
Report: Diana Elisa Gomes Correia, José João Baltazar Mendes
The Influence of Type 2 Diabetes Mellitus on Periodontal Disease
Portuguese Armed Forces Hospital – Dental Service
The epidemiological association between PD and DM results from a direct causal relationship in which the complications of DM act as modifiers of the expression of PD and vice versa. The aim of this study is to investigate the influence of DM2 in the development of PD in a Portuguese
population. Patients are followed in the Armed Forces Hospital by the Dental Medicine Department and the Endocrinology Department.
Introduction

Periodontal disease (PD) is a chronic inflammatory disease, primarily manifested by an oral infection by anaerobic gram-negative bacteria, and consequently leads to gingival inflammation, destruction of periodontal tissues and, if not treated, leads to tooth loss. It is estimated that 10% -15% of the world adult population and 60% of individuals older than 60 years suffer from PD.
Diabetes Mellitus (DM) is a disease whose complications are the leading causes of morbidity throughout the world. Worldwide there are about 285 million people with Diabetes Mellitus (DM) and Portugal is one of the countries with the highest prevalence of DM in Europe, 12.4% of the Portuguese population (between 20 and 79 years) have diabetes. The nondiabetic individuals with PD are at greater risk of developing insulin resistance and T2DM.
The relationship between PD and diabetes mellitus (DM) is widely accepted. DM is a major risk factor of PD and patients with type 2 DM (DM2) are more likely to develop this disease compared to healthy controls, approximately threefold.
The epidemiological association between PD and DM results from a direct causal relationship in which the complications of DM act as modifiers of the expression of PD and vice versa.
The aim of this study is to investigate the influence of DM2 in the development of PD in a Portuguese population. Patients are followed in the Armed Forces Hospital by the Dental Medicine Department and the Endocrinology Department.
Methods
Single center, randomized trial with 90 T2DM patients. In the day of the evaluation, an Endocrinologist and a Dentist observed all patients. Biometric parameters were measured and blood analyses were carried out for HbA1c, HDL, LDL, Triglycerides and glucose. Periodontal clinical parameters were measured by a computerized periodontal probe. PD was classified according to clinical attachment loss (CAL): initial (CAL 1-2mm), moderate (3-4mm) and severe (³5mm). Exclusion criteria: chronic renal disease;pregnancy; antibiotics (last 3 months); hemoglobinopathies; bleeding disorders; less than 3 teeth; periodontal treatment (last 6 months) and smoking habits. Chi-Square Tests and Multivariable Regression analyzed variables with a significance level of 5%.
A total of 90 individuals were observed: 70 male (77,8%); 20 Female, mean age of 64,3 years (± 9,95), BMI of 29,1kg/m2 (±4,42), waist measure of 103,4cm, HbA1c of 6,69% (±0,95), T2DM was diagnosed for 11,3 years (±8,66), and 84% had Dyslipidemia. Patients had in average 21,4 teeth (±7,1), 98,1% of teeth had bleeding on probing, 11,1% had suppuration and 100% had dental plaque. CAL ranged from 0 to 11 mm. PD was present in 98% of T2DM patients: 55% had initial PD, 30% moderate and 15% severe.
Results
A total of 90 individuals were observed: 70 males (77.8%); mean age of 64.3 years (G9.95), BMI of 29.1 kg/m2 (G4.42), waist circumference of 103.4 cm, HbA1c of 6.69% (G0.95), T2DM was diagnosed for 11.3 years (G8.66), and 84% had dyslipidemia. Patients had in average 21.4 teeth (G7.1), 98.1% of teeth had bleeding on probing, 11.1% had suppuration and 100% had dental plaque. CAL ranged from 0 to 11 mm. PD was present in 98% of T2DM patients: 55% had initial PD, 30% moderate and 15% severe.
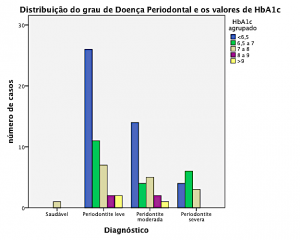
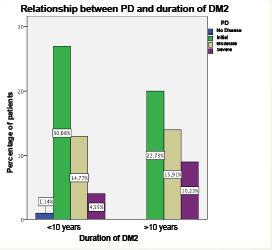
We found an association between metabolic control (HbA1c) and the duration of T2DM with the severity of PD (p<0.001 and P=0.05).
From multivariable analysis it was found that regardless metabolic control, diabetic patients had a higher risk of developing PD if they were obese (P<0.001) or had dyslipidemia (P<0.025).
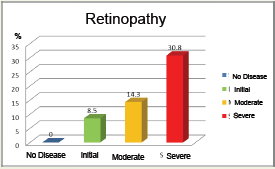
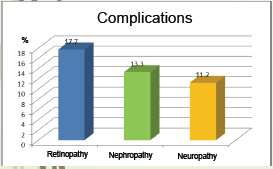
Retinopathy was the complication more frequent present in these patients and it was related with the severity of PD (p=0,042).
Conclusion
We conclude that patients with T2DM had a high prevalence of PD. Susceptibility to PD is increased in patients with poor glycemic control and with longer duration of DM2. Obesity, high waist circumference and dyslipidemia are risk factors for PD, independently of glycemic control.
Patients with DM2 should be referenced to Dental Medicine in order to PD be diagnosed and treated early. The Dentists should refer the patient with PD to their doctor in order to be done a DM screening.
The implementation of screening and multidisciplinary therapeutic approach of these patients in the military programs, also contributes to improved health in our forces and a reduction in expenses of the disease.
In this sense the Armed Forces Hospital becomes a privileged institution since due to present a service of Dental Medicine hospital, almost unique condition in Portugal, allows in conjunction with the service of Endocrinology and Laboratory analyzes create a favorable environment for clinical development of a single study in the country.
Date: 04/25/2019
Source: Medical Corps International Forum (2/2016)











