, improved stability, agility, accommodation of uneven surfaces and running. The original trial prosthesis we saw has been modified and its results reported in 2011. Those authors have had seven patients actively deployed in military combat duties using the IDEO system. Such a device is essential in persuading lower leg reconstruction patients to persist with their treatment and resist the lure of late amputation, knowing that they can match if not outperform amputees with a transtibial prostheses while retaining their leg.
Expansion at DMRC
Prior to 2006, there were only 36 beds at DMRC for inpatient rehabilitation, and military amputees were referred to local NHS Limb Fitting Centres for prosthesis provision which was often inconsistent, slow and limited by local NHS financial pressures. Increased government funding allowed the establishment of the military Limb Fitting Centre at DMRC and in the 6 years that it has been open has become the largest purchaser of C-legs in the UK. Further charitable donations have allowed improvements in infrastructure and facilities such as the swimming pool, gait lab and clinic space in The Help for Heroes Rehabilitation Complex opened in 2010. The Jubilee Complex was completed in 2012 with further Ministry of Defence funding and increased the inpatient rehabilitation provision to 96 beds (with ability to expand to 144) and a dedicated polytrauma therapy building.
Visits by medical and allied health staff to the USA and Canada helped steer the improvements needed at DMRC.
Conclusions
The management of limb reconstruction or extremity amputation followed by rehabilitation in this young, fit and previously highly active population presents as much of a challenge to our US and Canadian Allies as it does in the UK. Our overall impression was that the UK was doing as well as our peers. Trauma management was similar for most injuries with some differences noted. The USA and Canada have more technologically sophisticated solutions for rehabilitation. However, with the improvements to DMRC Headley Court since 2010, we can offer a similar level of treatment to our patients.
Acknowledgements The authors would like to acknowledge the contribution of Maj Raymond Anakwe RAMC for his assistance in preparing the original podium presentation on which this article is based. The full reports submitted to the Winston Churchill Memorial Trust are available at their website. We would like to sincerely thank the Winston Churchill Memorial Trust for enabling us to travel so extensively to see firsthand how our main NATO Allies care for their combat casualties at these world-renowned hospitals. Furthermore, we would like to encourage future military applications to the Winston Churchill Memorial Trust for travelling fellowships and to bring back lessons to help others. We would also wish to express gratitude to our kind hosts: Captain Eric Pagenkopf MD and Lieutenant Colonel Raymond Fang MD at LRMC; Lieutenant Colonel Robert Stiegelmar MD at the University of Alberta Hospital and Dr Jacqueline Hebert MD at Glenrose Rehabilitation Hospital; Lieutenant Colonel Romney Andersen MD at WRAMC and NNMC; Major Joseph Hsu MD, Colonel Jennifer Menetrez MD, Ryan Blanck, Johhny
Owens PT and Major Terry Fee PT at BAMC and CFI. Funding The Travelling Fellowships were funded by the Winston Churchill Memorial Trust.
References: [email protected]
Date: 02/11/2019
Source: Medical Corps International Forum (4/2013)











