
Article: Tom Verhofstadt
Prevalence of Periodontal Disease among Belgian Military Rapid Deployment ISTAR Battalion

ISTAR Bn in action (source: Belgian Defence/Istar Bn)
INTRODUCTION
Periodontal screening is an essential and integral part of the dental examination process. The prevalence of periodontal disease is assessed through epidemiological indexes that measure the periodontal health of a population, which allow us to formulate strategies for prevention, control and reduction of the disease. Early detection and diagnosis before the age of 40 are key elements in the prevention of this oral pathology (18).
Prevention is an essential pillar to reduce the number of urgent periodontal interventions in military missions.Problems arising from poor gingival and periodontal health in military personnel account for around 10% of the emergencies of oral origin during deployments and maneuvers (1).The aim of this study was to estimate the prevalence, extension, and severity according to the 2017 Chicago Workshop (2). In this case, we like to compare our results with other (military) prevalence studies. With our data we can also make comparisons with indices that are used in many (older) studies. For biofilm calculation, the most frequent index used is the Silness and Löe plaque index (3).
Materials and Methods: This was a cross-sectional observational prevalence study which analyzed the periodontal condition during the dental annual check-up according STANAG 2466 to make military personnel dentally fit. The study population of 107 military personnel are part of the Belgian ISTAR battalion between 19 and 35 years of age. ISTAR stands for intelligence, surveillance, target acquisition and reconnaissance. Most of these soldiers are younger than 35 years old. The study took place during autumn/ winter of 2023.
Before the periodontal examination, participants filled in a self-administered questionnaire that included several epidemiological variables such as age, educational level (secondary, college, university), smoking status; current regular smoker with more than 10 cigarettes per day, occasional smoker up to 10 cigarettes per day and nonsmoker, oral hygiene habits like toothbrush frequency, usage of dental floss/interdental brushes.The periodontal clinical data obtained from the automatic 3rd generation periodontal probe Pa-on (Orangedental) included: number of absent teeth, pocket depth (PD), gingival recession (REC) as the distance from the enamel-cement junction (CEJ) to the free gingival margin, bleeding on probing, plaque index (PI) and bone loss index (BL). As a resume, prevalence was estimated by calculating the Community Periodontal Index (CPI).The exclusion criteria were pregnant women, sick military, and military personnel under 18 years and over 35 years old and military personnel who had a previous periodontal treatment, conservative or surgical, within the previous six months. Wisdom teeth were excluded from the study.
All the parameters were scored by one experienced military general practitioner, to avoid interexaminer bias. For the determination of the plaque index and bleeding on probing, all four surfaces of all teeth (mesial, buccal, distal, oral) were scored. For PD, four sites were measured at every tooth (mesio-buccal, disto-buccal, disto-oral and mesio-oral).
Ethical consideration: The present study was conducted in full accordance with ethical principles and was reviewed and approved by the Medical Ethics Committee of the Brugmann Hospital (Ref.:B0772023000065). All participants were informed about the evaluation to which they were submitted and gave their informed consent for participation.
Measurement rehabilitates: Until now, manual probing is the ‘golden standard’, but has certain limitations due to interindividual varying pressures while inserting the probe, different inflammatory conditions of the gingival tissue, wrong angulation of the probe, as well as errors while reading the scale or transferring measurements in the dental record. The third generation electronic ‘Pa-on’ periodontal probe (Orangedental, Germany) was used as a measuring instrument as it provides greater precision and accuracy in periodontal screenings (4). The Pa-on probe is computer-based, electronic and pressure-calibrated, measurement and calculated the insertion depth with a thin steel tip with a plastic cover at 20 g/0.2 Newton pressure using resistance. Due to a computer-measuring-sequence, tooth-to-tooth data is recorded on a chip and transferred wireless to a periodontal chart. Standard manual probing and the use of an electronic probe correlate very well, albeit PD measurements showed a statistically significant difference, which was below a measuring error of 1 mm (4).
Cases Definition: Until 2017, there was not a clear consensus about the clinical criteria to be used in defining periodontal disease (5). In 2013, WHO introduced the modified CPI (Common Periodontal Index) to reduce weaknesses of the CPI. This index recorded the presence or absence of bleeding and periodontal pockets and attachment loss of all teeth. Bleeding on probing is the most objective indicator to assess gingivitis (6).The European Federation of Periodontology (EFP) and American Academy of Periodontology (AAP) in Chicago in 2017 developed case definitions for periodontal procedures to facilitate the uniformity of the data collection around the world and to avoid disparities related to different assessments of periodontal variables (2,15). However, there is still limited data from epidemiological studies that adopt these diagnostic criteria (7).A non-periodontitis person in our survey is defined for epidemiological purposes as following:
1. Healthy person: ≦10 % bleeding sites with probing depths(PD) <3,5 mm. A CPI score 0 or 1 was recording (6).
2. Gingivitis is defined as >10 % bleeding sites with probing depths of <3,5 mm. A CPI score between 1 and 2 wasrecording.
A periodontitis person is defined as following:
3. Staging of mild periodontitis or stage I periodontitis wasmeasured by calculating interproximal sites between ≦3.5mm PD and <5.5 mm PD or calculating a CPI score of 3.
4. Moderate periodontitis or Stage II was measured by calculating at least 2 interproximal sites on two or more teeth withPD of ≦5.5 mm or a CPI score of 4.
5. Severe periodontitis or stage III was measured by calculatingthe mean of bone loss (BL) of >4 mm or loss of 4 teeth or a PD≦6 mm on at least one tooth and recording a CPI score of 4.
Plaque index (PI) (3). This index is used to identify high-risk patients and monitor the patients ́ oral hygiene and patient compliance over time. PI is determined dichotomous in all quadrants. Bleeding on probing (BoP) and Plaque Index (PI) are simple options that record both the presence of disclosed plaque (biofilm) and the presence of bleeding in a dichotomous manner. Both indices focus on interproximal areas that was in general plaque retentive and susceptible to inflammation (13).
Bleeding on probing is determined by putting the Pa-on probe within the gingival sulcus together with measuring the pocket depth of the papilla from both sides, buccal and lingual. After 20 seconds, the results should be recorded dichotomous as “+ if there is bleeding” or “- in the absence of bleeding” for every of the four areas of the tooth.
To compare our results with other studies, we calculated the most frequent CP index researchers used in their surveys. The modified CPI or in Belgium the “Dutch Periodontal Screening Index” (DPSI) to analyze the periodontal condition. It is a simple, effective system to detect periodontal disease. CPI scores provides detailed information about the condition of a patient’s periodontium and allows a quick and comprehensive evaluation of the periodontal condition. With the CPI even the earliest symptoms of periodontal disease can be detected clinically. The possible findings are summarized in the codes 0 to 4. The pathological cut-off determined by the WHO for probing depth was set at 3.5 mm. The highest pocket depth score for each quadrant was calculated. Teeth that are evaluated: all existing teeth, except the wisdom teeth. The mouth is divided into sextants (17-14, 13-23, 14-27, 37-34, 33-43 and 44-47) A sextant is only examined if there are at least 2 teeth, and they are not intended for extraction due to caries. A sextant with only one or no tooth is recorded as toothless. Only one finding is made for each sextant, i.e. only the tooth with the greatest pocket depth per sextant is noted. CPI scores 3 and 4 distally of the second molars were not taken into consideration, to avoid a false-positive finding due to pseudo-pockets, which often occur in this region.
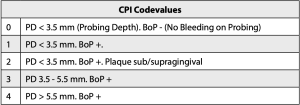
Table 1: CPI Codevalues 0 – 4
Statistical Analysis: The data was analyzed using www.medcalc.org, Belgium. Descriptive statistics were calculated: numbers, percentages, means and standard deviations of quantitative variables, proportions of qualitative variables. Logistic regression analysis was performed to model the relationship between the extent and the severity of periodontitis and co-variables as potential risk indicators. The odds ratio (OR) and their 95% confidence intervals (CI) was calculated. The level of statistical significance was set at P<0.05.
The results found in the study was compared with other prevalence studies in a military or civilian population with approximate the same age.
RESULTS
Sociodemographic Data: The sample consisted of 107 military participants. Sociodemographic data of the study participants are shown in table 2. Ninety-three percent of the subjects were males. Only 2 participants had a systemic disease and none of the soldiers had missing teeth due to periodontitis. All the soldiers attended formal education. The majority (89 %) stopped after secondary education (normally in Belgium at 18 years). The mean age of the participants was 25.98 years (SEM=0.43; SD=4.41).
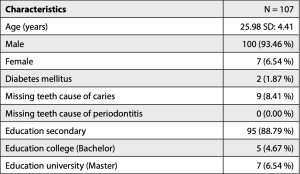
Table 2: The Sociodemographic Characteristics of the Study Participants (n=107)
Prevalence and Severity of Periodontal Disease: The Clinical Characteristics of the military participants are shown in table 3. 25.23 % of the participants had more than 5 mm in depth on one or more teeth. None of the participants had pockets more than 6 mm. More than half of the subjects had gingival recessions (53.27 %).
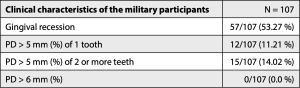
Table 3: clinical characteristics of the military participants.
The periodontal status of the participants is show in table 4. The mean probing depth was 2.52 mm (SD= 0.50) and the mean bleeding on probing was 17.72 % (SD= 35.94). About half (48.60 %) of the participants are clinically healthy (less than 10% bleeding on probing).
Periodontal Pockets were divided into 4 categories corresponding with the periodontal screening index. 42 of the military participants have according to the periodontal screening index no periodontitis (39.25 %). Only 7 of the military participants (6.54 %) have pockets equal or more than 5 mm. The majority of the military participants (55.14 %) have a mild form of periodontitis. None of the participants had pockets more than 6 mm. About half of all sextants are clinically healthy (51.24 %).
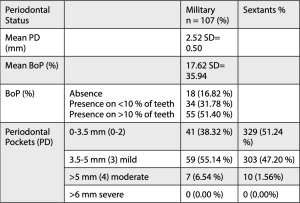
Table 4: Periodontal Status: Mean PD and BoP. Bleeding on Probing and Pocket Depth (PD) after examining of all teeth.
CPI or (Dutch) Periodontal Screening Index: table 6 shows the CPI modified found after examining four sites per tooth in all teeth present in the mouth, except for the wisdom teeth. In the study we found that the first sextant (57), closely followed by the third sextant (56) had the highest prevalence of periodontal pockets. This is in line with the finding in a previous study, were also the first and third sextants hat the highest scores (20).
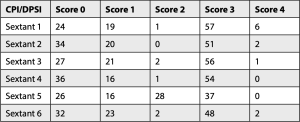
Table 5: Community Periodontal Index (CPI) or Dutch Periodontal Screening Index (DPSI) scores
Prevalence of Periodontal Changes and associated factors of gingivitis and periodontitis Table 6 shows the characteristics of the study population in relation to healthy gum and severity of gingivitis and periodontitis (n=107). A quarter of the participants had healthy gum, and another quarter had gingivitis. Half of the military participants had a kind of periodontitis. About a third of participants smoke. From a total of 14 heavy smokers (>15 cigarettes/day), 1 military (7.14 %) was diagnosed with PSI= 4 or moderate periodontal disease, while 3 military (21.43 %) were diagnosed as healthy or had gingivitis or PSI = 0-2. From 25 smokers (< 14 cigarettes/day) 2 military (8.00 %) hat PSI= 4 and 11 smokers (44 %) had PSI between 0 and 2. Between 43 % and 72 % of the participants brush their teeth twice a day.
We observed that there is minimal difference in smoking habits between participants with healthy gum (DPI= 0-2) and military with periodontitis (3-4), without statistical significance (OD Ratio= 1.05; p= .899).
We didn’t find a statistically significant relation between the severity of gingivitis and periodontitis and the frequency of brushing (OD Ratio= 0.73; p= .438) and the knowledge of interdental brushes (OD Ratio= 0.88; p= .813).
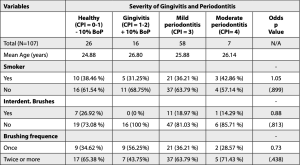
Table 6: Logistic regression analysis shows the association of age, smoking, frequency of cleaning teeth with different periodontal disease severity.
DISCUSSION
Until now, there is no Belgian periodontal health study found in a military population. Rapid Deployment military are mostly young men. The objective of the study was to determine the prevalence, severity and risk factor associated with periodontal disease of young adults, using the new classification of periodontal disease (2). To rule out biases, we use a calibrated automatic third-generation periodontal probe Pa-on to measure the periodontal condition of the probands.
We used the CPI score recommended by the AAP/EFP (2017), allowing future comparability with other studies worldwide. However, the CPI score has some limitations. It is important to differentiate between the objectives of etiological studies and surveys, including the potential bias in population and gender representation.
According to the CPI evaluation, 65 participants (60.75 %) were diagnosed as having “periodontitis”. In terms of initial diagnostics, a strict diagnosis of periodontitis (CPI 3-4) or no periodontitis (0- 2) seems reasonable. In relation to treatment, there is a considerable difference depending on whether one or more sites of a tooth are assigned CPI 3 or 4.
In this study the mean pocket depth, BoP and PI was similar to prevalence surveys in Portugal on 172 civilian participants between 18 and 30 years old and 461 Norwegian participants between 20 and 34 years old, mean PD= 2.52 vs 1.85 mm; mean BoP= 17.62 % vs 18.09 % (8) vs. 31.9 % (12) ; mean PI= 32.37 % vs. 36.99 % (8) vs. 45.2 % (12).
In 1979 Hugoson and Koch reviewed the oral condition in 1000 Swedish individuals, bleeding on probing was found in 35% and 24% of examined sites in the 20- and 30-year-old groups, respectively (16). In our study we found a mean score of bleeding on probing of 17.62 %. This is nearly an improvement of fifty percent. In our study a CPI score of 4 was found in 6.5 % of the participants. This is in line with other prevalence studies in the same age category (9,17). We found no pockets larger than 6 mm in our study. In some studies, we found these pockets in 1.3% of probands (9) and 8.1 % among 35 years-old ́s in Oslo (17). This is a good score because in our study the majority of the soldiers have an elementary education.
In comparison with another recent survey of recruits aged 19.6 years of the Israeli Army. At least one site with PD >5 mm was found in 20.1% of the Israeli recruits (10). In the present study, the corresponding proportion was 6.5 %, indicating a substantially lower prevalence of periodontitis under the Belgian military. With regard to tooth brushing, in the present study most patients have a brushing frequency of twice a day (61.7 %), higher than that found in a Portuguese study (52.6 %) (7), but lower than another Portuguese study (77.8 %) (8), Japan (94.8 %) (11), Norway (71.9 %) (12) and a Portuguese military study (65.6 %) (19).We didn’t find a statistically significant relation between the severity of gingivitis and periodontitis and the frequency of brushing, the knowledge of interdental brushes and smoking. Future research would be advisable to study the impact of periodontal health promotion on military dentists and accredited civilian dentists to the army (14).
There are several shortcomings in this study to compare prevalence between military and civilian studies. Young active combat personnel in Belgium consist mainly of men and according to the STANAG agreements witch Belgium apply are these soldiers obliged to undergo an annual dental check-up, so that theoretically their oral condition should be better than an average population. We didn ́t consider systemic diseases and education level, because only 2 probands had a systemic disease and only 10 % had a higher educational level.

Using the Pa-on Probe in the Belgian Military Hospital (Source: Tom Verhofstadt)
Conclusion
Periodontal disease data from several countries collected by using CPI, is stored in the WHO Global Oral Health Data Bank for the ages 15-19 years, 35-45 years and up to 45 years. Unfortunately, less periodontal information is available for young adults between 19 and 35 years old. The plausible reason for this lack of information comes from the fact that the results from early studies suggested little or no periodontal destruction before the age of 30 years exist.
Our survey revealed that young military adolescents have no optimal oral hygiene habits and negligence of interdental hygiene. This, in turn, means that efforts to promote dental mindedness should be reiterated in the present and future young adolescent population. Survey results and accurate health statistics serve as base findings for the military agreements to make choices how to improve the military agreements and treatment of the participants. The CPI is essential for initial periodontal examination. If signs of pathological changes (CPI 4) in the periodontium are established, detailed findings are essential for further diagnostics. This study shows that risk factors such as smoking and dental hygiene play not a significant role in the periodontal condition up to 35 years. Despite the elementary education of the probands, the data are in line with data from an average population from other studies. It is important to provide information and instructions about dental hygiene and periodontal diseases to soldiers, even if the majority do not yet show any forms of destruction at this young age.
Conflict of Interests: The author declares that there is no conflict of interests regarding the publication of this paper.
Acknowledgements: The expert advice of military dentist Matthias Neukermans and military dental assistant Jean-Michel Hanquin are gratefully acknowledged.
Dr. med. dent. Tom Verhofstadt, OF3, Belgian Army.He obtained his master ́s degree in dentistry at the Catholic University of Leuven in Belgium and the title of Doctor at the University des Saarlandes in Germany. He has been serving in the Belgian Reserve since 1991. He is a member of the Belgian Army DVI team. Since 1999 he has owned a Dental clinic in Kevelaer (Germany) and performs Orthodontic treatments at a Dental clinic in Kortenberg (Belgium).
ABSTRACT
Background: Information on periodontal disease and its predictors in military personnel is limited. The community periodontal index (CPI) is an element of the initial dental examination. The CPI provides information on the periodontal situation and provides a first estimate of the periodontal treatment required.
Patients and Methods: One hundred and seven military participants between 19 and 35 years of age were involved in a cross-sectional observational study. The study was conducted between June 1, 2023 and December 15, 2023 at the Beauvechain military airbase, Belgium. Participants were analyzed of their periodontal condition during the annual dental check-up according STANAG 2466 to make military personnel dentally fit. Before the periodontal examination, a panoramic x-ray was taken and participants filled in a self-administered questionnaire that included several epidemiological variables such as age, educational level, smoking status, oral hygiene habits like toothbrush frequency and usage of dental floss/interdental brushes.
One examiner evaluated the periodontal status of the participants by calculating the community periodontal index (CPI) with an electronic 3rd generation periodontal probe Pa-on (Orangedental, Germany). The Odds ratio was used for statistical analysis at 5 % level of significance.
Results: The mean age of the study participants was 25.98. The averages probing depth, plaque index and bleeding on probing were 2.52 mm, 32.37 % and 17.62 %, respectively. 38.32 % of the subjects had no pathological pockets and 16.82 % showed no bleeding on probing. 55.14 % of the subjects had mild periodontitis. 53.27 % of the subjects had gingival recessions. 51.24 % of the sextants are between CPI 0 and 2. CPI 3 was calculated on 47.20 % and CPI 4 was calculated on 1.56 % of the sextants. We found that the first sextant, closely followed by the third sextant had the highest prevalence with periodontal pockets.
No correlation was found between CPI and oral habit as frequency of brushing and smoking in the age group from 19 to 35 years old. Conclusion: Our study showed that young Belgian military adolescents don’t have optimal oral hygiene habits and negligence of interdental hygiene. This, in turn, means that efforts to promote dental mindedness should be reiterated in the present and future young adolescent population. Study results and accurate health statistics serve as base findings for the military agreements to make choices how to improve the military agreements.The study shows that risk factors such as smoking, and hygiene habits don’t play a significant role for the periodontal condition up to 35 years. Despite the elementary education of the participants, the data are in line with data from an average population from other prevalence studies. It is therefore important to provide more information and instructions about dental hygiene and periodontal diseases to military personnel, even if they show any minor forms of destruction at this young age.
Dr Tom Verhofstadt, OF3
Belgian Reserve Army
Email: [email protected]
Date: 09/18/2024
Source: European Military Medical Services 2024











