
Article: H.M.H.TAYSEIR, M. EL M. OSMAN, A.A.M. HASSAN (SUDAN)
Amputations in Patients Admitted with Diabetic Septic Foot to Wad-Medni Teaching Hospital (2008 – 2009)
Hospital based and general population based data of the burden of diabetic foot disease in Sudan are scanty. Accurate information on the prevalence of the risk factors for diabetic foot ulceration is also much needed, as it is essential for developing and evaluating preventive procedures, public health practices and health care services.
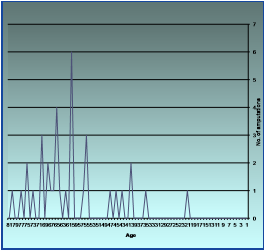 Fig. 6: RISK OF AMPUTATION INCREASES WITH AGE
Abbreviations
Fig. 6: RISK OF AMPUTATION INCREASES WITH AGE
Abbreviations
| D.M. | Diabetes Mellitus |
| DSF | Diabetic Septic Foot |
| ESRF | End Stage Renal failure |
| H/O | History Of |
| JDC | Jabir Abu Aliz Diabetic Center |
| LEAs | Lower Extremity Amputations |
| LOS | Length of Stay |
| MLEAs | Multiple Lower Extremity Amputation |
| NOGs | Non Government Organizations |
| Pt. | Patient |
| RBS | Random Blood Sugar |
| SPSS | Statistical Package Program for Social Science |
| U/S | Ultrasound |
| UT | University of Texas |
Introduction
The prevalence of lower extremity amputation (LEA) is high in Sudan, but the underlying risk factors remain to be defined. This study aims at determine the pattern of amputations in diabetic patients admitted with septic foot and to explore the prevalence rate, types, clinical features and possible risk factors and clinical outcome in diabetic patients with septic foot admitted to Wad-Medani Teaching hospital, Wad-Medani ,Sudan. This is a prospective descriptive cohort study of newly hospitalized, adult diabetic patients with septic foot conducted during theperiod from January 1st 2008 to December 31st 2009 (study period). Detailed clinical data were recorded for each patient, followed by a comprehensive physical examination. Clinical outcome was documented and analyzed using the statistical package program for social science (SPSS).The results were tabulated and presented in percentage forms. A total of 81 patients were studied. Nine patients (11.1%) had grade one, 54 patients (66.7 %) had grade two and 18 patients (22.2 %) had grade three ulceration according to university of Texas(UT) classification system. 46 patients (56.8%) were managed without the need for lower extremity amputation (LEA), 35 patients (43.22%) underwent LEA. 17 patients (20.99 %) underwent major LEA while 18 patients (22.23%) underwent minor LEA. The risk of LEA was significantly associated with the grade of ulceration at presentation, UT staging, other co-morbidities, increasing age and gender. The mortality rate was 3.7%. The outcome of ulceration was determined by the severity and grade of foot ulceration at presentation. Despite a significant proportion of patients having an underlying neuro-ischemic etiology for foot ulceration, the majority healed and the need for LEA did not arise. There was gender difference in risk for undergoing LEA, which was higher in male patients. The risk for LEA also increased with age. The situation is more challenging in developing countries due to limited resources so that more stress should be given to prevention, patient education, and the establishment of multidisciplinary teams in small diabetic units that disseminate and apply the international guidelines on the management of the diabetic foot.
Patients and methods
This is a prospective, descriptive cross sectional hospital based study. It was conducted at Wad Medani teaching hospital, which is a (300) bedded tertiary level hospital receiving referrals from various localities of Al Gezira state and surrounding states. There are five (5) surgical units; each is headed by a consultant, (2– 4) registrars and (8– 12) house officers. There is a daily referral clinic run by a surgical unit. The hospital theatre has four (4) rooms for general surgery and one room for laparoscopic surgery. The study population included all patients (81) admitted to the surgical wards with diabetic septic foot, from January 1st 2008 to December 31st 2009. All patients were consented to participate in the study.
Inclusion criteria
- All patients admitted to surgical ward.
- Aged 18 years and above.
Exclusion criteria
- Patients managed at the outpatient clinic or at home.
- Private Patients.
- Young patients below 18 year of age.
A full detailed history was taken from each patient and a proper systemic examination was performed by the author, together with relevant investigations.
All patients were assessed further for ischemia, neuropathy, grade of ulcer, infection and associated complications (e.g. renal function impairment, sepsis, hypertension…etc.)
Data were collected after obtaining consent from all patients using a pre-designed data collection sheet which was constructed in sections to address different aspects of the problem:
Section (1): Personal data.
Section (2): Diabetes history.
Section (3): Chronic illness history.
Section (4): Investigation.
Section (5): Treatment.
Section (6): Complications.
Section (7): Rehabilitation.
Data collected included age, sex, type/duration of diabetes, cause of ulceration, duration of ulcer, previous history of ulceration, presenting signs & symptoms of ulceration and previous treatment and socio-economic status. Diabetes control was assessed based on the fasting (FBS) & random (RBS) plasma glucose levels. FBS <120mg/dl good, 121-140 mg/dl, fair and >140mg/dl, poor. For RBG values <160mg/dl, good, 160-180mg/dl, fair >180mg/dl, poor.
The examination of the diabetic feet followed the recommendations of the American diabetes association (ADA) which was mentioned in chapter one of this study.
Each patient underwent assessment of the vascular status by manual palpation of femoral, popliteal, dorsalis pedis and posterior tibial arteries to define patency and grade: (a) good volume (b) diminished volume or (c) absent. Neuropathy was quantified assessing vibration sensation using a 128 HTZ tuning fork and a 10g monofilament applied perpendicularly to the plantar aspect of the first toe, the first, third and fifth metatarsal heads, the plantar surface of the heel and dorsum of the foot avoiding any callosities, corn or wound site and graded as normal, diminished or absent. Ankle and knee reflexes were assessed as normal reinforced or absent. Osteomyelitis was determined by radiological examination.
The University of Texas Classification System was used to classify the severity of ulceration at presentation.
The treatment provided covered these aspects:
- Surgical debridement (figure16)
- dressing
- Control of infection
- Control of diabetes
All foot ulcers were photographed at the initial presentation and at each stage of review through the study. Outcome is recorded as: No amputation or LEA defined as loss of any part of the lower limb as major if proximal to tarso-metatarsal joint and minor if distal to this joint.
All collected data were finally entered in the computer using the statistical package program for social science (SPSS).
Objectives
Main objectives
To study the pattern of amputations in diabetic patients admitted with septic foot. +
Specific objectives
To study:
- Prevalence of DSF related amputations.
- Types of DSF related amputations.
- Clinical features of DSF related to amputations.
- Possible risk factors for DSF leading to amputations.
- Relation to age and sex.
- Survival after amputations (peri operative).
- The need for a different approach to deal with the problem of DSF in our community.
- Patient awareness of the role of prevention.
Results
The total number of patients involved in the study was 81. The mean age for the study population was 55.5 years; the majority of patients (71%) had type 2 diabetes mellitus. Most of the patients (83.5%) presented with foot ulcers. Nine patients (11.1%) had grade one, 54 patients (66.7%) had grade two and 18 patients (22.2%) had grade three ulceration. 46 patients (56.8%) were managed without the need for LEA, 35
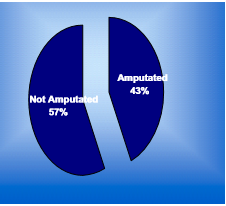 Fig. 1: AMPUTATION RATE AMONG PT. ADDMITTED TO SURGICAL WARDS WITH D.S.F
Fig. 1: AMPUTATION RATE AMONG PT. ADDMITTED TO SURGICAL WARDS WITH D.S.F
patients (43.2%) underwent LEA (Figure: 1). Nearly 21% of patients underwent major LEA while 22.23% of patients underwent minor LEA. The risk of LEA was significantly associated with the grade of ulceration at presentation, UT staging, other co-morbidities, increasing age and male gender (Figure: 6). The mortality rate was 3.7%. Inflicting cause was identified in (40.4%) of the patients. The most commonly affected toe was the big toe in 39.0% of the patients, followed by the second toe in 18.5% of the patients. The plantar aspect of the foot was affected in 42.6% of the patients whereas only the heel was involved in 10% of the patients. Dorsum of the foot was involved in 13.6% of the patients. The mean duration of diabetes among patients who underwent amputation was 16 years. It was recorded that 43.2% of patients had different types of amputations. (Figure 1) 20.99% of the patients had major
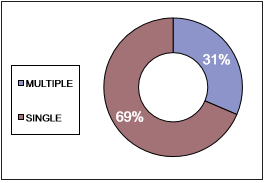 Fig. 2: H/O AMPUTATION INCREASES THE RISK FOR ANOTHER AMPUTATION
Fig. 2: H/O AMPUTATION INCREASES THE RISK FOR ANOTHER AMPUTATION
amputations. Above knee amputations were reported in 6.17% of the patients, below knee amputations and Sym’s amputation represented 12.35% and 2.47% of the patients respectively (Figure 2). It was recorded that 22.23% of the patients had minor amputations. Toe amputation was reported in 8.64% of the patients, Ray’s amputation and trans metatarsal amputations were recorded in 9.88% and 3.71% of the patients respectively. History of lower extremities amputations was present in 13.58% of the patients. This group represented 31% of the amputees (Figure 2). A re-amputation rate of 8% was reported ( Figure 3). The toes were the most commonly amputated in 18.52% of the patients (Ray’s and minor toe
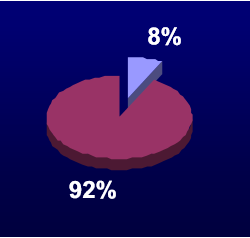 Fig. 3: REAMPUTATIONS
Fig. 3: REAMPUTATIONS
amputations) and accounted for 43% of total amputations (Figure: 4).
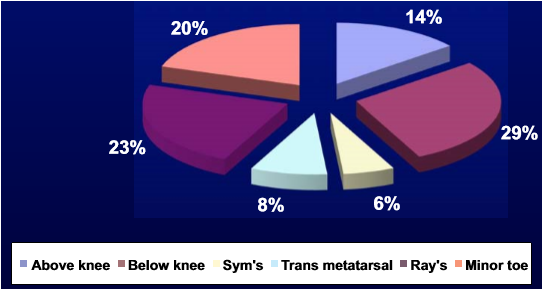 Fig. 4: Types of amputation
Fig. 4: Types of amputation
Gangrene was the commonest indication for amputation (59%), followed by osteomyelitis 23% 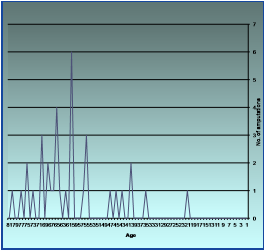 Fig. 6: RISK OF AMPUTATION INCREASES WITH AGE
Fig. 6: RISK OF AMPUTATION INCREASES WITH AGE
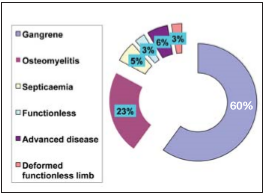 Fig. 5: INDICATIONS FOR AMPUTATIONS
Fig. 5: INDICATIONS FOR AMPUTATIONS
(Figure: 5) The risk for amputation increased with age. Maximum amputations occurred between ages of 54 to 70 years (figure: 6). (table: 1) Anemia was common among admitted patients (27.16%) representing an important risk factor for amputation as 45.71% of the amputees were anemic (Figure: 7) .On the other hand, 72.73% of the anemic subjects were amputated. Few (10.5%) patients had critical limb ischemia as determined by Doppler U/S scan. This was found to be the most significant risk factor for major amputations. There was no association between LEA and poor glycemic control as 45.71% of the amputees were on regular diabetic follow-up (Figure: 8, table 2).This can be explained by the fact that most of the patients have poor diabetic control. It was noted that six out of eight newly discovered diabetics were amputated (75%). Significant number of patients (57%) did not receive foot care advice at the time of diagnosis of diabetes, which is an important preventive measures (Figure: 9). This study recorded that 97% of patients were of low socio-economic class, nevertheless only 14% of them were covered by health insurance!
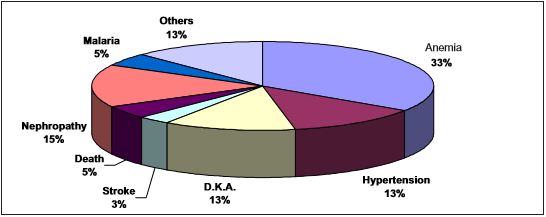 Fig. 7: Common complications associated with D.S.F.
Fig. 7: Common complications associated with D.S.F.
 Tab. 1: Distribution of pt.s into age groups
Tab. 1: Distribution of pt.s into age groups
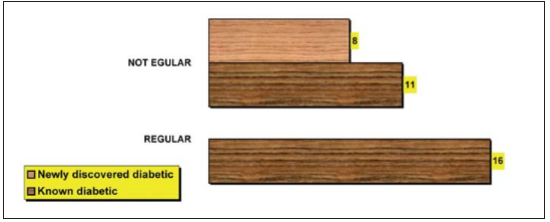 Fig. 8: History of diabetic follows up among amputees
Fig. 8: History of diabetic follows up among amputees
Discussion
Diabetic foot ulceration is the most frequent cause of hospitalization among diabetic patients. LEA, is the most feared and costly consequence of foot ulceration. In this study the majority of patients presented at an advanced stage
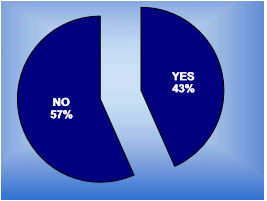 Fig. 9: FOOT CARE ADVICE
Fig. 9: FOOT CARE ADVICE
of foot ulceration with a resultant high amputation rate (43.2%) in agreement with several other studies. Furthermore, male subjects had a greater chance of undergoing LEA than female subjects as shown in other studies. Patients with neuropathy and ischemia were more likely to undergo LEA but neuropathy alone was not independently associated with LEA, as shown in a number of other studies. Analysis showed that beside age, hospital admission was independently associated with LEA. Clearly this is related to more advanced grade and stage of ulceration requiring hospitalization for intravenous antibiotics and surgical intervention leading to LEA. Patients with previous history of limb amputation were at a higher risk for amputation, representing 31% of amputees. Compared to our hospital, Jabir Abualiz Diabetic Centre (JDC), Khartoum reported a lower amputation rate of 38% among patients admitted with diabetic foot according to world diabetes foundation, Sudan project. The majority of patients presented with advanced stage and grade of ulceration reflecting a lack of structure in the health care delivery system of Sudan between primary, secondary and tertiary care units. Attempted home surgery, trust in traditional and faith healers and undetected diabetes further aggravates the problems.
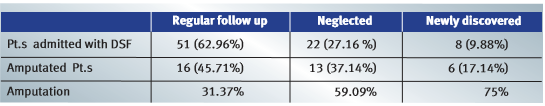 Tab. 2: FOLLOW-UP AND CONTROL OF D.M
Tab. 2: FOLLOW-UP AND CONTROL OF D.M
Moreover, inadequate antibiotic treatment and the use of nonsterile instruments for dressing, results in the growth of multi resistant organisms necessitating hospital admission and surgical intervention. This will also contribute to increase the length of stay (LOS) in the surgical wards, causing additional pressure on the health services. These poor outcomes also reflect the low priority in terms of health spending. Only 2% to 5% of the total household expenditure is spent on health, while the required amount is much higher.3 Most of the patients (97%) come from a low socio-economic back ground and therefore can not meet the demands of treatment (dressing material, drugs, investigations… etc) which are usually required for long periods of time. They need financial support, which they seldom get. Unfortunately, only 14% of them are covered by health insurance which is meant basically to support the poor and needy sections of the society. This issue needs to be addressed by the authorities taking in consideration the serious consequences of neglected D.S.F, the scale and the impact of this problem on the community. The mean duration of diabetes among patients who underwent amputations was 16 years. This explains the increased risk for amputations associated with aging. The peak incidence of amputation occurred at the age of 55 to 75 years. In this study, there was no association between LEA and poor glycemic control as shown in other studies. We noticed that patients with neuropathy underwent LEA independent of poor diabetic control. This reflects
the fact that all these patients had poor glycaemic control. It is of interest that 17.14% of LEAs were performed in persons newly and recently diagnosed as having diabetes. Moreover, six out of eight newly discovered diabetics (75%) underwent a sort of LEA. It would appear, therefore, that some patients presenting with established foot complications of diabetes would not be able to benefit from secondary preventative health care. Anemic patients were at greater risk for amputations as 72.73% of them underwent L.E.A., representing 45.71% of the amputees. Anemia will complicate the ischemic state of the diabetic foot and delays healing, therefore if present, anemia should be corrected immediately. The current study confirms a high amputation rate as a consequence of diabetic foot ulceration in Wad-Medani teaching hospital. The
major deficiency in this study is that it is not population based and represents patients referred to a tertiary care center. However, it has the
 Fig. 12: Typical diabetic foot ulcer caused by high plantar pressures at the third metatarsal head
Fig. 12: Typical diabetic foot ulcer caused by high plantar pressures at the third metatarsal head
advantage of accurate characterization of the stage and severity of foot ulceration with a high follow up rate. Earlier presentation with aggressive and appropriate medical and surgical treatment according to the severity of ulceration can improve morbidity and reduce mortality. This can be achieved by educating health care professionals and patients through education programs and instituting comprehensive multi-disciplinary foot care programs. At the patient level, effective tive foot care advice should be propagated to reduce the burden imposed by diabetic foot complications, particularly in developing countries. The implementation of these measures has led to a 77.8% decrease in amputation rates amongst persons with diabetes in Brazil where ‘Save the Diabetic Foot Project‘ has been implemented. This shows that even in resource-poor countries Strategies can be put in place to improve the outcome of diabetic septic foot without the need for expensive equipment. In parts of India and in Brazil, careful screening of patients, education of the patient and health professionals and the institution of preventive measures
 Fig. 15: Below knee amputation
Fig. 15: Below knee amputation
have been successful in reducing ulceration and amputation rates. These successes are heartwarming and should encourage us. Our ultimate target should be to make available effective preventative foot care and education programs that will work effectively in primary, secondary and tertiary health care settings throughout the country. „We can and should begin to follow the examples set before us. We must not wait till the present situation reaches catastrophic proportions before we begin to act”. A study conducted at Jabir Abu Eliz Diabetic Center (JDC), University of Khartoum, Implemented a system for prediction of lower extremity amputation.7 They used the criteria for wound classification adopted by the International Consensus for the Diabetic Foot to get a reliable grading of the diabetic foot and predict the outcome. These criteria were: the degree of limb ischemia, sensory neuropathy, depth and surface area of the wound, severity of sepsis, and ESRF. Risk factors for diabetic LEA, based on several types of analytic studies, are quite similar to those for foot ulceration. In fact, foot
 Fig. 16: Surgical debridement of D.S.F.
Fig. 16: Surgical debridement of D.S.F.
ulceration itself seems to be a major predisposing risk factor for LEA, preceding approximately 85% of amputations. Most studies indicate that duration of diabetes, level of diabetic control, and various degrees of neuropathy are independent predictors for amputations, as are blood pressure, retinopathy, nephropathy, and peripheral vascular disease. Cigarette smoking is an inconsistent risk factor across a variety of study designs. In their landmark paper, Pecoraro et al determined the causal pathways responsible for LEAs in a series of consecutive male diabetic patients. Using the model established by Rothman, the causal sequence was defined by both compo
nent and sufficient causes. Component causes are risk factors that are insufficient by themselves to cause the outcome of interest (LEA or ulceration) but are required components of a complete causal pathway that is sufficient to produce the outcome. A sufficient cause, therefore, is a constellation or grouping of the minimal number of specific component causes that, in concert with each other, inevitably produce disease. There can be a number of sufficient causes with various combinations of component causes that produce the same outcome. However, removal of any component cause will block the completed pathway to the sufficient cause and thereby prevent disease through this specific pathway. A study conducted in Nigeria reported LEA rate of up to 50% among patients admitted with diabetic septic foot to a tertiary health care center5, while the rate was 27.5% in another study conducted in Pakistan4 (Figure: 12 – 16)
Conclusions
Hospital based and general population based data of the burden of diabetic foot disease in Sudan are scanty. Accurate information on the prevalence of the risk factors for diabetic foot ulceration is also much needed, as it is essential for developing and evaluating preventive procedures, public health practices and health care services. The prevalence and outcome of diabetic foot disease are influenced by genetic factors, cultural factors, and the quality and availability of health care services. Lack of proper health education, knowledge and skills by both patients and health care providers, as regards the care of the diabetic foot, still results in insufficient prevention and management. For many people access to health care is still very limited, with a great number of patients presenting very late to hospital. The low socio-economic status and unsatisfactory diabetic control of many patients are significant contributory factor to the high morbidity and mortality associated with diabetic foot ulcerations. Delayed referrals to secondary and tertiary centers by medical practitioners are also common. Unfortunately, even in tertiary hospitals in Sudan, inadequate facilities and socio-economic burdens also hinder prompt and appropriate treatment. Presently, there are no podiatrists, orthotists or specialized foot clinics. Most tertiary centers are not even equipped for vascular intervention. There are also no facilities for customized footwear, and offloading devices. The inadequacy (or sometimes total lack) of foot care program provisions at primary and secondary health care settings is a considerable barrier to the provision of foot care for patients with diabetes mellitus. This emphasizes the need for the provision of foot care programs, not just at tertiary level, but also at primary and secondary health care levels. To reduce the amputation rate, however, attention should be paid through a multidisciplinary setup to timely referral from the physician, patient education, total contact cast, and appropriate revascularization. The situation is more challenging in developing countries due to limited resources so that more stress should be given to prevention, patient education, and the establishment of multidisciplinary teams in small diabetic units that disseminate and apply the international guidelines on the management of the diabetic foot.
Recommendations
The situation of diabetic foot care in Sudan is not satisfactory, resulting in high LEAs rates with major economic consequences for the patients, their families, and society and have a huge impact on health services. In order to tackle this growing problem we recommend the adoption of the following measures:
- Policy makers should understand the devastating effects caused by diabetic foot problems and the urgent need for an integrated DSF care program in primary, secondary and tertiary health care settings.
- Training health professionals in foot examination techniques and diabetic foot care at health centers and hospitals throughout the country. This leads to the provision of sufficient interested and trained personnel.
- To enhance preventive measures and provide adequate education facilities for people with diabetes and their families. The golden rule: „prevention is better than cure”.
- Introduction and implementation of hospital based specialist multidisciplinary foot care clinics and the addition of orthotists to the team. These teams are to be built up step by step, introducing the various disciplines at different stages
- To establish multidisciplinary care and the integration of work between the orthotists and nurses.
- Expansion of the national health insurance coverage to include and cover the weaker and low socio-economic sections of the society. This service should provide the necessary support for rehabilitation of amputees.
The time has come for a concerted effort to provide foot care programs for patients with diabetes mellitus. Governments, other health control agencies and non-government organizations (NGOs) need to be made aware of the importance and suffering relating to diabetes mellitus and diabetic foot problems, so that proper resources for diabetes education, care and foot care programs can be allocated. A concerted effort must be made towards obtaining nationwide epidemiological data on the burden of diabetic foot disease.
Date: 07/01/2015
Source: MCIF 3/15











