

Article: C. v. SEE, C. KÜHLHORN, F. HELLWIG, N.-C. GELLRICH (GERMANY)
Preparation for Active Deployment and Combat Readiness from the Perspective of Dental Medicine
A critical review: As part of their preparation for active deployment, personnel of the armed forces are required to undergo a medical examination that is appropriate to the proposed theatre of operations. This generally includes a thorough dental examination. In addition to assessing specific absolute criteria, the examining dentists also determine whether problems are likely to occur that could impair the subjects’ level of dental fitness. The objective is to assess both the combat readiness of personnel and their suitability for transport by air. These specific military requirements are reviewed in this article on the basis of selected case reports.
Military dental examinations focus on the current general dental status of the patients and the possible future complications they may experience (dental fitness classes I-III). As a rule, it is advisable to conduct a detailed dental examination of personnel prior to any form of active deployment. The objective is to ensure that the dental health status of personnel is such that they will not require any dental treatment while in the theatre of operations. This means that, unlike the civilian sector where facilities for dental treatment are always directly available to a patient, the prospective element plays a far more important role in military medical dentistry. Also to be taken into account are combat-specific aspects, such as the increased risk of bruxism, immunodeficiency as a result of exposure to psychological stress and the rapid changes in pressure that occur during flight and diving. There are changes to ambient pressure during sea diving, flying or presence at higher elevations. Among other things, this can lead to various pathophysiological alterations and pressure-related sensations of pain in the teeth (barodontalgia).
There is also the generalised risk of barotrauma as a result of changes to ambient pressure. The pressure changes that occur while flying and diving can differ considerably. For example, the pressure changes experienced by flight personnel on a commercial airliner are minor although their duration of exposure to these changes is relatively long. This is not the case for military personnel and aerobatics pilots ‒ in contrast with commercial air transport, very rapid changes in pressure occur while the personnel are also exposed to powerful acceleration forces.
Because of the higher density of the surrounding water, divers can be subjected to extreme ambient pressures, but the duration of exposure tends to be shorter than that of flight personnel. An additional complication is the fact that the gases required for breathing by divers vary considerably depending on depth and diving technique used so that, in addition to the changes of ambient pressure, divers may also be exposed to various physiological effects on their metabolism. Barodontalgia has been reported in pilots at heights of 600 - 1500 m and in divers at depths of 10 - 25 m1.
At present, the system of classification of barodontalgia proposed by Ferjentsik is generally employed, based on an assessment of causes and clinical symptoms2 (Table 1).
| Classification | Cause | Symptoms |
|---|---|---|
| Class I | Irreversible pulpitis | Sharp pain on exposure to increased pressure |
| Class II | Reversible pulpitis | Dull pain on exposure to increased pressure |
| Class III | Pulp necrosis | Dull pain on exposure to decreased pressure |
| Class IV | Periapical pathosis | Persistent severe pain on exposure to decreased and/or increased pressure |
Table 1: Classification of barodontalgia by clinical symptom
Barodontalgia is essentially a pressure-induced condition that can occur in the presence of both underpressure and overpressure. The physical effects are governed by Boyle's law, which states that at a constant temperature the volume of a fixed mass of an ideal gas is inversely proportional to the pressure of that gas. This means that as ambient pressure increases, the volume of a confined gas decreases while, vice versa, its volume increases as ambient pressure decreases. Although the aetiology of barodontalgia is not yet fully understood, it has been established that toothache experienced during ascent by pilots and divers can indicate the presence of a disorder of the vital pulp tissue (pulpitis). Similar pain experienced during descent can be a sign of pulp necrosis or facial barotrauma1. The latter may be experienced as diffuse pain or as local, stabbing pain.
The related pressure differences can occur in the human body when a gas-filled cavity cannot communicate with the exterior so that pressure cannot be equalised. In clinical terms, the resultant difference in the pressure in the gas-filled cavity and that of the external environment can result in the development of pain, oedema, or vascular gas embolism3. The corresponding symptoms commonly occur in the lungs, the middle ear or the maxillary sinus (barosinusitis)4; 5. Frequently, barosinusitis develops in the presence of acute or chronic maxillary sinusitis. When there is a change to ambient pressure, the pressure in the maxillary sinus rises or falls as appropriate as there is no possibility of pressure compensation. The resultant difference in pressure can cause headache, a sensation of numbness or toothache in the maxillary lateral incisors. A further problem for clinical diagnosis is that it is difficult to differentiate between barosinusitis and barodontalgia on the basis of pain in the maxillary region alone6; 7.
In addition, studies conducted in military pilots have shown that there is an increased incidence of bruxism during flight in these personnel. It is also difficult to differentiate between maxillary pain and toothache caused by this effect and that attributable to barodontalgia.
Similar effects have been observed in divers. In order to facilitate pressure equalisation, divers carry out chewing movements with their mouth while they also need to ensure that there is a permanent pneumatically effective seal between mouth and mouthpiece. These movements are frequently associated with stress on the masticatory muscles and maxillary pain.
In general, barodontalgia is defined as pain that occurs in the region of the teeth in the presence of pressure changes8. The phenomenon was first observed in air crews during World War II and was originally known as 'aerodontalgia'. The effect was also subsequently reported in divers. The incidence of this type of pain is generally quoted as 0.26 - 2.8% in all flight personnel and divers exposed to such pressure changes6; 9; 10. There is no statistically detectable difference between divers and flight personnel in terms of incidence: similarly, there is no statistically detectable difference between professional and hobby divers with regard to incidence. However, it can also be assumed that the actual incidence of barodontalgia among military personnel is significantly greater. Divers and pilots may avoid reporting such effects to their medical officers as they fear this could lead to their disqualification from their profession, with the associated negative consequences for their careers.
In view of the fact that the aetiology of barodontalgia is still unclear, current recommendations for the dental care of air crews and diving personnel tend to be based on the available statistical evidence11. Another complicating factor is that barodontalgia can occur irrespective of the type of pressure change during both increases (descent) and falls (ascent) in pressure and may even persist after pressure equalisation12. There is considerable debate at present as to whether (co-) factors might also play a role; such potential co-factors include dentogenic infections, sinusitis, differences in the expansion behaviour of dental enamel and pulp, and the displacement of fluids within the dentinal tubules13; 14; 7.
In animal experiments, Carlsson et al. were able to demonstrate that fluid moved from the dentine to the pulp chamber following appropriate preparation of the enamel under hyperbaric conditions13. According to as yet unpublished findings of the same authors, irreversible morphological changes in human teeth can occur at the pulp/dentine barrier that do not occur if the enamel is intact. It is postulated that these changes may be a causative factor for pain. Brannstrom et al.15 have subjected barodontally damaged teeth to clinical evaluation and their results support this hypothesis. Retrospective studies have also shown that most patients with clinically manifest barodontalgia had carious lesions or defective restorations extending into the dentine16. The clinical implication of this is that patients who have carious lesions or have undergone dental treatment that involves the exposure of dentine (for example, during preparation for the provision of prosthetics) should avoid diving or flying until definitive treatment has been provided.
In the literature, pulpitis with periapical inflammation or a status post dental restoration are reported to be the most common causes of barodontalgia. Although the pathophysiology associated with the pain sensations has yet to be fully explained, it can be assumed that the clinical symptoms are the result of impaired microcirculation in the dental pulp.
In addition to cases of toothache, incidents in which changes in ambient pressure have resulted in fractures to teeth and dental restorations in pilots and divers have been reported17. To date, this effect has only been observed in association with the use of non-adhesive restoration material and the cause was for some considerable time postulated to be the prolonged trapping of gas between the filling and the tooth. However, more detailed analysis showed that there was secondary caries beneath the fractured fillings in such cases. It is thus now believed that the movement of fluids from carious dentine is the cause of pulpitis17.
Our investigations have shown that restoration with an adhesive preparation using an acid etching technique and plastic filling material result in the creation of a seal that remains intact on exposure to pressure of at least 5.0 bar. It is therfore advisable to use an adhesive rather than non-adhesive approach for the conservative restoration of teeth in persons who are likely to be subjected to variations in ambient pressure.
In addition to the differing expansion/compression properties of teeth and dental materials on exposure to pressure, the inclusion of gas-filled cavities in restoration materials also plays a significant role, specifically in connection with prosthetic replacements18. Musajo et al. were able to demonstrate that the stability of dental restorations was significantly reduced following diving activities in comparison with a control group19. This effect is particularly marked when zinc phosphate or glass ionomer cements are used as fixatives and it is believed that this is due to the fact that air bubbles are trapped in the cement that create micro cracks on exposure to pressure changes. To ensure stability of restorations, these should thus be anchored with adhesive materials rather than simply fixed with retentive cements.
Direct/indirect pulp capping is currently not recommended in patients who are likely to be exposed to pressure changes. It is postulated that variations in pressure can adversely affect the regeneration of pulp tissue. In order to avoid possible complications in advance, endodontic treatment or extraction should therefore be undertaken in cases in which direct pulp capping would otherwise be indicated.
In the case of dental implants, however, no problems have been reported to date in connection with exposure to changes in pressure. No clinically relevant mechanical deformation of the implants or of their superstructures is likely to occur. In addition, our own investigations have also shown that pressure variations do not lead to significant mechanical malformation of the mandible. It can thus be concluded that there is little risk of the loosening of the connection between implant superstructures and abutment teeth.
Case 1
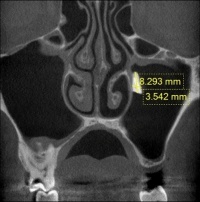 Fig. 2: Radiology image showing the extent of the root fragment in the maxillary sinus
Fig. 2: Radiology image showing the extent of the root fragment in the maxillary sinus
A 25-year-old serviceman reported to his dental officer for assessment of his suitability for deployment in a tropical theatre of operations. The patient reported that he suffered from chronic left maxillary sinusitis. The first molar in the upper left quadrant was missing. This had been extracted at least 4 years previously following the failure of attempts to preserve it using endodontic therapy. Under radiological examination, the presence of a foreign body was detected in the left maxillary sinus. On the basis of the results of 3D imaging following conservative therapy of the maxillary sinusitis, root retention following tooth extraction was postulated with no evidence of an air-fluid level (Fig. 2). The patient was strongly recommended to have the residual root removed prior to deployment abroad. The residual root was removed under local anaesthesia by means of the creation of a lateral access. Following paramarginal incision in the region of the crista zygomaticoalveolaris and subperiostal preparation, a bone flap was removed (Fig. 3). Once the residual root
 Fig. 3: Clinical situation following removal of a maxillary bone flap
Fig. 3: Clinical situation following removal of a maxillary bone flap
was revealed, it could be detached from the exposed Schneiderian membrane and was extracted (Fig. 4). The bone flap was then replaced and fixed using sutures, and the wound was also sutured. There were no complications following surgery. The earliest possible date for deployment of the patient was set at 21 days post surgery, assuming there was optimal progress of the healing process.
Case 2
During assessment of his suitability for deployment in a tropical theatre of operations, a 22-year-old serviceman was found to have supernumerary maxillary teeth (15, 25). These had not beem detected during the clinical examination. However, apparent in 3D digital volume
 Fig. 4: Intraoperative situation on extraction of the root fragment after careful detachment from the Schneiderian membrane
Fig. 4: Intraoperative situation on extraction of the root fragment after careful detachment from the Schneiderian membrane
tomography, was an almost horizontal disposition of the teeth in the close vicinity of the maxillary sinus (Fig. 5). After being informed about and advised on the condition, the patient decided to have the teeth removed prior to deployment. A bone flap was removed following marginal incision from the palatal side, the tooth buds were exposed, bisected in order to avoid damage to the trifurcation of the first molars and then extracted (Fig. 6). There was no oro-antral communication in either case. To provide for optimal healing, the bone flap was replaced and stabilised by means of osteosynthesis (Fig. 7). An intraoral dressing plate was applied for 1 week after surgery. Sutures were removed after 14 days. There were no complications during the postoperative healing process and the results of vitality testing of the first molars continued to be positive.
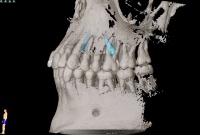 Fig. 5: 3D image of the displaced supernumerary maxillary teet
Case 3
Fig. 5: 3D image of the displaced supernumerary maxillary teet
Case 3
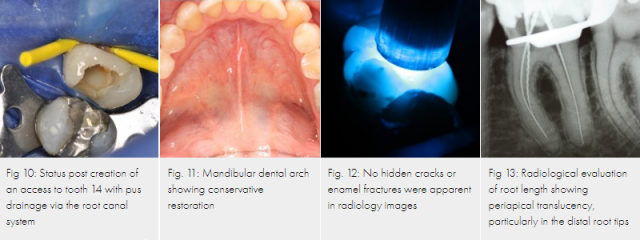
A 32-year-old serviceman presented with severely throbbing pain in the right maxillary region following air transport in a C-160 (Transall) aircraft. On clinical examination, a marked palatal swelling was observed that did not extend beyond the midline (Fig. 8). The result of a vitality test of tooth 14 was negative and the tooth was very tap-sensitive. An area of radiolucency was observed in the periapical region of tooth 14: it was decided to create an access (Fig. 9). Following appropriate preparation of the root canals, the palatal abscess was drained via the root canal system (Fig. 10). After daily lavage and drainage through the root canal system, there was complete remission of the abscess. After insertion of a temporary treatment filling for 4 weeks, a permanent root filling was provided.
 Fig. 6: In order to remove supernumerary tooth 15 from the trifurcation of the first molar after creation of the bone flap, it was bisected and then extracted
Fig. 6: In order to remove supernumerary tooth 15 from the trifurcation of the first molar after creation of the bone flap, it was bisected and then extracted
Case 4
A 26-year-old male patient presented with pain in the left mandibular region which had persisted for five days. He reported that he had been in an aircraft and the onset of the pain had occurred suddenly and unexpectedly when it had completed its ascent. On a numerical rating scale, the patient evaluated the intensity of his pain as 8. The pain had ceased for some 5 hours after the plane had landed, only to subsequently return in the form of a localised dull, throbbing toothache with a pain intensity of 6 - 7. Over the next 4 days, the patient had taken 1600 - 2400 mg ibuprofen daily for analgesia since he was unable to obtain immediate dental treatment.
On clinical examination, tooth 36 was was found to be very sensitive to percussion, although
 Fig. 7: Status post repositioning and fixation of the bone flap in the region of tooth 25
Fig. 7: Status post repositioning and fixation of the bone flap in the region of tooth 25
an apparently adequate conservative restoration was in place (Figs. 11, 12). The result of vitality testing of tooth 36 was negative.
A radiographic examination showed an adequately restored dentition in the left mandible (Fig. 13). A single-tooth radiograph of tooth 36 revealed an enlarged periodontal space and a periapical radiolucency in the region of the distal root of tooth 36.
Following the administration of a local anaesthetic and the application of a dental rubber dam, endodontic treatment of tooth 36 was initiated. An access was created and three root canals were exposed (see Fig.). No pus was released from the tooth when the access was created although there was extensive haemorrhaging from both mesial root canal orifices. There was extensive gangrenous decomposition of pulp tissue in the distal root canal.
 Fig. 8: Palatal abscess: showing a palatal swelling that does not extend beyond the midline
Fig. 8: Palatal abscess: showing a palatal swelling that does not extend beyond the midline
The root canals were prepared using nickel-titanium (Ni-Ti) files in accordance with a standard protocol. The tooth was temporarily provided with a treatment filling until it could be definitively filled. On completion of the endodontic course of treatment, the further progress of the patient was normal and free of complications.
Conclusion
The cases outlined above demonstrate the close correlation between exposure to pressure changes and effects on surrounding tissue prior to and during active deployment. None of the patients was considered to be combat-ready for at least one week following dental treatment. My experience shows that there are also likely to be subclinical pathological conditions that require treatment if the need for dental intervention for
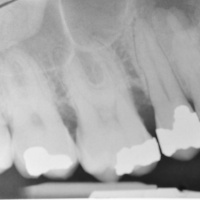 Fig. 9: Radiology image of the lateral maxillary teeth: a periapical translucency can be seen in tooth 14
Fig. 9: Radiology image of the lateral maxillary teeth: a periapical translucency can be seen in tooth 14
personnel posted abroad is to be kept to a minimum. As a rule, all service personnel, and particularly those who are likely to be exposed to changes in pressure, should be examined regularly and as early as possible. Treatment must provide for the restoration of all carious lesions and the elimination of any inflammation. From the dental point of view, patients need to be advised to avoid exposure to pressure changes until all necessary surgical, conservative, and prosthetic procedures have been completed.
Date: 11/12/2014
Source: MCIF 4/14










