
Article: R.M. HAGEN, H. FRICKMANN (GERMANY)
Outbreak Investigation and In-Theatre Diagnostics Using Real-Time PCR
In small, front-line (role 2) MTFs, the only diagnostic techniques usually available with which suspected outbreaks of infection can be investigated are malaria microscopy and rapid immunochromatographic tests. This means that the diagnostic range is very narrow while, at the same time, the results produced by rapid tests may be of little value in view of the limited sensitivity and specificity of these methods. The use of culture-based infection diagnostic techniques is only possible where the full infrastructure of a microbiological field laboratory is at hand; such laboratories are not widely present and are generally only provided in role 3 facilities. In circumstances in which reaction time can represent a crucial factor, the fact that medical facilities cannot always be transported by air becomes a problem. The management of time-related factors is a particular challenge in relation to the diagnosis of the outbreaks of infections. This challenge can be overcome using recently developed molecular techniques, specifically real-time polymerase chain reaction (PCR), which has already been successfully used by the German Armed Forces to investigate epidemics and to monitor personnel in tropical theatres of operation.
Introduction
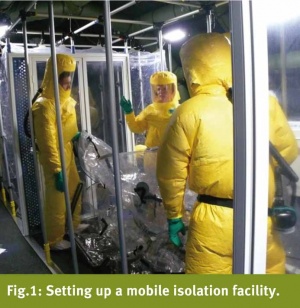
Today's Bundeswehr (German Armed Forces), as a modern combat force, is involved in a wide range of missions in subtropical and tropical regions, such as the current EUTM Mali, the EU NAVFOR Operation Atalanta off the coast of Somalia, UNIFIL Lebanon and the ISAF Afghanistan. These missions represent major challenges for the Bundeswehr medical services with regard to the handling and management of the infectious diseases that can be encountered in these regions. Endemic to West African countries such as Mali are, for example, the pathogens responsible for viral haemorrhagic fever (VHF), the Old World arenavirus that causes Lassa fever and the Ebola virus, a member of the family Filoviridae [1, 2]. A focus of particular concern at the present time is the currently largest global outbreak of EVD (Ebola virus disease) in Guinea, Liberia and Sierra Leone. As neither vaccines nor anti-infective agents are yet available, the only therapeutic measures that can be taken are the rapid identification of the pathogen in cases of suspected infection and the isolation of affected patients (barrier nursing) (Fig. 1).
But even respiratory infections and 'banal diarrhoea', the spread of which are facilitated by living in confined and often multinational base camps in extreme climatic conditions, can very quickly undermine the operational capacity of a combat unit. In the case of relatively small contingents consisting of about 100 personnel, the temporary diarrhoea-related incapacity of some 10 - 20 members of the unit per week – as was the case at the commencement of the EUTM Mali mission – significantly reduces its fighting strength. However, the high risk of the development of bacterially-induced diarrhoea, an ailment characteristic of deployment in tropical regions, was taken into account and a calculated empiric antibiotic approach was taken that successfully reduced the duration of the diarrhoea-related disorders. But as bacterial resistance is on the rise in West Africa [3], there is also the possibility that such calculated therapeutic strategies could fail so that the additional use of diagnostic techniques would seem highly advisable.
In the following, we consider the actual case of diarrhoea surveillance in the Koulikoro field camp, EUTM Mali, and a fictive example of analysis of an outbreak of VHF in order to demonstrate how PCR-based diagnostic techniques can be employed under the conditions of field deployment.
The problems associated with use of standard microbiological techniques in tropical theatres
For the rapid and patient-dependent evaluation of tropical medicine-relevant infections and symptoms, such as fever and diarrhoea, under the conditions obtaining in the field and theatres of operations, careful preparation and the maintenance of proficiency among laboratory personnel are essential; without this, it will not be possible to identify the rarer pathogens, such as the various Plasmodium species, amoebas, tropical viruses and others. In addition, there is no way of ensuring that techniques for diagnosing infections, including biochemical culture methods of identifying bacteria up to and including those in risk group 2, can be made available everywhere because of the logistical problems involved. It is clear that the employment of culture techniques in facilities under canvas is not possible in view of current health protection and biological safety requirements. At the same time, the use of container-based laboratory facilities is often impossible for tactical reasons, such as the need for troops and medical facilities to be rapidly deployable by air, or because of the nature of the terrain in the theatre.
Even in situations in which the infrastructure for standard microbiological culture techniques is available, as is the case in Prizren (KFOR Kosovo) and Mazar-e Sharif (ISAF Afghanistan), it takes several days before results are available. In the case of the outbreak of an infection, however, rapid identification of the causal pathogen on the same day is desirable in index cases if secondary cases of infection are to be prevented. Where it is suspected that a disorder is attributable to infection with a potentially dangerous pathogen that is classified in risk group 3 or 4, it is usually the case that samples need to be sent to a suitable reference laboratory in the homeland, a necessarily time-consuming procedure. Host nation support can rarely be relied upon and there are seldom local laboratory facilities that can supply reliable results that comply with the usual NATO microbiological standards. Many local laboratories, such as those in Mali or Afghanistan, are generally unable to employ standards for quality assurance that are equivalent to the German 'Quality standard for microbiological-infectiological diagnostics (MiQ)' or the 'Guidelines of the German Medical Council for quality assurance of medical laboratory techniques (RiliBÄK)'.
The value of direct detection methods that can be used in field clinico-chemical laboratories, such as light microscopy and rapid immunochromatographic tests, is seriously limited with regard to sensitivity, validity and spectrum [4]. Only in the case of the identification of malaria, the most important tropical medicine-related differential diagnosis, is light microscopy (perhaps supplemented by a rapid immunochromatographic test) still seen as the diagnostic gold standard [5]. In view of the fact that increasing numbers of laboratory assistants have insufficient experience of malaria microscopy, it would also be desirable to see a changeover in the medium term to the use of robust RiliBÄK and MiQ-conform real-time PCR systems even in the field of malaria diagnosis [6].
New approaches using molecular techniques

While the methods of molecular diagnostics are already being widely used in civilian and military medical facilities in Germany and are regulated by binding quality standards such as RiliBÄK and MiQ, the use of nucleic acid amplification techniques (NAT) and specifically real-time polymerase chain reaction (PCR) has yet to be generally established in field scenarios. One of the main reasons for this is the as yet insufficient standardisation and thus the availability of many differently operated equipment platforms, meaning that diagnostic assistants need to be separately instructed in the use of each device. In field laboratories, PCR is currently being used only in the form of a standardised rapid test system (GenXpert, Cepheid, Sunnyvale, CA, USA) for the identification of MRSA (methicillin-resistant Staphylococcus aureus) and Mycobacterium tuberculosis (the TB pathogen) (Fig. 2), while more complex cases require the dispatch of the necessary device and the specially trained personnel as a RDOIT, or rapid deployable outbreak investigation team.
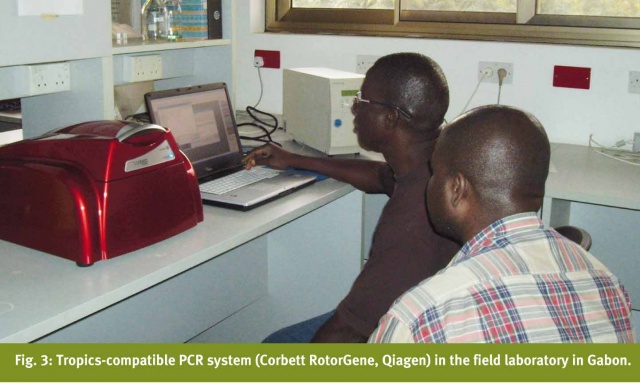
However, when a certain minimum level of technical resources is available (Fig. 3), real-time PCR can be used in its multiplex variant to amplify specific regions of the DNA of a range of pathogens and to identify these during the same test run. The 'multiplex' concept not only slashes costs per result to just a few euros but also means that work input is reduced, thus ensuring that results can be obtained within a reasonable time. As there is no need for culture incubation, a reliable result can be obtained using inactivated sample material (assuming that pathogen density is adequate) within just 2 - 3 hours.
Since the establishment of the Department of Tropical Medicine at the Bernhard Nocht Institute of Tropical Medicine of Hamburg Bundeswehr Hospital, various diagnostic PCR assays have been used in combination with a robust PCR platform and their viability for employment in tropical environments has been evaluated. Of particular interest were PCR systems that could be used to identify the cause of diarrhoea-related symptoms in personnel serving in tropical theatres. For use in this indication, multiplex PCR protocols have been developed for the identification of invasive bacterial pathogens (Salmonella spp., Shigella spp./enteroinvasive Escherichia coli (EIEC), Campylobacter jejuni and Yersinia spp.), intestinal protozoa (Entamoeba histolytica, Giardia duodenalis, Cryptosporidium spp., Cyclospora cayetanensis), intestinal nematodes (Ascaris lumbricoides, Ancylostoma spp., Necator americanus and Strongyloides stercoralis), trematodes (Schistosoma haematobium, S. mansoni and S. intercalatum) and for commercial PCR systems for the detection of enteropathogenic E. coli (EPEC), enterotoxic E. coli (ETEC), enteroaggregative E. coli (EAEC), enteroinvasive E. coli (EIEC)/Shigella spp. and enterohaemorrhagic E. coli (EHEC)) together with viral diarrhoea-related pathogens (norovirus, astrovirus, rotavirus and adenovirus). In addition, there are in-house pan-eubacterial and pan-fungal PCR systems with downstream sequencing that can be used to identify bacterial pathogens and pathogenic fungi in primarily sterile sample material. Special PCR systems for the detection of e.g. viral haemorrhagic fever viruses (Ebola, Marburg, Lassa, CCHF etc.) are used in cooperation with the civilian Bernhard Nocht Institute, the German National Reference Centre for Tropical Medicine and the WHO Collaborative Laboratory; and these are discussed in more detail in the following.
The above-specified PCR systems have been evaluated in several infection-epidemiological studies in tropical environments [7-13]. The main cooperation partners for evaluation testing in the tropics were the Kumasi Centre for Collaborative Research (KCCR) in Kumasi, Ghana, with which the Bernhard Nocht Institute collaborates and the Department of Microbiology and Parasitology of the University of Antananarivo, Madagascar (Fig. 4). During previous study visits to the tropical cooperation centres, valuable experience was obtained with the transport of the technical apparatus and the reagents, especially with regard to the maintenance of an uninterrupted cold chain. The operation of the PCR system under local, technical and climatic conditions proved to be problem-free and reliable. In contrast with many previously frustrating attempts to obtain utilisable microbiological results in difficult tropical conditions, PCR turned out to supply in this context valuable new infection-epidemiological data from tropical Africa.

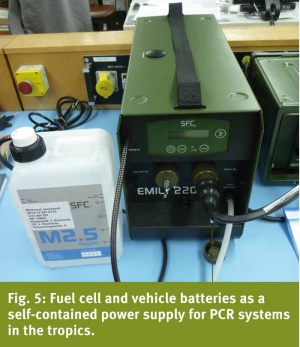
As the power supply in the corresponding regions is unreliable, an autonomous power system has been developed based on two truck batteries and a methanol-powered fuel cell (Fig. 5).
Initial use of real-time PCR in a subtropical theatre – ISAF Afghanistan
The real-time PCR platform developed by the tropical medicine laboratory team was first used in the context of the A/H1N1 ('swine flu') pandemic in April 2009 in the Mazar-e Sharif ISAF field hospital in Afghanistan. With the collaboration of the Dept. of Virology of the Bernhard Nocht Institute and within just a few days, a new PCR assay was made available through an expert network that was suitable for the device used by us. This made it possible to identify a new variant of the pathogen. On the instructions of the field commander, the mobile PCR facility was transferred to the theatre to ensure that even before the first cases occurred, the operational unit in Afghanistan had a reliable instrument at hand to detect and prevent any spread of this new influenza variant [14].
Diarrhoea surveillance in Camp Koulikoro, EUTM Mali
Respiratory tract infections, fever of unknown origin and diarrhoea (sometimes caused by contact with contaminated food and drinking water) are the most frequently encountered medical problems among military contingents serving in tropical theatres. In this context, less common pathogens (such as protozoa) may also be the cause. Amoeba infections can even develop into an acute life-threatening disorder (amoebic dysentery) while amoebic liver abscesses can be a late consequence of the infection. In tropical theatres of operations, the availability of a rapid, highly sensitive and specific diagnostic tool to identify infectious pathogens is of particular benefit as this means targeted therapeutic measures can be initiated in good time in order to effectively counteract the risk of an outbreak.
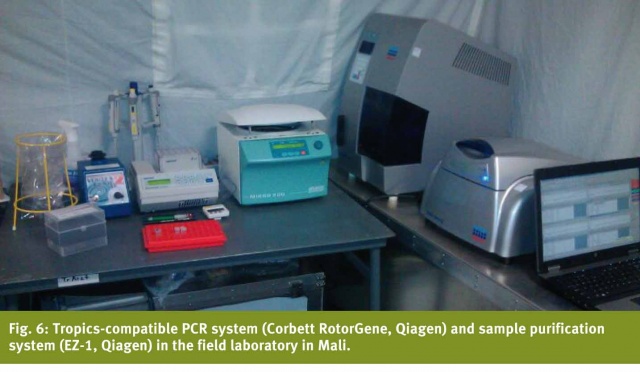
In view of the above-mentioned frequency of cases of diarrhoea among members of the German contingent of EUTM Mali at Camp Koulikoro, particularly in the early stages of the mission, the chief hygienist in the field requested the Dept. of Tropical Medicine to conduct an on-site surveillance in the autumn of 2013. Between December 2013 and April 2014, a mobile molecular diagnostic platform (Fig. 6) together with a trained medical assistant was deployed to Camp Koulikoro in order to conduct an on-site analysis of faeces samples for the presence of invasive bacterial pathogens (Salmonella spp., Shigella spp./EIEC, C. jejuni and Yersinia spp.), intestinal protozoa (E. histolytica, G. duodenalis, Cryptosporidium spp., and C. cayetanensis) and enteropathogenic E. coli (EPEC, ETEC, EAEC, EIEC/Shigella spp. and EHEC). It was established that the predominant causative agent of the diarrhoea symptoms was enteropathogenic E. coli [15]. However, as there was a significant fall in the incidence of diarrhoea and the risk of an outbreak had thus receded in the stated period, the PCR system was returned to the homeland. If necessary, sample material can still be transported from Mali to Germany in order to provide for continued monitoring of the situation. The problem of the development of resistance is also an aspect that will be assessed.
Case study: molecular VHF diagnostics in the field
One of the aims of the StratAirMedEvac concept of the Bundeswehr is to transport severely ill patients by air as quickly as possible (ideally within 48 hours) from the theatre of operations to the homeland. However, IATA (International Air Transport Association) regulations limit the use of aircraft to transport patients with suspected viral haemorrhagic fever. Wotj the critically ill patient, the 'scoop and run' approach needs to be replaced by a 'stay and play' strategy – in effect, the medical care of patients with VHF needs tobe provided under barrier nursing conditions in the medical facility. As front line medical facilities are not designed to provide longer term care under barrier nursing conditions, the material and human resources available on site will very soon reach the limits of their capacity.
In addition to being able to reliably diagnose malaria, it would also be of advantage to be capable of rapidly identifying pathogens in carefully inactivated patient samples in order to confirm or exclude the presence of VHF at the earliest opportunity. It would then be possible to decide whether isolation of the patient under barrier nursing conditions is really necessary. For this eventuality, the civilian Bernhard Nocht Institute as the German national reference centre for tropical diseases has several PCR panels that are based on accredited diagnostic procedures. When the first index or suspected case arrives at a medical facility, the objective is to quickly transport the inactivated sample to the WHO reference laboratory at the institute. In situations in which distance is a factor (e.g. if there is continuation of an outbreak), the diagnostic panels can also be transferred by the Dept. of Tropical Medicine to the field laboratory. The phased use of three panels should make it possible to complete the most important differential diagnostic procedures within 6 - 8 hours.
The first panel covers the VHF viruses that represent the highest risk because they are primarily transmitted by the aerogenic route between individuals. These include the Filoviruses [16, 17], the Lassavirus and the Crimean-Congo haemorrhagic fever virus [18]. The second panel covers VHF viruses that are not primarily aerogenically transmitted, including yellow fever virus (FTD Tropical Fever Africa Kit, Fast-track Diagnostics, Luxembourg), Rift Valley fever virus [19] and dengue fever virus (FTD Tropical Fever Africa Kit, Fast-track Diagnostics). The third panel is for non-viral pathogens that are important for differential diagnosis, such as the malaria pathogen Plasmodium spp. (FTD Tropical Fever Core Kit, Fast-track Diagnostics), meningitis and sepsis pathogens, such as Neisseria meningitides (FTD Bacterial Meningitis Kit, Fast-track Diagnostics) and Leptospira spp. (FTD Tropical Fever Core Kit, Fast-track Diagnostics). To avoid the risks associated with the analysis of a larger sample drop or smear of the potentially infectious blood of the suspected case of VHF infection, malaria diagnosis can also be performed using the PCR platform.
Discussion and outlook
With the development and testing of state-of-the-art multiplex/real-time PCR techniques for the detection of tropical pathogens (including enteropathogenic parasites, bacteria and viruses) that can be employed with mobile field and tropics-compatible device platforms, tropical medicine now has a powerful diagnostic tool that can be used for the investigation of infectious tropical diseases in the field. As has been successfully demonstrated in Koulikoro (EUTM Mali), it is possible to use this for comprehensive diagnosis of the causes of diarrhoea without the need for the time-consuming preparation of cultures (e.g. as in this case, in a rescue centre as part of the investigation of an outbreak). However, it is essential that appropriately trained personnel are available, and this is currently the main problem that is preventing more extensive implementation.
The inclusion and continuing use of PCR techniques in the range of diagnostic services provided by field laboratories, particularly at role 2 facilities, should be discussed at the NATO level. When it comes to multinational missions, the challenge will be to identify a device platform that is acceptable for all involved nations so that they can appropriately train their personnel. Standardisation of the techniques employed is essential if reciprocal operation of these devices by the various qualified personnel is to be possible. Without such standardisation, use of a complex technical procedure of this kind will be restricted to individual nations or specialised task force units and it will not become widely disseminated. The ease of use by field personnel and the avoidance of contamination under field conditions are important criteria when it comes to selecting the most appropriate technical solution.
However, it still remains to be seen whether 'closed' and commercially available systems can provide an adequate response to the problems posed by specific aspects of tropical medicine. It is doubtful that profit-orientated businesses operating on the free market will have the necessary incentive to make rare tropical diseases the focus of their R&D activities. The systems currently available cover only a very limited range. One option that could provide the necessary solution over the long term is NGS (next generation sequencing – also known as 'ultra deep' sequencing) that makes it possible to directly identify pathogens in a biological sample [20]. A definitive suspected diagnosis is not necessary if it is to be used and it can theoretically detect previously unidentified pathogens – in future, it will also be possible to employ it with the aid of bench top devices that are no larger than a laser printer [21]. Its value for diagnostic purposes has not yet been fully assessed, particularly in tropical environments, while it is currently plagued by IT-related problems with the database-supported evaluation of sequences [22]. But it will be worthwhile keeping an eye on the development of this technology. In the near future, it will in any case be necessary for the military medical services themselves to undertake their own development and evaluation work in order to provide solutions appropriately tailored to conditions in the field.
The development of innovations in the sector of molecular infection diagnostics thus continues to represent an important challenge for the medical services. It is particularly difficult to provide services based on the standard microbiological protocols during missions in tropical regions that require rapid mobility and deployment so that the development of flexible adaptations that provide new technological solutions has become imperative.
Conflict of interest
The authors declare that there is no conflict of interest in terms of the guidelines of the International Committee of Medical Journal Editors. N
Authors
Lt Col PD Dr med. Ralf Matthias Hagen
Dept. of Tropical Medicine of the Bernhard Nocht Institute
Medical formation and degrees
1994 Medical studies and degree as medical doctor (University of Ulm/GE and Lyon/F), Thesis at the Medical Faculty / University of Ulm
Postgraduate formation
1994 –1996 Internship in internal medicine (German Armed Forces Hospital Ulm);
1996 – 1998 Internship in general medicine (Munich); 1998 – 2003 Internship in clinical microbiology (Medical departments of the Universities of Munich, TUM and LMU);
2001 Diploma of Tropical Medicine & Parasitology (Bernhard Nocht Institute for Tropical Medicine); 2004 Consultant for Clinical Microbiology, Virology and Infectious Disease Epidemiology; 2008 Consultant for Infectious Diseases; Since 1998 Research fellow in the fields of: Clinical Microbiology, Medical B Defence, Tropical Medicine, Infectious disease Epidemiology; 2013 Habilitation at the Medical Faculty / University of Hamburg;
Actual position: Head of laboratory department Department of Tropical Medicine at the BNITM Hamburg
Address for the authors:
Hamburg Bundeswehr Hospital
Bernhard-Nocht Strasse 74, 20359 Hamburg, Germany
Tel.: 0049-40-6947-28740, Fax: 0049-40-6947-28709, E-mail: [email protected]
First and corresponding author
CO-AUTHOR
Dr Hagen Frickmann, Major MC, MD
Department of Tropical Medicine, Bundeswehr Hospital
Hamburg, Germany
2007 – 2008 Bundeswehr Institute of Microbiology, Munich, Germany;
2008 – 2010 Institute for Microbiology, Virology and Hygiene, University Hospital of Rostock, Germany;
2010 – 2011 Department of Internal Medicine, Bundeswehr Hospital of Hamburg, Germany; from 2011 Department of Tropical Medicine, Bundeswehr Hospital of Hamburg, Germany; Deployment: Microbiological Laboratory, Field Hospital of Camp Marmal, Mazar-e-Sharif, Afghanistan, October – December 2012
Date: 08/01/2014
Source: MCIF 3/14











